The concept of measuring a patient's quality of life (QoL) has obvious attractions to clinicians. It seems to be an objective, scientific, and quantitative tool to assist in deciding complex clinical and ethical dilemmas in daily practice. Its use has been promoted in many areas of medicine—from prenatal screening to do-not-resuscitate (DNR) decisions at the end of life.
In this brief article I shall try to sound a health warning. I shall argue that the concept of measuring QoL is fatally flawed, and that, in its current form, it represents a misleading and potentially dangerous avenue for clinical ethics in the context of contemporary social and political pressures.
An Incoherent Concept
Firstly, the concept of measuring QoL is fundamentally incoherent. It is assumed that, by performing an assessment across a series of domains such as material, physical, social, emotional, and productive well-being, a single quantitative score can be obtained.1 But comparing these different aspects of a human life and assigning an equal weight to each is like comparing apples with oranges. How can you rank the inability to walk more than 10 metres on the same scale with the value of an emotionally close and intimate relationship? How about ranking a moderate deficit in attention compared with outstanding musical abilities? The British philosopher Isaiah Berlin emphasised that, within any one life, each of us has competing values, desires, and goals that cannot be ranked against each other—they are incommensurable, to use philosophical jargon.2 The attempt to rank one person's experience or values against another's is fraught with similar difficulty. When we try to compare the value of certain components of well-being for individuals from different cultures, it becomes even more obvious that any attempt at quantitative ranking is futile.
It is particularly absurd to attempt to rank the "goods" of human life in some kind of hierarchy. Is physical well-being more important than emotional well-being? Is creativity more important than perfect sensory functioning? Is it possible to have any consensus within our own society on these issues?
Furthermore, our values change as we go through life. To children, physical pain associated with medical procedures may rank as a greater harm than a future loss of fertility. In adolescence, body image and peer group relationships may dominate one's priorities. To an elderly person, social isolation may be seen as a greater loss than cognitive impairment. The concept of QoL rankings becomes even more problematic when it is used in prenatal screening to predict and put a value on the future life experiences of a fetus that is not yet born.
Each person's experience of living is unique, profoundly complex, constantly evolving, and continually modified by relational and social influences. QoL is not a "thing"—a biological variable which can be measured like plasma sodium or Apgar score.
Misleading
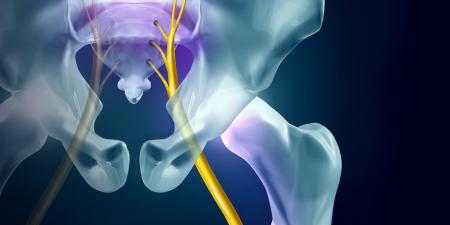
Because the QoL concept is flawed, the use of QoL measures in clinical practice can be misleading. Their use assumes that a physical handicap such as impaired neuromotor function translates automatically into a loss of well-being or satisfaction. Yet many disabled people say that the main problem in their lives is not their functional impairment but social attitudes and political responses to their disability.3 The question, "Are you able to use the local transport system?" could be rephrased, "Has the local transport system been adapted to meet your requirements?" A reduced QoL score may tell us more about social and political attitudes than about an individual's potential for well-being.
Secondly, when applied at the beginning of life, QoL assessment is always based on some probabilistic or statistical element. Can I, as a neonatologist, predict how an extremely preterm baby will feel about life as an adult in 20 years time? It is obvious that this kind of prediction is fraught with assumptions and incalculable factors, and yet these huge uncertainties are obscured in the apparent quantitative precision of QoL measures.
Thirdly, advances in neurobiology that are already starting to enter clinical trials, point to the remarkable plasticity of the developing CNS and brain repair strategies. A poor QoL assessment at the beginning of life tends to promote a pessimistic fatalism amongst clinicians and parents alike. Moreover, a predicted low QoL ignores the effective therapeutic and adaptive strategies that are likely to become available over the next decade and beyond and can easily become, instead a self-fulfilling prophecy.
Underlying Philosophical Assumptions
Although QoL appears to be an objective and "value-free" idea, some philosophers believe that the concept can never be separated from an underlying value system or worldview. The questions which comprise a QoL assessment conceal, but do not eliminate, value judgements about the goals, purposes, and "goods" of human life. By not allowing different goals or ideas to have more weight than others, this system forces a utilitarian point of view. In particular these assessments tend to form an ethical calculus where the "positive value" of one life outweighs the "negative value" of another within a population. By contrast, orthodox Christian and Jewish philosophy emphasise the intrinsic value and dignity of each human life, irrespective of different abilities and capacities. In the Judaeo-Christian worldview the value of human life resides in the stuff of our humanity, as beings made in God's image, with no form of ethical calculus that allows us to compare the ultimate value of one life against that of another or to reject one life in favour of another. This perspective was well summed up by Joseph Pieper, "Love is to say to a person, 'It's good that you exist. It's good that you are in the world.'"4
Dangers
Finally, I believe that QoL measures are dangerous because of their potential for abuse by political, social, and economic agendas within our society. The concept of a low QoL can perpetuate negative prejudices about the experiences of disabled people and may encourage a eugenic desire to eliminate people with any QoL-reducing impairment from our community. In an economic environment with rocketing health care costs, any approach which can reduce on-going health expenditures is attractive. The danger is that QoL subtly shifts the obligation for improving resources for disabled people away from politicians and economists and puts, on clinicians and parents, the responsibility to ensure that people who are likely to be disabled are not brought into the world or, at the very least, that they accept the consequences of their impairments without expecting legal, social, or economic support. I believe that we, as clinicians, should resist that responsibility and give it back to our democratically elected political leaders. Clinicians are called to act with wisdom, care, transparency, and humane judgement in our dealings with patients and parents. We must resist the concept that medicine is a form of social engineering.
Conclusion
Are there any alternatives to the use of current QoL measures? It is obviously important for clinicians to be concerned about the subjective experience and well-being of their patients, and questionnaires and tools designed to assess subjective well-being may be extremely valuable. I think, however, that we should resist the suggestion that subjective experience can be translated into any form of comprehensive assessment of life quality. We may be able to judge whether a treatment is worth giving, but we can never judge whether a life is "worth living." Perhaps, as clinicians, we need to relearn how to say to each of our patients, whatever their degree of disability, "It's good that you exist. It's good that you are in the world."2
References
-
Koot HM. The study of quality of life: concepts and methods. In: Koot HM, Wallender JL, eds. Quality of Life in Child and Adolescent Illness. New York, NY: Taylor & Francis Inc; 2001:3-21.
-
Gray J. Isaiah Berlin. Princeton: Princeton University Press; 1997.
-
Parens E, Asch A. The disability rights critique of prenatal genetic testing. In Parens E, Asch A, eds. Prenatal Testing and Disability Rights. Washington DC, Georgetown University Press; 2000:3-43.
-
Quoted in Meilander G. Bioethics: A Primer for Christians. Grand Rapids, MI Eerdmans; 1996.