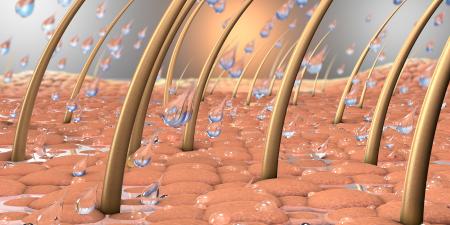
Cutaneous melanoma originates from uncontrolled proliferation of melanocytes, pigment-producing cells within the basal layer of the epidermis, and is the most lethal form of skin cancer due to its propensity to metastasize to distant organs. Despite decreasing incidence of other malignancies due to research and public health efforts, the number of invasive melanoma cases continues to rise, claiming around 8,000 lives in the U.S. annually [1]. The growing burden of this disease underscores the need to educate the public and health care professionals about screening methods.
Unlike tumors of internal organs, melanoma is often readily recognizable thanks to its external location and distinct pigmentation. Thus, many malignant lesions can be identified and excised at an early stage, increasing the likelihood of long-term survival for those with this form of skin cancer. To provide a simple and memorable method for distinguishing a malignant pigmented lesion from a benign nevus, Friedman et al. put forth the ABCD mnemonic in 1985 [2]; however, a fifth letter has recently been added to the screening acronym [3], which now reads as follows:
Asymmetry,
Border irregularity,
Color variegation,
Diameter greater than 6 mm and
Evolution.
The newest criterion, evolution, refers to the tendency of a lesion to change visually over time, e.g., to alter in shape, size or coloration, but the term also encompasses the emergence of associated symptoms like itching or pain. Benign lesions tend to remain stable, so noticeable changes in the characteristics of a nevus should raise suspicion that the lesion is malignant. Using these criteria, patients are encouraged to perform a skin self-examination (SSE) regularly to identify pre-invasive melanoma. This practice is especially important among those possessing one or more risk factors, including:
- Intense sun exposure,
- History of blistering sunburns, especially during childhood,
- Light complexion,
- Presence of typical and atypical nevi,
- Personal history of melanoma or other skin malignancies,
- Family history of melanoma [4].
Robinson and Turrisi recently reported that verbal explanation of the ABCDE criteria and demonstration of SSE techniques significantly improved the ability of patients to correctly identify suspicious lesions [5]—anyone can use a ruler to measure diameter and a magnifying glass to examine coloration and borders of nevi. This study suggests that providing simple instructions for melanoma screening would equip at-risk patients with tools to determine when to seek medical attention and confirms that efforts to educate the public in conducting a SSE would not be in vain.
Furthermore, training in skin cancer screening methods must improve within the medical education curriculum to enable budding physicians to differentiate benign from malignant nevi. An alarming report by Moore et al. indicated that most U.S. medical students feel ill-prepared to conduct proper skin examinations, with only 28.2 percent of students reporting that they felt "somewhat skilled" or "very skilled" in examining a patient for skin cancer and nearly 70 percent agreeing that the skin examination was under-emphasized in their clinical training [6].
Finally, a broadened melanoma awareness campaign is necessary to educate the entire public about screening practices. The campaign must reach members of minority populations who are often neglected due to the low prevalence of malignant nevi among individuals with darker skin. In a recent study from Miami-Dade County [7], the investigators found that people of African and Hispanic descent were more often diagnosed with melanoma at a late stage and exhibited poor survival compared to Caucasians. Thus, it is important that public health officials and health care professionals make an earnest effort to dispel the notion that melanoma is a disease that affects light-skinned individuals only and to teach the ABCDE acronym to all patients.
As suggested by Geller et al. in a recent editorial, achieving a meaningful improvement in melanoma detection at a curable stage will likely require a national initiative to educate physicians and patients about proper skin examination [8]. Indeed, cooperative efforts by the medical and public health communities to teach the ABCDE screening method may be the key to curtailing the discouraging increase in the burden of melanoma.
References
-
American Cancer Society. Detailed Guide: Skin Cancer—Melanoma.Available at: http://www.cancer.org/docroot/CRI/CRI_2_3x.asp?dt=39. Accessed July 13, 2006.
- Friedman RJ, Rigel DS, Kopf AW. Early detection of malignant melanoma: the role of the physician examination and self-examination of the skin. CA Cancer J Clin. 1985;35(3):130-151.
- Abbasi NR, Shaw HM, Rigel DS, et al. Early diagnosis of cutaneous melanoma: revisiting the ABCD criteria. JAMA. 2004;292(22):2771-2776.
-
Schuchter L. Melanoma and nonmelanoma skin cancers. In: Goldman L, Ausiello D, eds. Cecil Textbook of Medicine. 22nd ed. Philadelphia, Pa: W.B. Saunders Company; 2003:1248-1252.
- Robinson JK, Turrisi R. Skills training to learn discrimination of ABCDE criteria by those at risk of developing melanoma. Arch Dermatol. 2006;142(4):447-452.
- Moore MM, Geller AC, Zhang Z, et al. Skin cancer examination teaching in US medical education. Arch Dermatol. 2006;142(4):439-444.
- Hu S, Soza-Vento RM, Parker DF, Kirsner RS. Comparison of stage at diagnosis of melanoma among Hispanic, black, and white patients in Miami-Dade County, Florida. Arch Dermatol. 2006;142(6):704-708.
- Geller AC, Miller DR, Swetter SM, Demierre MF, Gilchrest BA. A call for the development and implementation of a targeted national melanoma screening program. Arch Dermatol. 2006;142(4):504-507.