Case
Mr. Stone had been experiencing cardiac problems, ranging from chronic hypertension to cardiomyopathy, for about 10 years when he was diagnosed with heart failure and was told that he would need a heart transplant. With a heart not forthcoming in the near future, Mr. Stone's long-time cardiologist, Dr. Holmes, suggested the possibility of inserting a left-ventricular assist device (LVAD) as a bridging strategy while they waited for a suitable donor to become available. Mr. Stone readily agreed to the idea. At 53 and a mechanic by trade, he told Dr. Holmes that he would do anything to relieve the burden he was currently placing on his wife by being unable to work and asked that the LVAD implantation be done as soon as possible. Dr. Holmes asked Mr. Stone if he had changed his advanced directives since his last surgery: "No doc, I still got the DNR order in there. I don't want to be a burden if it comes to that." Satisfied, Dr. Holmes called the hospital and scheduled the surgery.
On the appointed day, Mr. Stone arrived at the hospital for the surgery, his wife, Martha, at his side. As he was being wheeled to the operating theatre, Mr. Stone gave his wife a quick peck on the cheek: "Don't worry, dear. I'll be back in a jiffy. Dr. Holmes will look after me." The operation itself appeared to be another routine procedure for Dr. Holmes. After closing up the last skin wound, he checked Mr. Stone's cardiac function. On finding that it had improved as expected, he went off to scrub down, leaving his nurse aide, Mary, to take Mr. Stone to the recovery room. As he was washing his arms, Mary rushed in.
"Dr. Holmes, Mr. Stone just had a seizure."
"Call neurology, Mary. I'll be there right away."
Anti-convulsant treatment stabilized Mr. Stone's condition and he was kept in the intensive care unit. Although he regained consciousness a few days after the surgery, Mr. Stone developed complications with pneumonia and was placed on a mechanical ventilator, forcing him to stay in the ICU.
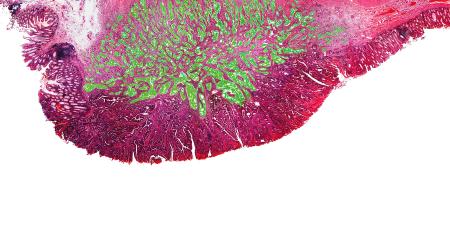
The pneumonia failed to resolve in the following weeks. On consultation with the respiratory service, Dr. Holmes discovered that Mr. Stone's lung parenchyma had been irreversibly damaged and it looked like his condition would not improve much. This was bad news; as a member of the hospital transplant committee, he knew very well that this would make Mr. Stone ineligible for a heart transplant.
Entering Mr. Stone's room, Dr. Holmes moved up close to the bed so that Mr. Stone could hear him better. "Mr. Stone, I am afraid that there are some complications to your case." Mr. Stone listened, and, apart from a few labored breaths on the ventilator as Dr. Holmes mentioned his loss of eligibility, he remained unemotional.
After Dr. Holmes finished, Mr. Stone shifted, and, motioning Dr. Holmes up close so he could whisper to him, Mr. Stone breathed: "You and I both know I'll be stuck like this for the rest of my life. I don't want to. This will blow our savings and I want Martha to get on with her life. Can you turn off the machine in my chest and let me be?"
Commentary 1
Death is a natural event. Every life on earth will have a beginning and an end. Thanks to astounding advances in medicine during the past half-century, health has improved for many. For some, the moment of death can be postponed by technological interventions, but the interventions may not bring back independence or former quality of life. Unfortunately, death has been transformed into a blame-seeking pathology. When someone dies there must be a mistake by an offender.
This mind-set is propagated among the lay public as well as among physicians and is fueled both by our health care system, which rewards the use of more interventions [1], and by our legal system, which punishes physicians who dare to do less than the latest tests—although fear of such reprisals tends to be greatly exaggerated. The inevitable result is that many dying people undergo procedures that they would not have chosen had the procedures and their ramifications been explained clearly—and understood—allowing them to make rational decisions [2].
The foregoing case does not present a true ethical dilemma; the patient had advanced heart disease that could not be improved by medication. After careful discussion with Dr. Holmes, Mr. Stone agreed to have a LVAD inserted as a bridge to a cardiac transplant. He was placed on the ventilator because of a postoperative irreversible lung disease that rendered him ineligible for a heart transplant. The fact that the patient was only 53 years old made an imminent death more tragic but did not alter the medical facts. He asked for his LVAD to be stopped and he wanted to discontinue all efforts to keep him alive by technical means [3].
The implanting of devices in terminally ill cardiac patients has proliferated enormously over the past 10 years to the extent that the majority of dying cardiac patients receive one or more devices before saying their final goodbyes [4]. This habit derives from a couple of sources: physicians' applying recommendations from studies to patients who may or may not be similar to the patients in the study and, secondly, from patients' own preferences. Less influential in the clinical decision making are complications and failure rates of these devices and whether they interfere with the natural process of dying. It is as though inserting such devices in the dying has become the rite of passage before the death of a cardiac patient [5].
Informed refusal of treatment
Usually, left ventricular assist devices are employed as a bridge to heart transplant [6]. It follows that they should be discontinued once one is no longer a candidate for transplant. Unfortunately the decision is not that easy; recent research suggests that a significant number of patients with advanced cardiomyopathy show a reduction in heart size and improvement in left ventricular function after receiving these devices [7]. This recent data must be shared with the patient and a recommendation made about whether to keep the device for a certain period of time before discontinuation. Of course the ultimate decision will depend upon the nature of the original consent and upon a sincere discussion with the patient about the recent clinical findings. It must be emphasized that the decision either to persist with a treatment or discontinue it and bear the consequences rests with the patient; this is the doctrine of informed refusal of treatment. It is particularly applicable if the initial consent was for transient use of the device [8].
Physicians often are tempted to accept treatment burdens on behalf of their vulnerable patients and to act paternalistically, as if "the doctor knows best." This is wrong; the impulse must be resisted at all times. It is the sacred duty of the treating physician to fulfill the patient's expressed wishes [9]. Doctors have to learn to see through their patients' eyes [10] and understand that they are fellow human beings whose wishes must be honored and obeyed so long as they are not making irrational decisions prompted by dementia, pharmacologically altered mental states, depression or feelings of being unwanted.
Furthermore, advance care planning should be instigated by the primary care physician [11] and should address conditions of irreversibility when death is near and unavoidable. These conditions can be associated with states of unawareness, such as deep coma, advanced dementia or permanent vegetative state [12], dependence on machines, or eligibility for hospice care. The decision makers must determine when and how to use or withhold cardiopulmonary resuscitation (CPR), life-sustaining machines, antibiotics and blood substitutes, and artificial feeding and hydration [13].
Documents that outline the use or nonuse of life-sustaining treatment are widely available. One such document has been developed by Project GRACE and is available at no cost [14]. The patient can indicate decisions about specific interventions on the document after learning more about each procedure and the risks and benefits associated with its use. To leave these weighty decisions in the hands of lawyers or other parties who speak in vague legal jargon about the heroic, terminal and irreversible ignores the patient's right to make his own choices. As an example, patients with advanced but not terminal dementia who had complicating, but potentially reversible, pneumonia—patients who stated that they wanted to die peacefully—ended up receiving aggressive treatment despite having signed such a legal document [15].
To let a person die by allowing nature to take its course is legally, morally and ethically right and, in the case under discussion, desirable. By contrast, to prolong a patient's suffering despite his request is morally and ethically reprehensible and should not be condoned [16]. For Mr. Stone, the left ventricular assist device and the ventilator only postpone his moment of dying; the intervention was initiated in the hope that he would recover lung function. The ventilator failed to achieve its desired effect, so Mr. Stone can no longer be a candidate for a heart transplant, and the treatment should be discontinued. Understandably, it is easier on the treating physician and the family not to initiate a certain treatment than to withdraw it, especially in this case where the device is implanted inside the body. Ethically, however, there is no difference between the acts of withholding and discontinuing life-sustaining treatment when a competent patient has requested it [17,18].
Medicine was meant to be a loving, caring and compassionate profession [19]. It upholds the primacy of the patient's own wishes. The basic principles of medical ethics remain those of beneficence, nonmaleficence and justice. Beneficence means that the physicians have an obligation to further their patients' interests and welfare. Nonmaleficence dictates that they do no harm and minimize risks to their patients. Justice implies that there is fairness in distributing access to care and services across all patients without discrimination.
Where is nonmaleficence when, through modern medicine, we enslave an unwilling patient while we intervene aggressively in a terminal, irreversible condition? We render an otherwise peaceful death harsh. We may even be denying a spouse a decent life or a grandchild the opportunity to go to college by persisting with a futile, expensive medical intervention [20]. To die on somebody else's terms when you have clearly stated your choices is an unfortunate consequence of modern medicine [21].
References
-
Starfield B. Is US health really the best in the world? JAMA. 2000;284(4):483-485.
- Gillick M. The high costs of dying. A way out. Arch Intern Med. 1994;154(19):2134-2137.
-
Carrese JA. Refusal of care: patients' well-being and physicians' ethical obligations. "But Doctor, I want to go home." JAMA.2006;296(6):691-695.
- Basta LL. End-of-life and other ethical issues related to pacemaker and defibrillator use in the elderly. Am J Geriat Cardiol. 2006;15(2):114-117.
-
Wellens FL. How long will the heart still beat? Tex Heart Inst J.2005;32(2):126-129.
- Madigan JD, Barbone A, Choudrhi AF, et al. Time course of reverse remodeling of the left ventricle during support with a left ventricular assist device. J Thorac Cardiovasc Surg. 2001;121(5):902-908.
- Rose EA, Gelijns AC, Moskowitz AJ, et al. Long-term mechanical left ventricular assistance for end-stage heart failure. N Engl J Med. 2001;345(20):1435-1443.
-
Schloendorff v Society of New York Hospital, 211 NY 125, 105 NE 92 (1914).
- Charon R. The patient-physician relationship. Narrative medicine: a model for empathy, reflection, profession, and trust. JAMA. 2001;286(15):1897-1902.
- Larson DG, Tobin DR. End-of-life conversations: evolving practice and theory. JAMA. 2000;284(12):1573-1578.
- Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. 2000;284(8):1021-1027.
-
Multi-Society Task Force on PVS, American Academy of Neurology. Medical aspects of permanent vegetative state, part 2. N Engl J Med.1994;330:1572-1579.
- Pasman HRW, The BA, Onwuteaka-Phillipsen BD, van der Wal G, Ribbe MW. Feeding nursing home patients with severe dementia: a qualitative study. J Adv Nurs. 2003;42(3):304-311.
-
Basta LL, McIntosh HD. Project GRACE (Guidelines for Resuscitation And Care at the End-of-life). Clinical Cardiology. 2000;23. Available at: http://www.projectgrace.org/. Accessed December 5, 2006.
-
Hickey DP. The disutility of advance directives: we know the problems, but are there solutions? J Health Law. 2003;36(3):455-473.
-
Snyder L, Leffler C, for the Ethics and Human Rights Committee. American College of Physicians. Ethics manual. 5th ed. Ann Intern Med. 2005;142:560-582.
- Berger JT. The ethics of deactivating implanted cardioverter defibrillators. Ann Intern Med. 2005;142(8):631-634.
-
Opinion 2.20 Withholding or Withdrawing Life-Sustaining Medical Treatment. American Medical Association. Code of Medical Ethics 2008-2009 Edition. Chicago, IL: American Medical Association; 2008:82-101.
- Verghese A. The calling. N Engl J Med. 2005;352(18):1844-1846.
-
Basta LL. Life and Death on Your Own Terms. Amherst, NY: Prometheus Books; 2001:211-230.
- Callahan D. Necessity, futility, and the good society. J Am Geriatr Soc. 1994;42(8):866-867.