I would not give a fig for the simplicity this side of complexity, but I would give my life for the simplicity on the other side of complexity. —Oliver Wendell Holmes
The challenge at the intersection of faith and health is that the experts on either side tend to think that the other is relatively simple, while their field is full of complex nuances. This is true at the bedside and, more dangerously, in Congress. Only a very young physician can avoid humility in the face of the mysteries of healing and death. And only a very young preacher can stand in a pulpit, look at the congregation and not be astonished by the patterns of tragedy, stupidity, and fortune that emerge in any group of more than a dozen human beings. Each knows that health and illness, meaning and incoherence reflect complex interactions and decades of small choices that cannot be explained, much less fixed with a pill or a sermon.
In recent years nearly every health science journal has seen a growing tide of articles linking faith and health in mostly positive ways. Sociologist Ellen Idler reviewed articles resulting from NIH-funded research that included a religion variable and found 1,373 papers published between 1980 and 2002. Found in journals ranging across the health sciences, the religion variable was usually simplistically conceived, while the health issue was the subject of an entire journal and thus deeply nuanced. Religion was usually measured by attendance at worship, or, worse, by denominational affiliation.1
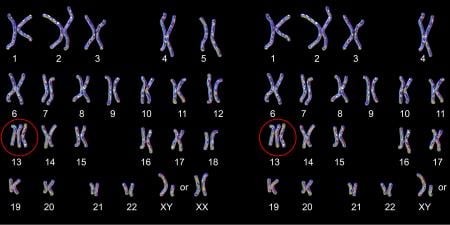
The most common religious traditions have developed over at least 1 or 2 millennia. They have a multicultural literature in which the most well-educated people of their time reflected deeply about the most complex human dilemmas. Those thoughts proved helpful to enough generations to become embedded in ritual and song, and eventually came to be regarded as sacred. (Think of the process as a highly extended peer review.) The result, as one would expect of any living phenomenon, is great complexity within apparent similarity. In the US today there are roughly 4,000 denominations, mostly within the loosely defined boundaries of Christian tradition, but increasingly sharing communities rural and urban with nearly every religious group in the world. This only describes the superficial complexity. When one encounters a single patient, the complexity goes to another scale entirely. If one even begins to probe the layers of coherence that operate within any one modern mind today one is amazed: astrology, Jesus, superstition, electrons, and pharmaceuticals all in one head.
The research corollary of "do no harm" is "do not make me any dumber than I already am." The quickest way to violate that rule is to count something before you understand it. The second quickest way is to ignore something just because you know you don't understand it. From patient to polity, physicians find themselves swimming in a religious sea whether they understand it or not. The first myth to dispel is that there is a necessary separation between science, religion, or politics. Replace it with constant negotiation, some of it at the bedside with the patient and family, other aspects of it in court, as a number of state and federal judges (most recently in Western District of Wisconsin)2 find themselves part of a 300-year effort to identify the appropriate line beyond which is "excessive entanglement" of state with religion. Life is an evolving tangle of meaning and method in which science, religion, and policy are all inextricably involved. The moving edge of science and communications makes the tangle more inevitable as our opportunities for medical and political intervention become enhanced.
The physician's first move into the confluence of faith and health should be one of humility guided by 2 questions that are somewhat novel for those schooled to look for disease. Illness and death are relatively simple, inasmuch as they signal that some vital process has been disrupted. Faith is more like health than it is like disease, so it requires different kinds of questions: First, "What do you think is the cause of your life, of your thriving and vitality?" The Interfaith Health Program, a project of Emory University's Rollins School of Public Health, is conducting research into the "leading causes of life" by interviewing a wide number of individuals. We are finding that the question itself tends toward a pattern of connection, coherence, agency, blessing, and hope.3 People place their struggles—including those of health—in the context of stories of adaptation, resilience, choice, and strength. Religious language is much better with such subjects, but little of the discussion is "religious" in the sense that it talks about extrinsic behavior. It is a language of life that illuminates what the doctor is working with, not just against.
The second question moves to a policy level. "In what ways are religious-social networks and structures assets for health?" Like physicians, policy makers often take 15 minutes to focus on what is wrong at the moment so they tend toward simple, quick, and cheap interventions. In recent years politicians have hoped that religious networks would be willing to replace expensive and inconveniently complicated government services with volunteers and charity. Needless to say the dismantling of government services has moved much more quickly than the research into the actual capacities of nongovernmental entities. In Africa where all philosophies and strategies have been humbled by the deadly weave of AIDS and intractable poverty, leaders are forced to the fundamental question: "What do we have to work with?" And part of the answer is the tangible and intangible assets found in religion. The Africa Religious Health Assets Program conducted by Emory University and the University of Cape Town is finding through case studies and quantitative mapping that faith has multiple proximal and distal affects on which programs of scale could be built once policy makers and program designers think creatively about assets. The findings suggest collaboration with government, not hand-off.
Having argued for humility, let me finish with a plea for intellectual courage. Faith and health are utterly inseparable because both deal with the lifespan developmental processes that inevitably reflect physical, mental, social, and, yes, spiritual, determinants and outcomes. It would be bad science to avoid the complexities of how patterns of coherence and meaning contribute to health outcomes on all scales. And it would be terrible theology to try to contain faith apart from the physical and mental dynamics that physicians deal with daily. We will simply have to learn to talk to each other about what matters most—life.
References
-
Idler E. Religion and Physical Health: Historical Perspectives and Current NIH Research. Address to the International Center for the Integration of Health and Spirituality, April 1, 2003. National Institutes of Health, Washington DC. Available at: http://www.icihs.org/conference/proceedings/day1proceedings/dridler.cfm. Accessed April 16, 2005.
-
Freedom From Religion Foundation, Inc., (and others) v Jim Towey et al., US District Ct, W Dist Wis. June 17, 2004. Memorandum and Order 04-C-381-S. Summary Judgment, January 11, 2005.
-
Gunderson, Gary. The Leading Causes of Life. Address presented at: The Chicago Theological Seminary; April 9, 2004; Chicago.