Case
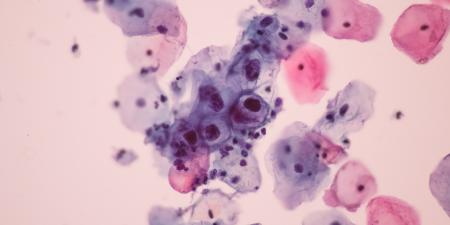
Mrs. Freeman is a lawyer and mother of two daughters. During her morning shower one day, she was surprised to feel a small, hard mass in her left breast. After having a mammogram, she underwent a core biopsy and was diagnosed with a 2-centimeter invasive ductal carcinoma.
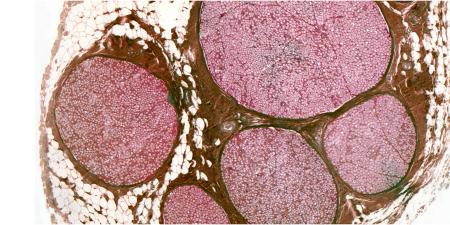
Because Mrs. Freeman is only 34, her physician thought that she might have a genetic mutation that would greatly increase her chance of developing breast cancer. She asked to be tested and was in fact found to express a BRCA1 mutation.
Mrs. Freeman's surgeon, Dr. Hanes, advised that her breast tumor be removed by a lumpectomy. But after learning her BRCA1 status, Mrs. Freeman had become anxious about developing another breast cancer, and elected to undergo bilateral mastectomies. At her first postoperative visit, she seemed noticeably relieved.
"I just couldn't live with the fear of finding another breast lump some day," Mrs. Freeman told Dr. Hanes. "And I've been thinking that I don't want my daughters to live in fear and uncertainty either. I'm going to have them screened for BRCA mutations, too."
"Your daughters are 8 and 10 years old, is that right?" Dr. Hanes asked. "Even if they have the mutation, they wouldn't be at risk for cancer for many years."
"I know," she said, "I just want them to be prepared."
"Well maybe you should at least wait until they are a bit older and can decide for themselves if they want to be screened," Dr. Hanes countered.
"No," Mrs. Freeman answered, "I've made up my mind, and if our insurance won't cover it, I will pay myself to have them tested. They'll be better off knowing their breast cancer status now."
Commentary
Mrs. Freeman, diagnosed with a BRCA1 mutation and a personal history of early-onset breast cancer, is determined to have her two minor daughters (8 and 10 years of age) undergo genetic testing to discover whether either has inherited the mutation. Mrs. Freeman refuses her physician's suggestion to wait until her daughters reach adulthood and can decide on their own whether or not to be tested.
Predictive genetic testing of children for adult-onset diseases like hereditary breast cancer raises two main ethical issues [1]. The first is whether the putative benefits of predictive testing outweigh the risks, and the second is whether parents' requests for this type of testing on their child's behalf should be honored by the physician.
Do the Benefits Outweigh the Risks of Testing?
Predictive testing can sometimes provide medical benefit. Identification of an individual who has a high risk of future disease might lead to disease prevention or diligent screening for early detection and treatment [1]. Several interventions are available to reduce the risk for cancer in women with a BRCA1 mutation. These include early initiation of mammography, breast MRI screening, and prophylactic mastectomy and oophorectomy [2,3]. Although these measures are imperfect and not always acceptable, they do provide a means to reduce the cancer risks facing women with BRCA1 mutations [2-6]. Current practice standards recommend that these women start screening in early adulthood (25-35 years) [7]. As a result, no interventions would be recommended to Mrs. Freeman's daughters at this time, even if either tested positive. If no medical benefit is available to Mrs. Freeman's daughters before adulthood, what would be the benefit of knowing their mutation status now?
Benefits of testing are not all related to health. Psychosocial benefits must also be considered. Knowing their genetic status would reduce the Freeman girls' uncertainty about their risk of breast cancer and allow them and their family to make informed choices for the future, including plans for health care, education, career and reproduction [1].
Psychosocial harms are also possible. A daughter who inherited the mutation might worry about her future health [8]. The mother might develop feelings of guilt or anxiety about her daughter's future. Knowledge of an adverse test result could change the parents' expectations of the child's future in a negative way [1,9,10]. In response to an adverse test result, parents might think of the child as "sick and damaged" or might perceive her as vulnerable and become overly protective of her [1]. Relationships between siblings can also be affected, especially if one has the BRCA1 mutation and the other does not. Predictive testing during childhood might have a lasting impact on the girl's developing self-identity, in either positive or negative ways; integration of her risk status into her developing identity could lead to a loss of self-esteem, or, alternatively, to a sense of empowerment [1,11]. Identification of a deleterious mutation might have negative consequences for the child's future in terms of insurance or employment discrimination [1,9,11].
After considering these potential risks and benefits, most experts have concluded that predictive testing of children for adult-onset diseases is not appropriate unless specific medical interventions are recommended prior to adulthood or the request is voluntary and comes from a competent and informed adolescent [1]. The determination to delay testing until adulthood is based on the speculative nature of the psychological benefits and harms.
Should Parents' Requests for Predictive Testing for their Children be Honored?
This question addresses the right of minors to self-determination. The case of Mrs. Freeman demonstrates the tension between the parents' right to make medical decisions for their children and the children's opportunity to exercise their own decision making in the future.
In general, parents have the authority to make decisions about their children's health care, unless those decisions are obviously harmful [1,12,13]. Because parents are primarily responsible for their children's well-being and know them better than anyone else does, they are permitted to decide what's best for them [1,12,14]. Yet, physicians have obligations to both parents and children [15]. Parents may have their own interests in mind when requesting genetic testing or may be seeking reassurance from a negative test result, so the physician must ensure that parents have considered the consequences of both negative and positive results for the child as well as for the rest of the family [12].
Although parental consent is required to perform testing, the child's assent should be sought as early as age 7, according to the American Academy of Pediatrics (AAP) [15]. Physicians and parents must respect the child's right to dissent [15].
The argument for preserving a minor's right to decide for himself or herself whether or not to undergo testing, i.e., the right to choose in the future "not to know," is supported by the observation that only a fraction of adults at risk for late-onset genetic disease decide to undergo predictive testing [12,14]. Some have argued that letting parents request predictive testing for their children does not reduce the child's future autonomy, because knowledge of one's status provides an opportunity to prepare and adapt for the future [14,16].
Predictive testing can be allowed before adulthood when mature adolescents seek it out [11,17,18]. In such cases, the American Society for Human Genetics (ASHG) and the American College of Medical Genetics (ACMG) recommend assessing the child's competence, obtaining her assent or consent, and ensuring that her decision is voluntary [1]. If the adolescent demonstrates "mature decision-making capacities," the physician should respect her autonomy to decide to undergo testing [17,18].
Deferring testing until late adolescence or adulthood makes it easier for the physician to communicate the test results and their implications for the future to the individual being tested. A young child may not understand the implications of the test results, and it is often unclear who has the responsibility of disclosing the results to this child years later when she is old enough to understand them.
Conclusion
Predictive testing of children involves both potential harms and potential benefits and restricts the child's present and future autonomy in favor of the parents' present autonomy. Professional organizations, such as the ACMG, the ASHG, the AAP, the American Society of Clinical Oncology and the American Medical Association do not recommend testing minors for adult-onset genetic conditions, even in high-risk families, unless there are proven medical benefits to childhood testing [1,15,18-21]. Although physicians should respect the decision of competent adolescents and their families, they have no obligation to provide a service that is not in the best interest of the child. Nevertheless, the concerns of the parents deserve serious consideration and emotional support [22].
In this case, it would be appropriate to refuse genetic testing of Mrs. Freeman's children, on the grounds that they are unlikely to derive benefit from testing at this early age but would benefit from having the opportunity to participate in the decision-making process when they are old enough to do so. Family relationships and well-being should be taken into account when making this decision, however [22]; Dr. Hanes should assure Mrs. Freeman that deferring testing will not compromise her daughters' health. He should also offer her the opportunity to discuss her concerns further, and recognize the fact that she is motivated by the desire to protect her children.
References
- Wilfond BS. Points to consider: ethical, legal, and psychosocial implications of genetic testing in children and adolescents. American Society of Human Genetics Board of Directors, American College of Medical Genetics Board of Directors. Am J Hum Genet. 1995;57(5):1233-1241.
-
Nelson HD, Huffman LH, Fu R, Harris EL; for the US Preventive Services Task Force. Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: systematic evidence review for the US Preventive Services Task Force. Ann Intern Med. 2005;143(5):362-379.
- Calderon-Margalit R, Paltiel O. Prevention of breast cancer in women who carry BRCA1 or BRCA2 mutations: a critical review of the literature. Int J Cancer. 2004;112(3):357-364.
- Oei AL, Massuger LF, Bulten J, Ligtenberg MJ, Hoogerbrugge N, de Hullu JA. Surveillance of women at high risk for hereditary ovarian cancer is inefficient. Br J Cancer. 2006;94(6):814-819.
- Kuhl CK, Schrading S, Leutner CC, et al. Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol. 2005;23(33):8469-8476.
- Wainberg S, Husted J. Utilization of screening and preventive surgery among unaffected carriers of a BRCA1 or BRCA2 gene mutation. Cancer Epidemiol Biomarkers Prev. 2004;13(12):1989-1995.
-
National Comprehensive Cancer Network. Genetic/Familial High-Risk Assessment: Breast and Ovarian. Accessed October 30, 2006.
- Cappelli M, Verma S, Korneluk Y, et al. Psychological and genetic counseling implications for adolescent daughters of mothers with breast cancer. Clin Genet. 2005;67(6):481-491.
-
Cohen CB. Moving away from the Huntington's disease paradigm in the predictive genetic testing of children. In: Clarke A, ed. The Genetic Testing of Children. Oxford, UK: BIOS Scientific Publishers; 1999:133-143.
- Sarangi S, Clarke A. Constructing an account by contrast in counseling for childhood genetic testing. Soc Sci Med. 2002;54(2):295-308.
-
Duncan RE, Delatycki MB. Predictive genetic testing in young people for adult-onset conditions: Where is the empirical evidence? Clin Genet. 2006;69(1):8-16.
- Florencio PS. Genetics, parenting, and children's rights in the twenty-first century. McGill Law J. 2000;45(2):527-558.
- Ross LF. Predictive genetic testing for conditions that present in childhood. Kennedy Inst Ethics J. 2002;12(3):225-244.
-
Duncan RE. Predictive genetic testing in young people: When is it appropriate? J Paediatr Child Health. 2004;40(11):593-595.
- Committee on Bioethics, American Academy of Pediatrics. Informed consent, parental permission, and assent in pediatric practice. Pediatrics. 1995;95(2):314-317.
-
Cohen CB. Wrestling with the future: Should we test children for adult-onset genetic conditions? Kennedy Inst Ethics J. 1998;8(2):111-130.
- Elger BS, Harding TW. Testing adolescents for a hereditary breast cancer gene (BRCA1): respecting their autonomy is in their best interest. Arch Pediatr Adolesc Med. 2000;154(2):113-119.
-
Nelson RM, Botkjin JR, Kodish ED; for the American Academy of Pediatrics Committee on Bioethics. Ethical issues with genetic testing in pediatrics. Pediatrics. 2001;107(6):1451-1455.
- American Society of Clinical Oncology. American Society of Clinical Oncology policy statement update: genetic testing for cancer susceptibility. J Clin Oncol. 2003;21(12):2397-2406.
- Borry P, Stultiens L, Nys H, Cassiman JJ, Dierickx K. Presymptomatic and predictive genetic testing in minors: a systematic review of guidelines and position papers. Clin Genet. 2006;70(5):374-381.
-
Opinion 2.138 Genetic Testing of Children. American Medical Association. Code of Medical Ethics 2008-2009 Edition. Chicago, IL: American Medical Association; 2008:57-58.
-
Donchin A. Autonomy and interdependence: quandaries in genetic decision making. In: Stoljar N, MacKenzie C, eds. Relational Autonomy: Feminist Perspectives on Autonomy, Agency, and the Social Self. New York, NY: Oxford University Press; 2000:236-258.