The social contract, an idea derived from political science, has recently come to be used to describe the relationship between the medical profession and the society which it serves.1,2,3,4,5 Medicine's contract with society has always been more implicit than explicit. It functioned reasonably well when both medicine and society were relatively homogeneous, sharing many values. Medicine knew what society expected of both individual physicians and of the profession as a whole. The obligations of physicians necessary to sustain the contract were understood and passed on by respected role models. For its part, society understood what it wanted from those responsible for the care of the sick. Societal obligations were present, but less clear. Society granted physicians status, respect, autonomy in practice, the privilege of self-regulation, and financial rewards on the expectation that physicians would be competent, altruistic, moral, and would address the health care needs of individual patients and society.6 This "arrangement" remains the essence of the social contract.
Professionalism is fundamental to the social contract: society uses the concept of the profession as a means of organizing the delivery of complex services it requires. Professionalism is the basis of the contract and of the expectations of the profession of medicine. Hence, it is important for physicians to understand the origins, evolution, and obligations of professionalism.
Each physician fills 2 roles--that of the healer and of the professional.6 Even before recorded history, mankind required healers. With the development of science, the healer learned to cure.
The professions arose in the guilds and universities of medieval Europe and England. They had little impact on society until science made health care worth purchasing and the industrial revolution provided sufficient resources so that society could afford it. Some means of organizing health care was required and society turned to the preexisting concept of the profession.1,2,3 This occurred in the middle of the 19th century, when licensing laws were passed granting the medical profession a monopoly over the use of its complex and expanding knowledge base, thus establishing the basis of the modern social contract.
Until the mid-20th century, the structure of the health care system evolved slowly: Trust in authority, including medicine, remained high, and the term social contract was not used. Assuming that members of the profession would be altruistic, social scientists looked favorably upon the professions, and medicine's influence on public policy was substantial.2,3 In the 1960s and 1970s, all forms of authority were challenged. Social scientists argued that medicine had abused its monopoly to further its own interests, had self-regulated poorly, and that its organizations were more interested in serving their members than society. In a 1984 book, Paul Starr used the term social contract to describe medicine's relationship to society, stating that it was being renegotiated to cope with the complexities of both modern medicine and contemporary society.1
Although much of it is unwritten, it is possible to outline broadly the terms of the contract by examining both the expectations of the medical profession and those of society.
Societal Expectations of Medicine
The services of the healer. Society's primary expectation is that individuals will receive the services of the healer.6 They want caring and compassionate treatment, with their confidentiality respected and their dignity preserved. Furthermore, they want to retain control of the direction of their own treatment. Medicine must fulfill this role.
Guaranteed competence. Society expects that the profession will ensure the competence of each physician by setting and maintaining standards for education, training, and practice—and by disciplining incompetent, unethical, or unprofessional conduct. The obligation of individual professionals is to maintain their own competence and to participate in the process of self-regulation.
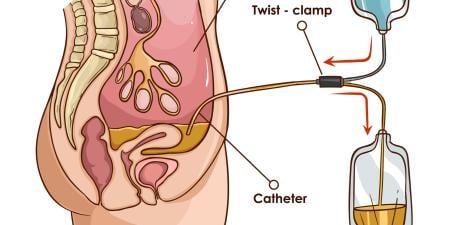
Altruistic service. Physicians are empowered to ask intrusive questions and carry out invasive procedures. For this to be permitted, patients must trust that their physicians will not pursue self-interest but have the patient as their first priority.7 This must not be an open-ended commitment that is incompatible with a healthy physician's lifestyle, but altruism is central to the social contract.
The pervasive nature of conflicts of interest must be recognized and managed by individual physicians if they are to maintain patient trust.8 Professional organizations are also expected to demonstrate altruism, putting the interests of society above their own.9
Morality and integrity. Physicians are expected to demonstrate morality and integrity in their practice, and in their day-to-day lives. Physicians who do not do so will, without question, lose trust, and this will reflect upon the profession as a whole.
Promotion of the public good. Inasmuch as the profession is given a monopoly over the practice of medicine, it is expected that its members will address the problems faced by individual patients and also concern itself with issues of importance to society.
Transparency. Historically, professions carried out their deliberations in a relatively closed manner.10 This is no longer acceptable; it is now expected that public membership in regulatory bodies will be significant and that the establishment and maintenance of standards and policy will be done in consultation with public representatives.
Accountability. For generations, physicians recognized that they were accountable to individual patients, to the public for advice on policy, and to each other for self-regulation. As medicine became more costly, it was inevitable that physicians would become accountable in both economic and political terms.11 These newer levels of accountability are a cause of major tension. A physician's fiduciary duty to patients now comes into conflict with the social purposes of medicine.12 Devoting resources to the care of a single patient inevitably diminishes the resources available for other patients. As the contract evolves, this tension will remain, but medicine's fiduciary duty to individual patients must take priority.
Medicine's Expectations
A contract involves obligations from both parties, so it is reasonable for medicine to expect certain deliverables from society. Recent observers have stated that negotiating for these deliverables is one of the characteristics of a contemporary profession.13 Just as society's trust in physicians is heavily influenced by how it believes the profession is meeting its obligations, an individual physician's trust in society will be influenced by societal actions. There is some evidence that physicians' current dissatisfaction with how society is upholding its part of the contract has less to do with financial issues and more to do with their belief that they have lost both autonomy and respect.14,15
The following are what appear to be medicine's expectations of the contract:
Autonomy. Autonomy is essential to the practice of medicine and has been labeled by some sociologists as the hallmark of a profession.10 Physicians expect to be granted sufficient autonomy to act in the best interests of their patients. Traditionally, autonomy has been incomplete, with customs, codes of ethics, and legal constraints setting the boundaries. In cases where the medical profession feels that it is being restricted in its efforts to act in the best interests of the patient, however, it can legitimately resist unreasonable intrusions into that autonomy. The profession as a whole also requires sufficient autonomy to self-regulate.
Trust. In spite of well-documented failures on the part of some individual physicians and of medicine's organizations, most physicians remain honorable, competent, and devoted to service. They believe that, due to their actions, and the nature of the medical act, they deserve trust. They also believe that the profession, collectively, is trustworthy.
Monopoly. Medicine's monopoly is granted under licensing laws. Because society appears to accept that licensure leads to higher standards, and because of the long education and training required, medicine expects that the monopoly will be maintained.
Status and rewards. The healer has always occupied a respected place in the community, and respect and status have been important nonfinancial rewards associated with being a physician.3 Reasonable financial return is also an expectation of the modern profession.
Self-regulation. Self-regulation has been part of the social contract since the modern professions were organized in the 19th century.1,2,3 Medicine's knowledge base is complex and difficult to understand. Therefore, it has been deemed a benefit to society to allow the profession to regulate itself—within limits—and according to guidelines established by law.
Self-regulation has been questioned in the literature because of medicine's documented failures in this area.10 When failure to self-regulate occurs, some of medicine's autonomy is generally lost, but, thus far, society has decided that it is in its own best interests to allow the profession to set and maintain standards and carry out disciplinary procedures.
Functioning health care system. The transformation of the medical marketplace which resulted from the entry of the state and the corporate sector has greatly transformed the social contract between medicine and society. The values of the marketplace have become dominant, and those of the professional are threatened.2,3,4,5 This situation is unlikely to change, and physicians must function in the systems established by society. However, they have a legitimate right to expect to work in a system which supports, not subverts, the traditional values of the healer and the professional.
Society also has an obligation to provide sufficient resources so that individual physicians can meet their responsibilities. The cost of health care in modern society has led to containment measures which many physicians believe have interfered with their ability to care for patients. A challenge to the profession is participation in negotiations to guarantee a health care system which is adequately funded and value-driven. This is a major concern of physicians.
Summary
A social contract does exist between medicine and society. Because society has chosen to use the concept of the profession as a means of organizing the services of the healer, professionalism has come to serve as the basis of this social contract. What is expected of the physician as healer is largely determined by what it means to be a professional in contemporary society. The medical profession must understand professionalism and the obligations that are necessary to sustain it because these serve as the basis for societal expectations. Those representing society must also understand both the presence and the nature of the contract and society's obligations under it. If both sides understand the expectations of their partners—and their own obligations—the contract will function. If not, tensions will exist and impact on the quality of health care.
References
-
Starr P. The Social Transformation of American Medicine. New York: Basic Books; 1984.
-
Sullivan W. Work and Integrity: The Crisis And Promise Of Professionalism In North America. New York: Harper Collins; 1995.
-
Krause E. Death of the Guilds: Professions, States and the Advance of Capitalism, 1930 to the Present. New Haven: Yale University Press; 1996.
- Cruess SR, Cruess RL. Professionalism: a contract between medicine and society. CMAJ. 2000;162(5):668-669.
- Barondess JA. Medicine and professionalism. Arch Intern Med. 2003;163(2):145-149.
- Cruess RL, Cruess SR. Teaching medicine as a profession in the service of healing. Acad Med. 1997;72(11):941-952.
- Mechanic D. Changing medical organization and the erosion of trust. Milbank Q. 1996;74(2):171-189.
- Schlesinger M. A loss of faith: the sources of reduced political legitimacy for the American medical profession. Milbank Q. 2002;80(2):185-235.
- Pellegrino ED, Relman A. Professional medical associations: ethical and practical guidelines. JAMA. 1999;282(10):1954-1956.
-
Freidson E. Professional dominance: the social structure of medical care. Chicago: Aldine; 1970.
-
Emanuel EJ, Emanuel LL. What is accountability in health care? Ann Intern Med. 1996;124:229-239.
- Bloche MG. Clinical loyalties and the social purposes of medicine. JAMA. 1999;281(3):268-274.
- Wynia MK, Latham SR, Kao AC, Berg JW, Emanuel LL. Medical professionalism in society. N Engl J Med. 1999;341(21):1612-1616.
- Landon BE, Reschovsky J, Blumenthal D. Changes in career satisfaction among primary care and specialist physicians, 1977-2001. JAMA. 2003;289(4):442-449.
- Sibbald B, Bojke C, Gravelle H. National survey of job satisfaction and retirement intentions among general practitioners in England. BMJ. 2003;326(7379):22-24.