Though there is no shortage of studies designed to determine the efficacy of mammography, debate continues in the profession about the effectiveness of routine mammography in reducing mortality from breast cancer.1 Research over the past 10 years, involving more than 500,000 women worldwide, has drawn vastly disparate conclusions. A meta-analysis of 5 Swedish studies found that mammography screening lowered breast cancer mortality by 29 percent. However, an epidemiological study, also from Sweden, found no decrease in mortality for women who were screened.2
The argument for screening is that mammograms can detect smaller tumors with less likelihood of lymph node metastases. There is a cure rate of approximately 90 percent for small tumors (less than 10 mm) without lymph node involvement, and proponents of mammography think that screening will detect many tumors in this size range.3 Critics contend that mammograms can miss up to 20 percent of potential tumors, thus leaving a significant percentage of tested women who believe, falsely, they are tumor-free for at least another year or until they are tested again. Coupled with the risk of anxiety-provoking false positives, this makes screening less effective than is often believed. The result seems to be that research on the efficacy of mammography has generated, "more heat than light for the public."3
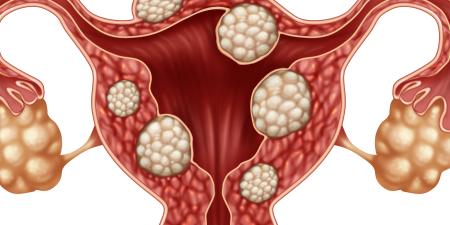
The disputed effectiveness of mammography is only one example of a disagreement in the field of obstetrics and gynecology. Research is still inconclusive on the association between oral contraceptives and cervical cancer.4 And, while physicians agree that tests for the BRCA 1 and 2 genes can identify individuals who have increased risk, they are divided about appropriate use of the test. The BRCA 1 and 2 mutations account for only 5 to 10 percent of breast and ovarian cancer, so negative test results do not mean a woman will not get the disease. On the other side of the argument, for women found to have the mutation, the only known prophylaxis at present is bilateral mastectomy and oophorectomy [5]. Because many women are unwilling to undergo these life-changing surgeries, the value of positive test results is debated.
On issues such as these where there is no professional consensus, physicians face the challenge of how best to inform and advise patients about diagnostic procedures and treatment. When the profession's absence of consensus reaches the mass media, physicians must decide whether it is ethical to share just their own bias about the disputed treatment and, if not, how much information should be shared with patients; when does information confuse more than clarify?
There is a full range of possible patient-physician combinations in decision making, but 3 are obvious. A physician can use his or her medical knowledge and judgment to arrive at a conclusion and present only that recommendation to the patient. Secondly, the physician may choose to tell the patient that a controversy exists, offer his or her medical opinion, and work with the patient in assessing the risks and benefits associated with different decisions. Lastly, a doctor who is treating a highly informed patient may choose to allow the patient to make a decision after the patient has reviewed the relevant literature.
These 3 scenarios present a spectrum of patient decision-making autonomy. In the minds of many, when either patient autonomy or physician paternalism assumes a dominant role in the patient's decision making the other must be a subordinate influence. Prior to the 1970's, most medical decisions were left to physicians; patients and their families were "spared" the difficult choices encountered in medical treatment. The paradigm shift of the last 30 years has created a patient-centered approach to decision making as the profession recognized the shortcomings of the paternalistic approach: the difficulty of determining a patient's best interest, the risk of stereotyping patients based on race or sex, and the lack of an opportunity for patients to consider treatment options in the context of their particular situation.6 Today, physicians present medical options, along with risks and benefits, but often leave the final choices up to patients. Some physicians will go to great lengths to not reveal their preference for a particular treatment option.6
Writing in the Annals of Internal Medicine in 1996, Timothy Quill and Howard Brody suggested ways for physicians to balance physician power with patient choice.6 As a middle ground for patient involvement, Quill and Brody put forth a model they call "enhanced autonomy." The key element of this model is open dialogue between the patient and physician that explores the patient's values and experiences. The authors argue that it is better for a physician to openly admit biases rather than remain artificially neutral. When facing difficult health care decisions, patients will often be emotionally overwhelmed and seek guidance from their physicians. At the same time, patients are more likely to report greater satisfaction with their medical care when they actively participate in decision making.6
Raisa Deber et al took on the task of explaining the patient paradox of need for guidance yet desire to make decisions. In a study reported in Archives of Internal Medicine in 1996, the authors asked more than 400 patients how much physician involvement they would like to have in a variety of medical decisions.7 Looking at the patterns in their results, the authors realized that patients separate medical encounter activities into 2 categories, which the authors called "problem-solving" (PS) and "decision-making" (DM). PS activities are those that require specific expertise and have a single correct solution. Examples of PS activities include making diagnoses and presenting treatment options with the associated risks and benefits. DM activities are those in which patients must choose the acceptability of risks and benefits for their particular situations and make informed treatment decisions.7
Given a series of vignettes, the respondents rated the level of involvement they would wish to have on a 5 point scale, where 1 was the doctor acting alone, and 5 was the patient acting alone. The results confirmed the authors' hypothesis that patients are more willing to have physician control in PS activities than in DM activities.8
Although it would be convenient if doctors could classify all decisions into PS or DM, with the knowledge that patients prefer to be involved in DM choices, most medical decisions have elements of both activities. For example, a physician may wish to order a test for the BRCA 1 and 2 genes, the result of which significantly changes a patient's likelihood of developing breast cancer. Formulating patient risks and benefits are PS skills that are usually performed by physicians. However, the decision of whether or not to perform these genetic tests may fall in the DM category, since each patient must determine whether the potential information gain outweighs the possible anxiety and worry that knowledge of the genetic mutation may bring.
In cases such as mammography, where the profession is not in agreement, the question is: does uncertainty justify less patient involvement in decision making, ie, greater physician paternalism? No simple formula or equation tells a physician when to use his or her own judgment exclusively, when to tell patients about professional disagreement, or how much information to provide. Doctors must make that decision for each patient. Some patients will want to know the details of the medical community's disagreement in making an informed choice. Others may state clearly that they wish to follow the physician's recommendations. It may help physicians to be aware of the PS and DM elements of medical decisions in order to allow patients to participate at appropriate times. As expressed by Quill and Brody, this will require a constant balance between patient autonomy and paternalism.
Questions for Discussion
- How should physicians decide when to tell patients about treatment controversies within the profession? Can you think of circumstances where they would be justified in not informing patients?
- How can physicians decide how much patient involvement to invite without resorting to patient stereotypes based on culture, age, ethnicity, religious beliefs, or educational level?
- As a patient, do you agree with Deber's conclusion that patients prefer to be involved in decision-making but not problem-solving activities?
- Does medical uncertainty justify greater physician paternalism?
References
-
The most recent contribution to the debate came in an April 2003 Lancet article that summarized findings on deaths from breast cancer during 2 twenty-year periods—one before the advent of mammography and one after its advent. Tabar L, Yen MF, Vitak B, et al. Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet. 2003;361:1405-10. Though the authors interpreted their findings to show that "mammography screening is contributing to substantial reductions in breast cancer mortality," cancer prevention experts soon questioned whether the drop in deaths was from early detection through mammography or from advances in treatment. Ross E. Study backs benefits of regular mammograms. Chicago Sun Times. April 25, 2003: 35.
-
Gotzsche PC, Olsen O. Is screening for breast cancer with mammography justifiable? The Lancet. January 8, 2000; 355:129-133.
-
Hornung C. Routine mammography: to screen or not to screen? Law and Bioethics Report: University of Louisville School of Medicine. March 2003: 2(3):6.
- Smith JS, et al. Cervical cancer and use of hormonal contraceptives a systematic review. The Lancet. 2003;361(9364):1159-1167.
-
Bailey R. Warning: bioethics may be hazardous to your health. Reason Magazine. August/September 1999. Accessed April 28, 2003.
- Quill TE, Brody H. Physician recommendations and patient autonomy: finding a balance between physician power and patient choice. Ann Intern Med. 1996;125(9):763-769.
- Deber RB, Kraetschmer N, Irvine J. What role do patients wish to play in treatment decision making. Arch Intern Med. 1996;156(13):1414-1420.
-
Ibid, 1417.