Case
Ms Wannamaker is tired of visiting the emergency department at her community hospital, but on this occasion, her abdominal pain is simply too excruciating to let it go. A working mother of 2, Ms Wannamaker is not apt to let a little stomach pain keep her down. With a sharp wit, she would be quick to tell you about her struggles and accomplishments over her 49 years of life. As Dr. James enters the room, she is happy at the sight of a familiar face and manages to let out a partial smile.
"Hello, Ms Wannamaker. I'm sorry we see each other again under these circumstances. How is your stomach today?"
"It's the same old thing, only worse this time. Still hurts on the right side, right about here," she says, pointing to the right upper quadrant. "And it happened again after I cheated on my diet the other day, you know, at the fast food place."
"How long has the pain been going on?" Dr. James asks.
"About a full day and then some. Plus I feel like I might throw up. Do you think it's related to those gallstones or that colic you talked about last time?"
"It just might be, but let's talk a bit more and then have a look…"
The only abnormal findings in Dr. James's physical examination include a slightly elevated temperature (37.9° C) and pain in the right upper quadrant upon palpation. The relevant blood test results are within normal limits. Dr. James, already aware that Ms Wannamaker's biliary colic might now be acute cholecystitis, orders an ultrasound examination that confirms the diagnosis.
"Ms Wannamaker, I'm sorry to tell you that we'll need to get surgery involved. As I mentioned last time, that gallbladder of yours needs to come out…"
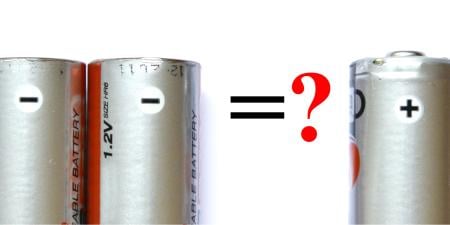
To help his surgery colleagues, Dr. James begins the indicated treatment for acute cholecystitis and preoperative screening, as he often does. He adds an ECG and further blood work (eg, coagulation studies).
Later in the day, Dr. Thorp, the general surgeon, comes to discuss the case with Dr. James and concurs with the diagnosis. Somewhat glibly, Dr. Thorp mentions, "I see you're still ordering those coagulation studies for preoperative screening across the board. You know, we stopped doing that for patients without a suggestive medical history a while ago. For low-risk procedures, it's not worth it. Costs too much and is probably unnecessary."
"I know, I know. But like I said, it would only take 1 adverse event and 1 lawsuit to ruin a career. Someday you'll thank me."
Commentary 1
In this era of evidence-based medicine (EBM), Dr. James seems either very brave or very foolish to recommend a course of action that appears contrary to the best available evidence produced from clinical outcomes research. Certainly, if his decision to order coagulation studies for Ms Wannamaker stems only from force of habit, a decades-old pattern of practice that sends his unthinking hand over the lab order form producing an invariable pattern of checked boxes, his ordering would be indefensible. But Dr. James does have a reason for ordering the test, not one based on clinical research but on a concern regarding legal liability, should a bleeding complication occur with Ms Wannamaker's diathesis having been undetected prior to surgery. His reason is not a scientific one, certainly not evidence-based, but it cannot simply be dismissed out of hand. Rather, one must consider whether his reason for ordering the test is sufficient to outweigh, or "trump," the clinical evidence that suggests a contrary course of action.
Clinical judgment in medicine has traditionally been understood to involve different kinds of reasons and reasoning. The EBM movement has sought to make reasoning from empirical evidence, derived from well-designed clinical research, the preeminent and preferred form of clinical reasoning, initially de-emphasizing all others. But other kinds of medical knowledge exist and remain valuable.1 Experiential knowledge, gained directly from the practice of clinical medicine, provides a direct and personal foundation for clinical practice. Similarly, the understanding of physiologic principles and adherence to a theory of disease and healing form another knowledge base that may influence clinical decisions. Each of these kinds of medical knowledge has strengths and weaknesses when invoked as a warrant for medical decision making. They differ in kind, not in degree, and none, including empirical evidence, necessarily takes precedence over the others. That is, empirical evidence is not necessarily more prescriptive or compelling than clinical experience or pathophysiologic rationale in any particular case. The importance of one over another varies depending on the specifics of the case at hand.2 For instance, low tidal volume ventilation improves outcome in populations of patients with respiratory failure due to acute respiratory distress syndrome (ARDS). But if a particular patient with ARDS develops malignant ventricular arrhythmias each time the tidal volume is reduced and a respiratory acidosis develops, the clinician faces a compelling pathophysiologic reason not to reduce the tidal volumes in that patient despite the imperative of the empirical evidence.
Two other topics, in addition to these 3 different forms of medical knowledge, are important in considering any clinical decision. First, the preferences of the individual patient may be paramount. Even the best empirical evidence can only tell us what treatments are most likely to produce a specific outcome; whether that outcome is relevant to an individual patient—and worth the associated costs or burdens—requires an understanding of that person's goals and values. Second, one must always consider system features: the economic, logistic, legal, and cultural barriers or facilitators of care. The cost, availability, or legality of specific interventions may preclude use even in the setting of strong empirical and experiential evidence in support. For instance, studies that demonstrate that early revascularization with balloon angioplasty improves outcomes in myocardial infarction will be neither helpful nor prescriptive in a community that does not have the resources or personnel to operate a cardiac catheterization lab 24 hours a day. More subtly, the very system of health care delivery, as well as professional and societal values, may appropriately influence decisions regarding the care of individuals.
Expert Judgments
Dr. James, presumably with full knowledge of the relevant research, has decided to act in apparent disregard of that empirical evidence in ordering coagulation studies on Ms Wannamaker. He does so invoking an argument based on the health care delivery system in which he operates. This system feature cannot simply be dismissed because it is not based on empirical evidence; rather it must be examined more carefully to see if it merits relegating that kind of evidence to secondary importance. Certainly Dr. James could support his decision by noting that the US legal system relies on the testimony of experts rather than empirical evidence, that the legal notion of standard of care bears no relationship to evidence-based guidelines, and that juries may award for the plaintiff in spite of evidence-based practice decisions.3 And certainly the cost of a malpractice suit, in personal and financial terms, can be huge. Dr. James, given the system in which he practices medicine, can defend his choice as the most prudent. We might disagree with the relative weighting he assigned to the avoidance of liability, but no appeal to clinical outcomes research will likely be persuasive in changing his mind.
In the current era of evidence-based medicine, knowledge and understanding of the empirical evidence is absolutely necessary for the delivery of quality medical care. But such knowledge is not sufficient for optimal clinical practice. Rather, clinicians must continue to utilize all the forms of knowledge available to them, to solicit patient goals and values, to understand the relevant features of the system in which they practice. They must be able to negotiate these topics in a way that results in the best advice or treatment for an individual patient. Clinical judgment still demands complex reasoning skills. In the absence of sound clinical judgment, thoughtless adherence to the evidence or any other single source of medical knowledge will result in the practice of "cookbook" medicine.
References
- Tonelli MR. The philosophical limits of evidence-based medicine. Acad Med. 1998;73(12):1234-1240.
-
Tonelli MR. Integrating evidence into clinical practice: an alternative to evidence-based approaches. J Eval Clin Pract. (In press).
- Merenstein D. Winners and losers. JAMA. 2004;291(1):15-16.