Introduction
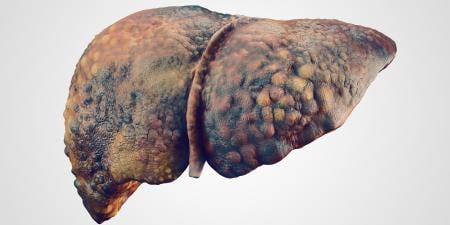
Alcoholic cirrhosis of the liver, which is characterized by severe scarring due to the heavy use of alcohol, is the major cause of end-stage liver disease.1 For those afflicted with cirrhosis, a liver transplant often offers the only possibility for survival. Unfortunately, the demand for liver transplants for both alcoholic cirrhosis and other conditions exceeds the supply. Thus we arrive at an important question, which has both medical and moral dimensions: should those whose end-stage liver disease was caused by alcohol abuse be deprioritized for liver transplantation?2
Medical Considerations
It is largely uncontroversial that limited resources should be allocated where they will do the most good. In triage situations, for example, we try to save those who stand the greatest chance, rather than invest our limited resources in those who are likely to die regardless of the medical care they receive.3 If we are going to try to invest our resources in ways that generate the greatest return, we could ask what medical considerations would be relevant to this assessment. Two jump out as obvious: likelihood of success and life expectancy.4 Starting with likelihood of success, we might reasonably postulate that, all else equal, we should invest our finite resources in cases where the investment is likely to be most effective. For example, imagine that 2 people are in need of a transfusion. Imagine that their blood types are A and B respectively, and that our blood supply consists only of type A blood. In this case, we should obviously transfuse the A patient since the other transfusion would face rejection. Similarly with life expectancy, it should be uncontroversial to postulate that, all else equal, we should invest in those with the longest life expectancy. For example, if we had 1 organ that could be transplanted into a patient with 6 months of life expectancy or into an adolescent patient with 50 years of life expectancy, many would argue that we should transplant to the adolescent.
So, in confronting the issue of whether we should deprioritize alcoholics for liver transplantation, we must ask whether such transplants would be successful and whether alcoholics have a shorter life expectancy than nonalcoholics, all else being equal. If alcoholics score poorly on either of these medical criteria, then we could presumably justify their deprioritization. Regarding likelihood of success, I do not think there are compelling reasons to believe that alcoholics who have been abstinent for at least 6 months would be any riskier as transplant candidates than any other population of patients who need livers. It could be the case that their immune system has been weakened by alcohol consumption, or that they suffer other health-related problems because of their alcohol consumption. However, these cases would have to be investigated individually, and it is clearly inappropriate to assume that alcoholics, as a group, necessarily carry a lower likelihood of success. And if they have health issues that would lower that likelihood, it is not their alcoholism that is (proximately) relevant, but rather the manifestation of other health risks. For this reason, we cannot categorically discriminate against them for their alcoholism, though we could discriminate against them on the grounds of other health problems which they might be more likely to manifest.
Let us now consider life expectancy: do alcoholics who receive transplants have a lower life expectancy than nonalcoholics? Again, there is no necessary reason to think so. Alcoholics might, on average, have shorter life expectancy than nonalcoholics, but this would not provide any reason to discriminate against a particular alcoholic for a transplant. In some cases, the alcoholic can have a longer life expectancy than the nonalcoholic; imagine that the latter has cardiac disease and the former does not. We certainly can discriminate against an individual alcoholic because he or she might have a lower life expectancy, but this is no reason to deprioritize alcoholics as a population. And again, it would not be the alcoholism that was deprioritizing them, but rather their shortened life expectancy. While the latter might have resulted from the former, the alcoholism is still (proximately) irrelevant for the assessment.
While I have thus far maintained that, by medical criteria alone, alcoholics should not be deprioritized, there is at least 1 more feature that we should consider. If the alcoholic is nonreformed (ie, destroyed his liver through alcohol consumption and continues to drink), this is certainly going to be a relevant medical consideration. I do not think that we can deprioritize a reformed alcoholic on medical criteria, though a case might be made against him on moral ones. However, the nonreformed alcoholic is arguably a different case. Remember that our guiding principle thus far has been to invest our limited resources in such a way as to maximize their efficacy. A nonreformed alcoholic might, in theory, destroy a second liver through alcohol consumption and, thus, would suffer a lower life expectancy. In these cases, we would have a medical reason for the deprioritization. However, we should be careful about too hastily invoking this argument against alcoholics. In many cases, an alcoholic has ruined his liver through decades of serious drinking, and it is quite possible that he or she will be unable to redevelop cirrhosis in a second liver before dying of other causes.
Moral Considerations
Thus far, I have tried to argue that a compelling case cannot be made for deprioritization of alcoholics for liver transplantation on medical criteria alone. But certainly there are considerations other than medical ones, namely, moral ones. The central question here is whether alcoholics should be deprioritized on the grounds that their own actions caused their illness, while nonalcoholics might have been afflicted for reasons beyond their control. A related issue is whether failure to deprioritize alcoholics condones their alcohol abuse. First, let's try to make the case for deprioritization on moral grounds. Imagine that there are 2 homeowners, and that each has his or her home destroyed. In 1 case, the homeowner sets his own house on fire and watches it burn down. In the other, the homeowner watches her house be destroyed by a tornado. If we only had enough relief to provide for 1 of the homeowners, whom should we choose? Intuitively, we would fund the second homeowner since her house was destroyed through no fault of her own. This intuition might drive some more general moral principle which says that we must hold individuals accountable for what they do and prioritize those who are blameless over those who are blameworthy. If we accept this principle—and I expect most all of us would—then we might have a reason to deprioritize alcoholics on the grounds that they are to blame for their condition.
But are alcoholics to blame for their condition? Is their case really analogous to the thought experiment proposed above? Arguably not. In the thought experiment, we imagined that 1 homeowner willfully destroyed his own house, and this was supposed to be a thinly veiled allusion to the alcoholic willfully destroying his own liver. But maybe this is not a good analogy; it depends on how we conceive of alcoholism. To put the question simply: does the alcoholic choose to drink? If the answer is yes, then perhaps we can blame him for his cirrhosis. But, if the answer is no, then maybe we cannot. I cannot solve this issue here, but let me gesture toward some avenues of inquiry.
Consider the hypothesis that the alcoholic does not choose to drink; let us call this the "disease concept" of alcoholism.5 This approach could work in either of 2 ways, which I shall label the weak and strong approaches. On the weak approach, the alcoholic chooses to start drinking, but then cannot stop because he is then addicted and lacks volitional control over his actions. This is not to say that he does not know that he is drinking, nor that he fails to engage the means-end reasoning necessary to drink (eg, going to the store to buy alcohol). Rather, the thesis is that he is "unable to do otherwise" because he is in the grasp of an addiction.6 We might compare this weak disease concept of alcoholism with a strong disease concept wherein the alcoholic does not even choose to take the first drink but rather is compelled to start. The compelling could come from genetic predispositions or be due to environmental influences. Or, lest we be accused of genetic or environmental determinism, the compelling might derive from some interaction between genes and environment.
I think that lots of us are likely to find the disease concept of alcoholism (whether weak or strong) unconvincing because of an intuition that, at some level, alcoholics still choose to drink. And, because they choose to drink, they are therefore blameworthy for their cirrhosis. Maybe this is true, and maybe alcoholics do choose to drink. But certainly we cannot reach this conclusion from where we sit without access to the alcoholic's phenomenology. Those who do not suffer from addictions can have great difficulty imagining how crippling an addiction can be, and it might be easy to hasten to the conclusion that cravings, no matter how strong, could nevertheless be resisted. However, this is almost assuredly false. Whether alcoholism is resistible or not is an empirical question, and not one which I claim to be capable of answering. But, insofar as our moral condemnation of alcoholics (and their potential deprioritization for liver transplantation) hinges upon their blameworthiness, it is a question we must engage.
Conclusion
In this short essay, I have tried to highlight some of the medical and moral issues at play in deciding whether alcoholics should be deprioritized for liver transplantations. I argued that medical considerations are not likely to be substantial on a population level insofar as alcoholics are not likely to be riskier transplant cases nor to have lower life expectancies than nonalcoholics. In certain cases, some alcoholics will do poorly in regards to these criteria, though this does not justify deprioritizing them in virtue oftheir alcoholism since they will already be deprioritized on straightforward medical criteria alone. The moral dimensions are harder to evaluate, though the critical question is whether alcoholics are blameworthy for their cirrhosis. If we endorse a disease concept of alcoholism, then they arguably are not blameworthy and should not be subjugated to a deprioritization. However, if we reject the disease concept, then we might legitimately deprioritize them on moral grounds.
References
-
Liver Transplantation. NIH Consensus Statement Online. 1983;4:1-15. Available at: consensus.nih.gov/con/036/036_statement. Accessed August 24, 2005.
- Cohen C, Benjamin M. Alcoholics and liver transplantation. The Ethics and Social Impact Committee of the Transplant and Health Policy Center. JAMA. 1991;265(10):1299-1301.
-
Some philosophers disagree with this position on the grounds that it is unfair to those who just happen to be worse off, and these philosophers might instead argue that we should flip a coin or adopt some other mechanism that would result in an equal chance of everyone being saved. See, for example, Taurek JM. Should the numbers count? Philos Public Aff. 1977;6:293-316.
- Rescher N. The allocation of exotic medical lifesaving therapy. Ethics. 1969;79(3):173-186.
-
See, for example, Jellinek EM. The Disease Concept of Alcoholism. New Haven, Conn: Yale University Press; 1960. For a critical stance and further discussion, see Engs RC, ed. Controversies in the Addictions Field. Dubuque, Iowa: Kendall Hunt; 1990.
-
The "unable to do otherwise" criterion for moral responsibility is a traditional one in moral philosophy, albeit not one without its challenges. The most important of these challenges comes from Frankfurt H. Alternate possibilities and moral responsibility. J Philos. 1969;66:828-839.