Case
"I've been feeling miserable lately, and I haven't been able to eat much at all," Mr. Brooks said, wincing as he shifted on the exam table.
"Well, end-stage colon cancer is a pretty nasty disease," Dr. Winston, his primary care physician of 15 years, replied softly. "And I understand from your chart that the masses in your liver and lungs haven't gotten any smaller since your last round of chemo."
"That's right. And the last drug we tried was the only standard option left, which might be a good thing, since I'm getting pretty tired of all of the awful side effects. My oncologist, Dr. Lin, really wants me to try one more drug, and I think I'm going to do it. I guess he's in charge of this study. He told me it's called a phase 1 trial. He said this drug has worked really well in mice and that it might work well for me too."
"Hmmm, well I don't know much about experimental cancer treatments, but phase 1 studies are very new and often have more benefit for future patients than for study participants," Dr. Winston cautioned.
"Honestly doc, I hate to sound selfish, but at this point I'm not really thinking about helping other people. I just want to feel better, and Dr. Lin said that this is my best shot. Joining the study sounds like a good idea, right?"
Commentary
How should Dr. Winston respond to his ailing patient, Mr. Brooks? This patient is asking a seemingly simple but actually a very challenging question: "Joining the study sounds like a good idea, right?" The inexorable natural history of advanced colon cancer, the fundamental human need for hope, and the complexity of finding the right balance between honesty and optimism in the patient-doctor relationship all make this situation difficult for both Mr. Brooks and for Dr. Winston. The ethical differences between the goals of scientific research and the goals of patient care provide the keys to understanding this case.
Scientific Research
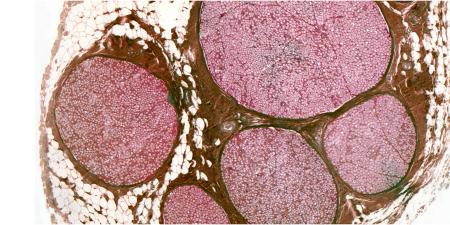
On the scientific research side, Mr. Brooks has been invited (and perhaps even encouraged by Dr. Lin) to enroll in a phase 1 research trial. Traditionally, phase 1 protocols have the identification of toxicity and tolerability parameters as their primary objectives. Such trials typically investigate pharmaceutical agents that are being administered to human research subjects for the first time with the aim of establishing "maximum tolerable dose," often with little or no therapeutic benefit expected for research participants. The stereotypical profile of phase 1 protocols is that they are high risk for study subjects without likely benefit. But recent meta-analyses of phase 1 clinical oncology trials may be telling a different story. The level of risk experienced by cancer patients taking part in phase 1 trials may be trending downward, due in part to the targeted and less-toxic nature of newer cancer drugs and to increased attention to the safety of clinical research [1]. Further, some phase 1 oncology studies have demonstrated that participants' quality of life improved as a result of their research experience compared with the alternative of receiving only supportive care [2]. Finally and importantly, enrolling in phase 1 studies should not necessarily preclude the possibility of a patient's receiving symptom management or palliative care simultaneously [3].
Potential Conflicts of Goals
In the thin description of this case, there is little information about Dr. Lin, the oncologist, or the study that is being considered. Dr. Lin is probably the principal investigator of the clinical trial, and he may be encouraging, if not trying to persuade, Mr. Brooks to enroll. Dr. Lin may have more than one motivation for doing so: he may want to both help this patient and advance scientific knowledge. Some may consider having multiple motives a conflict of interest [4], but we do not. There are many circumstances in which individuals have more than one motivation for any particular action. As Mr. Brooks' oncologist, Dr. Lin has an ethical duty to promote his patient's best interests. As a researcher, he has an interest in promoting scientific advancement (and perhaps his career) by enrolling research subjects and overseeing the study. These two roles and sets of goals are not necessarily in conflict—depending on what is known already about the study drug, the possibility of benefit for Mr. Brooks and the moral integrity of Dr. Lin. More often than not, these two goals live in an ethically acceptable co-existence and tension [5,6].
Mr. Brooks' goals seem fairly evident. He does not seem to be in denial about the seriousness of his illness, but like many patients with advanced cancer he remains hopeful that modern medicine can still help him. In general, his goals seem to include a better quality of life through symptom management. He recounts that he has been feeling miserable and weary and unable to eat, all probably due to the progress of his colon cancer and the side effects of medications. In his own words, "I just want to feel better." His goals at this time do not include helping future cancer patients.
Dr. Winston, in preparing to advise Mr. Brooks as his primary care physician, may have at least two sets of goals, one related to his patient and the other related to Dr. Lin. If Dr. Winston operates out of an "enhanced autonomy" model of the patient-physician relationship [7], he will be aiming to engage Mr. Brooks in a conversation that leads to an exchange of information and ideas, a clarification of Mr. Brooks' values and goals, and a sharing of power and influence that serves Mr. Brooks' best interests. Regarding Dr. Lin, Dr. Winston may want to appear at least collegial by refraining from any frank expression of disagreement with Dr. Lin's recommendation, if indeed he has some hesitancy or disagreement with Dr. Lin's promotion of the phase 1 study.
Within the context of the above-noted actual and possibly conflicting goals, and that of an "enhanced autonomy" partnership and relationship with Mr. Brooks, how should Dr. Winston respond to his patient's assertion and question, "Joining the study sounds like a good idea, right?"
Answering the Question
Dr. Winston should begin with assisting Mr. Brooks' understanding of the general processes of human research and the meaning of the different phases of research trials (i.e., phase 1, phase 2, etc.). Helpful resources would include the Journal of the American Medical Association Patient Pages titled, "Cancer Clinical Trials" [8], and "Participating in Medical Research Studies" [9]. A potentially relevant note from the "Cancer Trials" page, depending on Mr. Brooks' financial situation, is that, "Health insurance may not cover all the costs associated with participating in a clinical trial" [8]. Further, Dr. Winston should explain the role of palliative care and symptom management and encourage Mr. Brooks to ask Dr. Lin whether participants in the phase 1 study can use palliative care simultaneously. The Journal of the American Medical Association Patient Page on "Palliative Care" [10] may be helpful for this part of the conversation.
Dr. Winston should encourage Mr. Brooks to be a full and assertive participant in the informed consent process related to the phase 1 study, including asking any and all questions related to the study. Mr. Brooks should be counseled to read the informed consent form carefully, with special attention to the sections on information about the research and its risks and discomforts. For example, it would be relevant to Mr. Brooks' daily routine if he will need to travel to an academic center and spend a few hours each day over many days to receive an infusion of the experimental agent. Also, with the goal of making Mr. Brooks a better-informed potential research subject, it may be possible to find out if he would be among the very first patients to receive the phase 1 drug and whether he could talk to someone who has already participated in or completed the research study.
In the end, the decision to enroll in the phase 1 study must belong to Mr. Brooks, as he weighs a complex set of projected burdens, benefits and trade-offs. Nevertheless, Dr. Winston has an ethical responsibility to advise, counsel and inform his patient to the best of his ability. One of Dr. Winston's goals, as he answers his patient's question, is to help him avoid therapeutic misconception (conflating research with clinical care) and therapeutic mis-estimation (underestimating risk, overestimating benefit or both), while not interfering with Mr. Brooks' therapeutic optimism (hoping for the best personal outcome) [11]. Dr. Winston should not attempt to erode the trust that Mr. Brooks seems to have in Dr. Lin. The proper balance between honesty and optimism in this case requires that Dr. Winston confront his dilemma and answer the simple question with a clear answer [12]. We believe that his answer should be: "It sounds like a good idea to me, and I hope it does help you. If it doesn't, at least you will be helping others in the future."
References
- Roberts TG Jr, Goulart BH, Squitieri L, et al. Trends in the risks and benefits to patients with cancer participating in phase 1 clinical trials. JAMA. 2004;292(17):2130-2140.
- Agrawal M, Emanuel EJ. Ethics of phase 1 oncology studies: reexamining the arguments and data. JAMA. 2003;290(8):1075-1082.
-
Casarett DJ, Karlawish JH, Henry MI, Hirschman KB. Must patients with advanced cancer choose between a Phase I trial and hospice? Cancer. 2002;95(7):1601-1604.
- Morin K, Rakatansky H, Riddick FA Jr, et al. Managing conflicts of interest in the conduct of clinical trials. JAMA. 2002;287(1):78-84.
- Miller M. Phase I cancer trials: a collusion of misunderstanding. Hastings Cent Rep. 2000;30(4):34-43.
- Helft PR. Necessary collusion: prognostic communication with advanced cancer patients. J Clin Oncol. 2005;23(13):3146-3150.
- Quill TE, Brody H. Physician recommendations and patient autonomy: finding a balance between physician power and patient choice. Ann Intern Med. 1996;125(9):763-769.
-
Parmet S, Lynm C, Glass RM. JAMA patient page. Cancer clinical trials. JAMA. 2004;291(22):2778.
-
Pace B, Lynm C, Glass RM. JAMA patient page. Participating in medical research studies. JAMA. 2001;285(5):686.
-
Stevens LM, Lynm C, Glass RM. JAMA patient page. Palliative care. JAMA. 2006;296(11):1428.
- Horng S, Grady C. Misunderstanding in clinical research: distinguishing therapeutic misconception, therapeutic misestimation, and therapeutic optimism. IRB. 2003;25(1):11-16.
-
Kodish E, Post SG. Oncology and hope. J Clin Oncol. 1995;13:1817.