Case
Mr. Roberts was admitted to the University Medical Center with heart failure. He was well known to the staff, having had quadruple bypass surgery 10 years prior when he was 55. He had been a frequent visitor to the cardiology and surgery service with various heart complications since then. After a long night of tests and consultations, the cardiology team diagnosed Mr. Roberts with end-stage heart failure. Due to his past medical history, he was deemed to be ineligible for a heart transplant. Visibly distressed by the news, Mr. Roberts, his hands tightly clasping his wife's, asked the attending physician about his prognosis. In his current condition, he was told, he probably had a month to live. "Come on doc, there must be something you can do." The attending physician told Mr. Roberts he would consult with his colleague, Dr. Jones, to see whether there were any treatment alternatives.
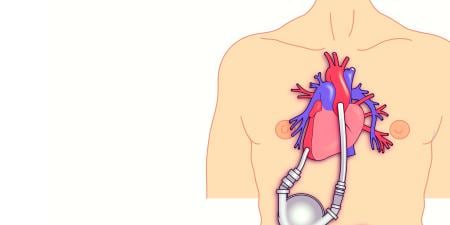
Dr. Jones, an eminent cardiac surgeon at the medical center, had been preoccupied with transplants and machines since his medical school days. Although he had performed numerous heart surgeries in his 25 years of practice, the goal of creating a cardiac device that would eliminate the problems of rejection or failure had long been in his dreams. For the past 20 years, he had been developing an artificial heart in collaboration with its manufacturer, Hipprotech. In the past year the FDA approved the device for a clinical trial with humans, and 10 months ago they implanted one in a patient to much fanfare.
Although the implant occurred without incident, the patient sustained several embolic strokes and died after two months. The autopsy had shown a thrombus within the artificial heart, a problem thought to have been resolved in developing the device. After deliberating, Dr. Jones's group had decided to press ahead with the trial and to collect more data from the next eligible patient to determine whether the clotting problem was device-based or due to the patient, as well as to gather more data about the implant.
They could not decide, however, whether to disclose the clotting problem to the next patient. It was not part of the informed consent protocol, but some of Dr. Jones's colleagues argued that the problem might be in the device. They adjourned the meeting without a consensus. At that point, the cardiology service paged Dr. Jones with the news of a new candidate for the trial. Driving in to the hospital, he was excited about continuing his research. On arrival, he found that the patient's file was already on his desk. Eager to familiarize himself with the profile before talking to the patient and family about joining the trial, he immediately flipped open the folder. To his surprise, the patient was one that he had operated on several times in the past decade: Mr. Roberts.
Commentary
This case illustrates a number of ethical risks:
- Mr. Roberts knows that with optimal therapy he probably has a month or less to live.
- An artificial heart (AH), a cutting-edge technology in early clinical trial, may be an alternative.
- The principal investigator for an experimental device is a surgeon who is deeply and emotionally committed to the success of the device.
- The principal investigator has been Mr. Roberts' surgeon in the past.
- The research team has not decided whether to reveal information acquired thus far in the trial to Mr. Roberts.
Informed Consent
A physician is ethically and legally bound to obtain informed consent to treat a patient. The patient needs enough information to balance the benefits of treatment against its risks. The more invasive or dangerous the intervention, the greater the risk and, consequently, the greater the duty to inform. In human research risks may be greater than anticipated, and the benefits, only speculative. Moreover, the history of human experimentation includes many abuses of human rights. For a number of reasons then, there is a heightened ethical duty to obtain valid informed consent from research subjects [1,2].
What might Mr. Roberts not realize about the AH? While it may pump efficiently, it can't reverse the consequences of chronic congestive heart failure (CHF). Chronic CHF is a systemic disease that can irreversibly damage the liver, kidneys, lungs and other organs. His postoperative care may be compromised, increasing the risk of complications. For example, it's possible that stroke-threatening clots might again form in the AH. With chronic CHF, Mr. Roberts might not tolerate prophylactic anticoagulation treatment without cerebral, gastrointestinal or pulmonary bleeding.
The chance of Mr. Roberts' living longer comes at a price—the risk of suffering and dying in an intensive care unit. Patients like Mr. Roberts who know they are close to death are sometimes unable to make fully rational assessments of their options. This may limit their ability to provide fully informed consent [3]. (Note that Mr. Roberts would be a patient-subject. For simplicity I will use the terms "patient" and "research subject" interchangeably.) Mr. Roberts may understand, but fear of death can evoke denial. He may not appreciate that he could himself experience a negative outcome [4]. It is ethically imperative for Dr. Jones to try to evoke both Mr. Roberts' understanding and appreciation. A person who not only understood but could identify with the risks, benefits and alternatives might well reject the AH in favor of hospice.
Divergence of Goals
If Mr. Roberts enrolls in the AH trial he will encounter Dr. Jones in the changed role of clinical investigator. While sharing the hope that Mr. Roberts will benefit from the device, Dr. Jones's primary goal is to learn whether the AH can be an option for future patients with terminal heart failure. Although Mr. Roberts may wish to help future patients, his primary goal is to avoid dying of heart failure. Because he is accustomed to thinking of Dr. Jones as his physician, he is at particular risk for therapeutic misconception, the erroneous assumption that the AH is actually innovative therapy. Dr. Jones must make a clear distinction between treatment and research, both in goals and promises [3,5].
Conflicts of Interest
That physicians and researchers bring conflicts of interest to their work is inevitable and must be accommodated [3,6,7]. The first step is to recognize that the conflict exists. If an investigator stands to profit financially from the outcome of a study, the conflict can be addressed ideally by ensuring complete financial detachment. The conflict is more subtle when an investigator is so passionately committed to the success of the trial that he loses objectivity. In our case the only person to have received the implant died in two months. Dr. Jones's optimism has yet to be justified, but were he inadvertently to transfer that optimism to Mr. Roberts, it could distort the latter's ability to judge the risks and benefits of participating in the research. A few trials have provided subjects with an independent patient advocate, a knowledgeable third party committed exclusively to the interests of the research subject [8]. Absent a patient advocate, the primary physician or some other knowledgeable designate must act as a consent intermediary, identifying and redressing any lack of objectivity on the part of the principal investigator.
Updating the Consent Form
The consent form, approved by the hospital's institutional review board (IRB), reflects information known at the time of board approval. In one important case the courts chose not to require continuous updating of consent forms with evolving experience [9]. Nonetheless, IRBs that follow FDA guidelines periodically review consent forms to ensure that they reflect new data such as serious adverse events that might be related to the study device and that might materially affect risk-benefit deliberations [2]. While the legal requirement to update the consent form may be ambiguous, the ethical obligation to do so is clear. In this case, the consent form should be changed to reflect that clots and strokes have occurred, information surely relevant to Mr. Roberts' deliberations.
Withdrawing from the study
Patients often decide to become research subjects because of the possibility that the modality under investigation will offer a better outcome than conventional therapy. They are told that they may withdraw from the study at any time, without causing bias on the part of physicians toward their future care [1]. What would that mean for Mr. Roberts? His native heart will have been excised. As his candidacy has already been rejected, the AH can't be a bridge to transplantation; it is destination therapy. And since there is no possibility of reverting to conventional therapy, "withdrawing from the study"—turning off the AH—could only mean certain and immediate death. Mr. Roberts must understand that once he has the AH there is no turning back.
How does one die with an artificial heart? Were the clinical trial to succeed, a new techno-ethical question would arise. Mr. Roberts may well suffer complications to which a biological heart would succumb, but, barring technical failure, the AH will pump until it is turned off. Death by cardiopulmonary criteria won't occur; waiting for brain death can make dying seem interminable. Both legal and ethical consensus support the right to refuse unwanted care, including life-sustaining therapy [10]. Because he may become incapable of making that demand, it is essential for Mr. Roberts to appoint a health care proxy to act in his place. Mr. Roberts needs to explain to both Dr. Jones and the proxy the circumstances under which he would no longer want to live. Should that point be reached, the proxy would be obligated to ask Dr. Jones to deactivate the AH, and Dr. Jones would have to comply.
Conclusion
With increasing regularity we are called upon to evaluate sophisticated medical technology for treating the most desperately ill patients. Meeting that task will require heightened ethical vigilance in studying innovative devices like an artificial heart and in recruiting patients like Mr. Roberts who are terminally ill.
References
-
Emanuel EJ, Wendler D, Grady C. What makes clinical research ethical? JAMA. 2000;283(20):2701-2711.
-
US Food and Drug Administration. Guidance for Institutional Review Boards and Clinical Investigators—1998 Update—A Guide to Informed Consent. Available at: http://www.fda.gov/oc/ohrt/irbs/informedconsent.html. Accessed January 6, 2007.
- Luce JM, Cook DJ, Martin TR, et al, and the American Thoracic Society. The ethical conduct of clinical research involving critically ill patients in the United States and Canada. Am J Respir Crit Care Med. 2004;170(12):1375-1384.
-
Grisso T, Appelbaum PS. Comparison of standards for assessing patients' capabilities to make treatment decisions. Am J Psychiatry.1995;152:1033-1037.
- Bamberg M, Budwig N. Therapeutic misconceptions: when the voices of caring and research are misconstrued as the voice of curing. Ethics Behav. 1992;2(3):165-184.
-
National Institutes of Health. Financial conflicts of interest and research objectivity: issues for investigators and institutional review boards. Release date: June 5, 2000. Available at: http://grants.nih.gov/grants/guide/notice-files/NOT-OD-00-040.html. Accessed January 6, 2007.
- Levinsky NG. Nonfinancial conflicts of interest in research. N Eng J Med. 2002;347(10):759-761.
- Morreim EH, Webb GE, Gordon HL, et al. Innovation in human research protection: the AbioCor artificial heart trial. Am J Bioethics. 2006;6(5):W6-W16.
-
Goodman v United States. 298 F3d 1048 (9th Cir 2002).
- Meisel A. Legal myths about terminating life support. Arch Intern Med. 1991;151(8):1497-1502.