What is the proper length for family medicine residency training? Well, medical knowledge is exploding, expectations are rising, and there is pressure to incorporate more sophisticated information technology into everyday practice. So we should increase family medicine training from 3 years to 4 years, right? This, in fact, is one of the recommendations of a comprehensive assessment, known as, the Future of Family Medicine, carried out by leading family medicine organizations.1 But before we jump on the bandwagon, let's take a closer look at the field of family medicine and how we train family physicians.
Family physicians are taught to provide comprehensive, continuity of care to patients throughout the life cycle, paying particular attention to biopsychosocial issues. Newborns, sports physicals, deliveries, counseling for depression, caring for hospitalized patients and those in nursing homes, death and dying, we do it all. However, are we the best physicians to provide each of these services? Before we decide the length of family medicine training we should first clearly define what is our unique expertise.
Family medicine, along with pediatrics, internal medicine, and perhaps obstetrics/gynecology are primary care fields. The ability of primary care physicians to evaluate patients with undifferentiated, multiple, often ill-defined complaints distinguishes them from their specialist colleagues. Because family physicians are broadly trained and are sensitive to the psychosocial needs that play such a huge role in primary care, they are uniquely positioned to provide primary care services in ambulatory settings. At the same time, it is hard to argue that family physicians do a better job in inpatient care, labor and delivery, or the operating room that are the domains of internists, obstetricians, and surgeons, respectively. Therefore, family physicians should define themselves as the "specialists" in primary care, while acknowledging the more intensive preparation other specialties receive in areas including inpatient care and labor and delivery.
If we accept the premise endorsed by the Future of Family Medicine report that family medicine should focus on primary care services in ambulatory settings, what are the implications for residency training? I believe The Residency Review Committee for Family Medicine should reduce mandated training in specialty areas including inpatient medicine, obstetrics, and surgery. At the same time we should signal to our residents as well as to the public that we train our residents to be experts or—specialists—at providing primary care in ambulatory settings by emphasizing educational and practice experiences in family health centers.
Reducing training in specialty areas would allow family medicine to cut back its training from 3 years to 2,2 which would be a boon to recruitment efforts. The number of American medical school graduates who select family medicine has plunged over 50 percent in the last 6 years. This reflects not only a lack of clarity regarding the role of family physicians that an emphasis on primary care in the ambulatory setting could address, but also an economic imperative. After all, as politicians are wont to observe, "It's the economy stupid!" As the director for a family medicine training program, I want more and better applicants. So, let's reduce training to 2 years to appeal to students who want to graduate and get paid as full-fledged board certified family physicians 1 year sooner. At the same time, let's create opportunities for family physicians to receive additional postgraduate training in areas of interest including hospitalist services, obstetrics, research, emergency medicine, rural health, and sports medicine, to name a few.
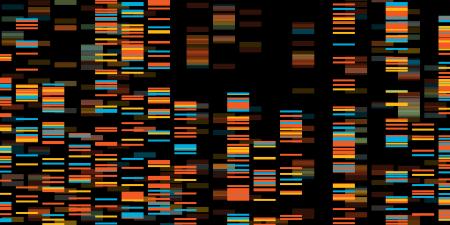
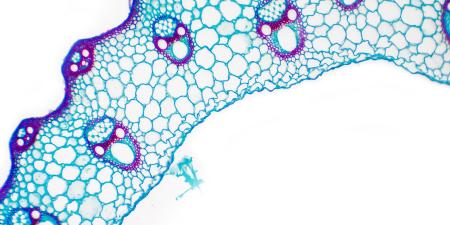
What are the ethical implications of a 2-year training program? Certainly if we were to unleash unprepared physicians solely out of self-interest and a desire to increase our graduates' lifetime earning potential that would be cause for concern. It is my contention, however, that emphasizing primary care in ambulatory settings will help integrate important advances in medical education even in the context of a slimmed-down curriculum. The family health center can naturally incorporate information technology, evidence-based principles, and teaching strategies that address practice-based learning, systems-based practice, and interpersonal and communication core competencies through chart audits, videotaping, and shadowing. The notion of 2-year training is not completely untested. There have been several hybrid medical school/residency programs that graduated participants in 6 years rather than 7 years with no apparent differences in outcomes.3,4,5 Canada already trains family physicians in 2 years, and internal medicine is contemplating changes based on an initial 2-year training period followed by specialization.6,7
We can also consider ethical implications from a societal perspective. Training a physician is subsidized to the tune of close to $100 000 per resident per year by us, the taxpayer, directly through Medicare and indirectly through Graduate Medical Education payments to hospitals. A 2-year primary care training program would allow us to allocate resources to address other pressing societal needs. Retooling family medicine could also lead to a discussion of health workforce issues. We can potentially increase the efficiency of our health care delivery system by clarifying the role of primary care and its relationship to the other medical specialties.
These are turbulent times for health care and medical education. A 2-year family medicine training program emphasizing primary care in the ambulatory setting would position family medicine to respond flexibly and nimbly to the changing paradigms we face.
References
-
Future of Family Medicine. Available at: www.futurefamilymed.org. Accessed January 28, 2005.
- Zweifler J. Why we should reduce family practice training to two years. Acad Med. 2003;78(9):885-887.
- Petrany SM, Crespo R. The accelerated residency program: the Marshall University family practice 9-year experience. Fam Med. 2002;34(9):669-672.
- Stageman JH, Bowman RC, Harrison JD. An accelerated rural training program. J Am Board Fam Pract. 2003;16(2):124-130.
- Galazka SS, Zweig S, Young P. A progress report on accelerated residency programs in family practice. Acad Med. 1996;71(11):1253-1255.
-
The Future of General Internal Medicine. Available at:www.sgim.org/futureofGIMreport.cfm. Accessed January 28,2005.
- Smith LG, Humphrey H, Bordley DR. The future of residents' education in internal medicine. Am J Med. 2004;116(9):648-650.