Background
Cervical cancer is an international problem. Worldwide, more than 500,000 women are diagnosed with cervical cancer each year. By the end of 2006, 10,000 new cases will be diagnosed and nearly 4,000 women will die of cervical cancer in the United States alone.
Epidemiologic studies published in 1999 determined that 99.7 percent of cervical carcinomas expressed DNA from the human papillomavirus (HPV) [1]. HPV is a circular double-stranded DNA virus that infects both cutaneous and mucosal epithelia. More than 100 HPV genotypes have been identified and categorized as either high-risk or low-risk relative to their association with the development of anogenital carcinoma. Human papillomavirus is the most common sexually transmitted disease in the United States; over the span of a lifetime, women and men have an 80-percent chance of being infected. The high-risk subtypes, HPV-16 and HPV-18, are believed to account for 70 percent of all cervical cancers, 50 to 60 percent of moderate to severe dysplasia (CIN II-III) and 25 percent of mild dysplasia (CIN I). Subtypes HPV-6 and HPV-11 are low-risk and account for 90 percent of genital warts (condyloma acuminata) and 10 percent of mild dysplasia.
Introduction of the Pap test in 1928 resulted in a dramatic reduction in the incidence of cervical cancer in the U.S. Despite the effectiveness of this screening modality, however, the incidence of cervical cancer has reached a plateau and is no longer declining. The newest approach in cervical cancer prevention is not a new screening technique but the prevention of the HPV infection through a vaccine. The primary public health goals of the HPV vaccine are to reduce the incidence of HPV-related dysplasia (CIN I, II and III) and cervical cancer.
Vaccine development
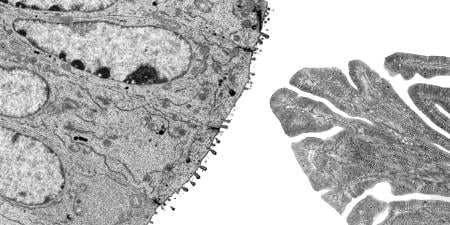
The HPV vaccine is composed of self-assembled virus-like particles (VLPs) that form when a specific HPV protein is produced by microbial organisms through a fermentation process. These VLPs closely resemble native HPV particles and act as the antigen that evokes the production of HPV-neutralizing antibodies in the human body. The vaccine does not contain DNA and is therefore considered to be noninfectious. Nor does the vaccine contain RNA, mercury, antibiotics or egg products.
To date, there are two primary vaccines developed against the human papillomavirus. Gardasil, developed by Merck, is the only current Food and Drug Administration (FDA)-approved vaccine [2]. It is a quadrivalent recombinant vaccine that spurs production of antibodies against HPV subtypes 6, 11, 16 and 18. The efficacy of Gardasil was established in four placebo-controlled, double-blind, randomized phase 2 and 3 clinical trials [2-4]. A bivalent vaccine known as Cervarix designed to be effective against HPV-16 and HPV-18 has been produced by GlaxoSmithKline and is awaiting FDA approval.
Administration
The federal Advisory Committee on Immunization Practices (ACIP), the American College of Obstetricians and Gynecologists (ACOG), and the Society of Gynecologic Oncologists (SGO) have all issued formal recommendations favoring vaccination against HPV [5,6]. The vaccine should be offered to all women aged 9-26 years. Vaccination requires three separate intramuscular injections given on day 1, month 2 and month 6. The vaccine is most effective when administered prior to the onset of sexual activity, but should also be given to women who have a history of abnormal Pap test results, cervical dysplasia, genital warts or positive test results for high-risk HPV. It is believed that these women can benefit from protection against subtypes other than those by which they have been previously infected. Although the vaccine's efficacy has not yet been formally established in immunocompromised patients, both ACOG and SGO state that this population should not be excluded from receiving the vaccine and that it should be offered to immunocompromised women in the 9-26 age range.
The HPV vaccine has been categorized by the FDA as category B in its pregnancy risk classification, meaning that there is not enough information about it to determine whether it poses a risk to the fetus. Until more is known, the vaccine should not be administered to women who know they are pregnant. If a dose is given during pregnancy, the remaining dose(s) should not be administered until after delivery. Vaccination during lactation, however, is considered safe and appropriate.
Post-vaccination surveillance
It is imperative that clinicians educate patients about the HPV vaccine. The vaccine is not intended as a treatment for pre-existing HPV infection or HPV-related disease. Neither of the currently developed vaccines protects against all subtypes of the virus. It is estimated that 30 percent of cervical cancers are due to infections with other, non-HPV-16 or HPV-18 high-risk subtypes. Furthermore, vaccination does not negate the need for screening. The current consensus guidelines recommend initiating screening within 3 years of first sexual intercourse or by age 21. Women under 30 should have Pap tests every 1-2 years, and women 30 years or older should have the test every 2-3 years as long as there is no cytologic abnormality and high-risk HPV is not identified. The guidelines should be followed regardless of the woman's vaccination status.
The future of the HPV vaccine
Vaccination against the human papillomavirus is an exciting advancement in the war against cancer. This achievement deserves great respect, but it should be approached with thoughtful acknowledgment of the many questions still unanswered [5,7]. One of the larger unknowns is the length of time that the HPV vaccine provides protection against the target subtypes. It may or may not be necessary to administer booster doses of the vaccine throughout a woman's lifetime. The regional and global impact of the vaccine has yet to be determined. The true efficacy of the vaccine is going to be limited by barriers such as cost, access and compliance—the same factors that have impeded the success of cervical cancer screening. Other challenges that remain include determining the utility of the vaccine in immunocompromised patients and its efficacy in men or in women over the age of 26.
References
- Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12-19.
-
Merck and Company. Prescribing Information for Gardasil. Accessed December 4, 2006.
- Villa LL, Costa RL, Petta CA, et al. Prophylactic quadrivalent human papillomavirus (type 6, 11, 16 and 18) L1 virus-like particle vaccine in young women: a randomized double-blind placebo-controlled multicentre phase II efficacy trial. Lancet Oncol. 2005;6(5):271-278.
-
Skjeldestad FE. Prophylactic quadrivalent human papillomavirus (HPV) (Types 6, 11, 16, 18) L1 virus-like particle (Gardasil) reduces cervical intraepithelial neoplasia 2/3 risk. Paper presented at: 43rd Annual Meeting of Infectious Diseases Society of America; October 2005; San Francisco, Calif.
- Society of Gynecologic Oncologists Education Resource Panel Writing Group, Collins Y, Einstein MH, Gostout BS, et al. Cervical cancer prevention in the era of prophylactic vaccines: a preview for gynecologic oncologists. Gynecol Oncol. 2006;102(3):552-562.
-
ACOG releases HPV vaccine recommendations for ob-gyns [press release]. Washington, DC: The American College of Obstetricians and Gynecologists; August 8, 2006. Accessed December 4, 2006.
- Bosch X, Harper D. Prevention strategies of cervical cancer in the HPV vaccine era. Gynecol Oncol. 2006;103(1):21-24.