Physicians are faced with death in its many varieties throughout their careers. There is an undefined socialization process which takes place during the training years in medical school and post-graduate training. This is necessary to provide the capability of continuing to function with death all around. However, we sometimes feel we are exempt from the emotional toll that death extracts from us. Several events in the past month brought this home to me and I would like to share them with you.
2001 Gets off to a Bad Start
The new year began on a decidedly bad note. On December 30th, a Peace Corps volunteer from one of my Eastern Africa countries was killed in an automobile accident while on holiday in a South African country. Because the death occurred in the area covered by my colleague based in Pretoria, I was spared the necessity to travel there and take charge of the death review that includes an autopsy. I began to make plans to travel to her host country to assist with grief counseling. This was the first death in my area, and I reviewed the protocol developed by the Peace Corps on what to do when a volunteer dies. Unfortunately, this review was prophetic of another tragedy that pulled me into a series of extraordinary events.
One week later, on a rainy Sunday afternoon, I got a call from another of the Eastern Africa countries I cover that a volunteer had been critically injured and was probably dead. Could I come right away? I told them I would come as soon as possible and to have the nurse in the medical office call me as soon as she knew the details. The next available flight was not until Tuesday morning. We forget the luxury of frequent flights between the major cities that we enjoy in the States. The country nurse called back that evening that the volunteer was dead and had been killed by an elephant. "What! An elephant! How did it happen?" "We do not have all the details. You will need to get these when you get here." No one else was injured but a friend observed her death. We went through the details that would need tending to since we all wanted to be able to transfer the body back to the States as soon as possible. The country nurse would arrange for the body to be brought to the capitol and arrange for a host country pathologist to perform an autopsy with me.
The In-country Morgue and Autopsy
On Tuesday morning, we went to the morgue at the public hospital. I had been warned by more experienced medical folks in Eastern Africa that the handling of bodies in this area of the world was quite different. I felt like I had been through enough in thirty years of medical practice that I could handle anything. When I arrived at the morgue, I was surprised to see two to three hundred people arranged around the building. My driver explained that tribal customs required that the family stay with the body until burial. I thought there must be several bodies in the morgue or a very large family. The morgue building consisted of two rooms. One was a body holding area and the other a room for autopsies. The body room was completely full of stacked bodies so the overflow of bodies lined the corridor and the walls of the autopsy room. Some of the bodies were still in their clothing, but others in the clothing they were born with. There was no refrigeration or even air-conditioning. The odor was predictable. All the windows in the autopsy room were wide open for ventilation. I felt like we were center stage in a theater in the round as all the relatives were sitting outside looking in through the windows.
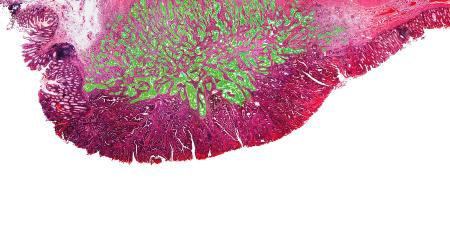
The pathologist was very helpful. He had gone to medical school in Africa but did his post-graduate work in Great Britain. He apologized for the room and bodies but said the laws of the country required a release from the authorities before an autopsy could be done or a body released. I asked if we could drape a sheet over at least the two closest windows. He laughed and said, yes. He agreed that an autopsy on a white body would attract a lot of attention. The autopsy itself was relatively easy. There was no mystery about the cause of death. There was massive blunt trauma to the thorax and abdomen with a flail chest, ruptured left apex of the heart, bilateral hemo-thorax, a huge liver laceration and a ruptured spleen. We both agreed that microscopic examination was not necessary, and he signed off the cause of death to allow us to start the process of getting the body released for transport to the States. Meanwhile, I was charged with writing up the autopsy and getting the facts surrounding the death.
Her college roommate was visiting the volunteer. They had hired a driver and car for an animal safari in one of the National Parks. About 10:00 in the morning, they came across a herd of elephants near the road. They stopped to watch and take pictures. The driver warned them to stay in the car. After some minutes, the elephants started to move away and the two young women got out to get some better photos. After they moved about ten meters toward the elephants, a large female, probably with a young elephant ward, charged. The volunteer was knocked to the ground and the friend and driver related that the elephant then kneeled on the body and rolled back and forth. This is apparently how elephants kill. The story was consistent with the autopsy findings.
After the Emergency, Stopping for Death
The rest of the week was taken up with government releases, securing a hermetically sealed casket for transport, and arranging for transport of the body back to the States. We had several sessions with the staff and other volunteers for grief counseling. I was impressed with how the country personnel handled this very difficult situation. A counselor was sent out from Washington to assist the process. She was very helpful. She asked how I was holding up and of course I said I was fine. She then pushed me to describe the autopsy and surrounding events, and it all came flooding out. Tears are therapeutic, and I was getting therapy. As strong as we feel we are as physicians, situations like this extract their toll. It is ok after the emergent situation to be a human. To grieve. To cry. To be angry. If you ignore this human need, it just builds up inside. I am convinced after all these years that we in the profession do not do enough to support each other. A colleague who takes the time to listen and allow the physician to reduce their guards and talk about feelings provides a very important service.
When I got back to Nairobi, there was an e-mail awaiting me from one of my medical student sons. He is in his third year and currently assigned to the trauma surgery service at a large urban public hospital. He had just experienced his first intra-operative death that happened to be a police officer. He described how he did not even think about it during the surgery. As he left the theater after it was all over, he noticed that the lower part of his scrubs below the gown were blood soaked. He laughed that now he knew why they wore rubber boots. As he headed toward the locker room, he realized that some of the police officers were staring at his legs and the blood. The reality of what he had just been through and the impact on the lives of the officer's family came pouring over him. I felt so helpless on the other side of the world. I wanted so badly to be there to let him vent. I want him to retain his humanity. I can only hope that one of his colleagues will let him vent and provide an atmosphere that it is ok to be vulnerable as a physician.
Questions for Discussion
Dr. Davidson asks us to consider how treating dying patients and witnessing death affect the physician’s physical health and emotional well-being.
- How can physicians tap into social support from colleagues in a culture that expects them not to show signs of weakness or vulnerability?
- How can physicians strike a balance between their own health and well being and that of their patients?