To students and beneficiaries of western biomedicine, the greatest contribution of the ages-old humoral model might seem to be the expressions it provides for describing someone's disposition: he is in good (or bad) humor; or we might even say, "he is phlegmatic." But the humoral theory left more than a linguistic legacy. The group of fourth- and third-century BC physicians known as the Hippocratics who formulated (and more importantly wrote about) their theories, were the first organized group to consider that illness had natural—not supernatural—causes. The significance of this change in attention cannot be overstated for reasons I will return to later. Their notion that 4 bodily fluids—blood, phlegm, yellow bile, and black bile—caused illness persisted for more than 2000 years in the West until the rise of controlled empirical science in the mid-19th century. Humoral medicine's most compelling claim on our attention, though, is its belief that health and its opposite, dis-ease, were due to complex interactions among an individual's 4 internal humors, his lifestyle and habits, and his environment.
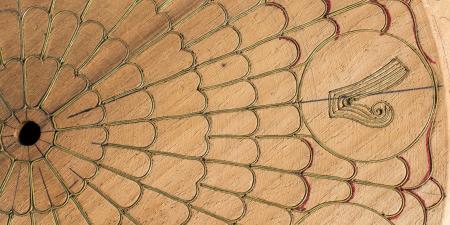
The 4 humors corresponded in their natures to earth, air, fire, and water—the 4 elements of which all matter was composed, according the Greek philosopher Empedocles, a contemporary of Hippocrates. As evident in the diagram above, blood was hot and wet like air; phlegm was cold and wet like water; yellow bile was hot and dry like fire; and black bile was cold and dry like earth. Health consisted in humoral equilibrium. Illness resulted when an excess or a deficiency occurred in one or more or the humors. The disturbance could result from overindulgence in food or drink, too much or too little physical exertion, or changes in the so-called "naturals," ie, the uncontrollable environment and climate. Because of the similarity of the natural elements and humors, certain humors were more likely to become excessive during given seasons of the year. Phlegm increased during the winter, bringing with it bronchitis and pneumonia because phlegm was cold and wet, like the chilly Mediterranean winters.1 In warm, wet spring, hot, wet blood increased, causing dysentery and nose bleeds.2
The physician's task was to diagnose which humor was out of balance; treatment then focused on restoring equilibrium by diet or by reducing the offending, out-of-balance humor by evacuating it. Medicinals were not an important part of Hippocratic treatments. (It was Galen who, in the first century AD, concocted and treated with medicinal herbs and compounds. "Polypharmacy," says history-of-medicine scholar, Robert Hudson, "was Galen's legacy."3)
The all-important Hippocratic breakthrough to which I alluded earlier—the conviction that disease had natural rather than supernatural etiology—forced the Hippocratic physicians to observe their patients closely. Such observation of the patient and his or her physical condition, dietary and exercise habits, and environment were irrelevant when disease was thought to have a supernatural source. In that view, the offending curse or possession was independent of the physical characteristics of those afflicted and their environments. But, for the Hippocratics, diagnosis and treatment began with the knowledge of the patient.
The Hippocratics derived their specific theories about which imbalance caused which symptoms by observing the fluid excretions of sweat, urination, hemorrhage, vomiting, and defecation that coincided with a return to health. They then applied this empirical information to future patients. The Hippocratic Aphorisms attest to close and careful observation of many, many patients: "Persons who have had frequent and severe attacks of swooning, without any manifest cause die suddenly." Hudson explains that this aphorism describes Stokes-Adams syndrome characterized by insufficient cerebral blood flow, victims of which faint frequently and often die suddenly.4 (Today, Stokes-Adams is treated by the implantation of pacemakers.) Another aphorism, Hudson notes, anticipates present-day insurance actuarial tables: "Persons who are naturally very fat are apt to die earlier than those who are slender."5
Their "scientific" observation notwithstanding, the Hippocratics had it all wrong. Though they knew illness had natural causes, they believed that cause to be generalized and in the fluids of the body. The history of medical science is the story of discovering ever more localized cause of illness. That history is familiar, beginning with Vesalius's new anatomy, published in 1543 and based upon his many dissections of human cadavers. Though others had speculated on the role of anatomy in illness, the anatomical idea—that function of the body is related to its structure—took permanent hold after Vesalius. In 1761, the Italian physician Morgagni published the results of his comparisons of organs observed in autopsy with the symptoms those individuals had exhibited before their deaths. His treatise, On the Seats and Causes of Diseases, concluded that sickness and death resulted from changes in the organs.
From there, the localizing of disease narrowed further and further. Bichat and Virchow located disease in tissues and cells in the early and mid-1800s, respectively. Next came the discoveries, starting with Pasteur and followed by Koch, about an external cause for the pathological changes in the cells, tissues, and organs of the body—the germ. By 1900, the germ theory was indisputably established in western medicine.
Throughout the first half of the 20th century, infectious medicine was ruled by the dominance of the germ theory and the spectacular control of germs that antibiotics increasingly afforded. It is humbling, in a way, to note medicine's re-attention to lifestyle and environment in the late 20th and early 21st century. Germs and, now, genes are indeed "master molecules," to be reckoned with in the diagnosis and treatment of illness. Yet, we are coming to realize more and more that the same germ or gene affects different people differently. As the Hippocratics turned their focus away from the supernatural and toward the individual patient, the contemporary physician, too, knows that neither germs nor genes are sacred; successful treatment begins with understanding the individual patient.
References
-
Porter R. The Greatest Benefit to Mankind: A Medical History of Humanity. NY: W.W.Norton & Company; 1997:58.
-
Ibid.
-
Hudson RP. Disease and Its Control: The Shaping of Modern Thought. NY: Praeger; 1987:199.
-
Hudson quotes the Aphorisms on p. 79. His source is Adams F. The Genuine Works of Hippocrates. Vol. 2. NY: William Wood and Company; 1886:208.
-
Hudson (p. 79) from Adams, 204.