Case
"Dr. Peterson, it's been a while." Lifting his head up from a plate of stuffed mushrooms, Dr. Peterson eyed a familiar face—Dr. Kelly. Although the two had been friends since the very first day of medical school, the residency match had assigned them to lives on opposite coasts; Dr. Peterson in internal medicine in New York; Dr. Kelly in radiology in Los Angeles, and they had lost contact. Indeed, one motivation to attend this medical school reunion was to finally catch up with each other.
"It has been a long time, hasn't it? I really should have gotten here earlier, but our practice just opened a new clinic and I had to stay late, what with everyone cashing in on that coupon we placed in the paper. Here's our new business card."
Eyeing the card, Dr. Peterson noticed the bold letters: "Kelly Health-E-Scan: Full Body Imaging."
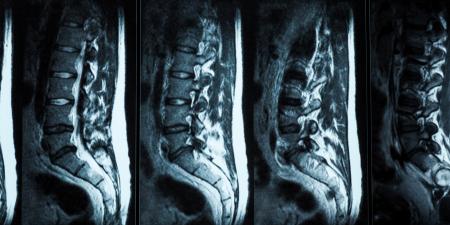
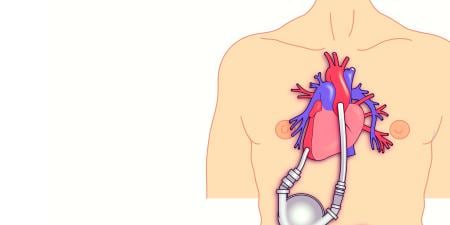
"Our radiology group is creating a straight-to-the-public, full-body scan clinic. We have CT and MRI facilities in the office. We can see potential tumors and calcifications before they become symptomatic. Surveying the community around our practice, we found a sizable interest in such a service, and voila!"
It appeared that Dr. Kelly's famous showmanship had not waned. But Peterson, ever the debater, retorted immediately.
"It does look snazzy, but don't you think that it's rather costly to do scans just on a whim? What about all those false positives? You could put patients through so much unnecessary grief."
"We don't just scan any guy off the street," Kelly replied. "We have it all thought out; we make sure that the patient is at risk before we scan them. Our radiologists go over the results thoroughly with them and send a report to their primary care physicians. There will always be benign findings in every setup; I think it's better to do these scans early and potentially save people from the blocked artery or a brain tumor. If the technology is there and a market for it exists from the patients, I don't see why we shouldn't allow patients to take their health care into their own hands. It doesn't do them any harm. Come on, it's the ultimate public health initiative; giving the patient the latest and greatest to stop them taking up a hospital bed 10 years down the line!"
Commentary
While the American health care system leads the world in many aspects of medical innovation and advanced medical technologies, it also suffers from serious problems that form the context for any discussion of this scenario. The problems include, most notably, high costs that are still increasing and a growing number of people who are uninsured. More than 45 million Americans do not have health insurance, due, at least in part, to a lack of affordability. For those who do have coverage, indecipherable layers of complexity and restrictions prevail over personal choice.
On the one hand, drawbacks of the current U.S. health insurance system can be traced historically to the interposition of employers between individuals and access to insurance, as well as to complex government mandates and other multifactorial influences outside the patient-physician construct. On the other hand, virtually every country, regardless of the fundamental structure of its health care system and the degree of government regulation, is struggling to control costs while grappling with limitations in access to modern medical advances. Needless to say, there is no simple solution.
The U.S. health system is often held up as an example of the failure of "private" medicine, yet this characterization is misleading. Indeed, the vast majority of payments to physicians or hospitals are directly or indirectly set by government and not by market forces. Moreover, the U.S. has one of the most government-regulated health systems in the world—and at a huge cost. Beyond payment, the close linkage between employment and health insurance just mentioned has severely limited choice and autonomy for the individual patient. For these reasons, many policy makers and consumers welcome movement away from governmental dictates toward individual consumer empowerment with information and control of the health care dollar.
Unfortunately, imaging-based screening centers, as an example of consumer-directed care, have so far fallen short of their laudable goals. One serious limitation is that they require out-of-pocket payment because the vast majority of health care insurance policies do not cover such screening. This type of service, then, may be accessible only to the socioeconomic group that has the means to pay out-of-pocket or to consumers who carry newer high-deductible insurance with health savings accounts. Access and a means to pay, though, are only parts of the problem.
Notwithstanding the obvious irregular quality and other controversies about implementation [1], the basic idea of screening for disease at imaging centers should not be immediately discarded. These centers may potentially benefit consumers of health care a great deal. It is widely acknowledged that providing medical care only for those who are already sick is neither efficient nor optimal from a public health perspective. Thus, screening and preventive care with pre-morbid detection of disease is extremely significant if implemented correctly. Estimates are that even a mere 1-percent permanent reduction in cancer death rates wouldsave $500 billion [2].
The Case of Dr. Kelly
The case described by the dialogue between Drs. Peterson and Kelly is hardly fiction. More than 108 imaging centers offering heart, lung, brain and other scans exist in the U.S today. In 2001, 88 centers were operational, distributed across the country and highly concentrated in coastal regions such as California, Florida and New York [1]. The distribution has changed over the past five years, but only slightly. Peaks in areas of concentration are less sharp than before and centers are now distributed across 31 states. In Canada and Europe, availability is also increasing steadily [3].
Benefits. The potential benefits of consumer-directed, self-referred imaging are significant. At the top of the list is the possibility of a life-saving finding or early intervention by virtue of detecting preclinical disease. While a life-saving discovery may be rare, and empirically established true positive rates are not as well-documented as widely cited anecdotal testimony of good outcomes, the early detection of subclinical disease has undeniable value. Second on the list of benefits is patient empowerment. For individuals to take control of their own health care is a good thing—for them and for society—assuming that appropriate access to information, full disclosure about risks and assistance for follow-up by physicians is available. Third is autonomy and privacy. In this electronic age when personal privacy may be all but an illusion, the opportunity to seek a medical answer to a nagging private question outside the traditional health care system is also desirable. This is true whether a consumer-patient is entirely asymptomatic and seeks reassurance of fine health or is one who worries in the wake of a medical scare.
Risks. A list of risks arises from indiscriminate use of imaging marketed to consumers without physicians in the loop. Our own work has shown that, given the current culture, design and framework for screening imaging, risks outweigh benefits in number and quality. The risks include:
- Psychological, health and financial costs of false positive findings and the potential for unnecessary, invasive follow-up tests.
- Risks incurred when an anonymous diagnostician relays highly significant information to a patient with whom he or she has no relationship or rapport.
- Diagnosis with no available therapy.
- Lack of standards for disclosure of benefits and risks.
- Caregiver conflict of interest.
- Unregulated quality control of radiologist and scanning methods and equipment.
- Risks of radiation from repeat CT scans; patients may visit many centers, and record-keeping across centers is not required.
- Inadvertent changes to patient lifestyle due to over-confidence in clearance from disease by screening imaging technology.
The impact of misleading marketing and advertising must also be taken seriously [4]. There is no question that competition among health care professionals is beneficial to all, but in medicine, where the asymmetry of information between clinicians and patient is high, competitive marketing can lead to problems. Most worrisome are aggressive advertising campaigns aimed at vulnerable prospective consumers: the patient who suffers from mental illness or the patient who is desperately seeking relief from untreatable disease or incompletely explained symptoms. The free availability of a wide range of information on the Internet is extremely positive, but the very nature of the Internet also allows medical information to be of variable quality, completeness and reliability, which exacerbates these risks [5].
Conclusion
Unlike the sales and marketing of pharmaceutical products, the market for consumer-directed imaging is currently unregulated and suffers from dramatic variations in quality on numerous levels. Individual physician caution, improved information and organized professional self-regulation would go a long way in ensuring the integrity of the practice and tipping the scale towards benefit over risk for the consumer. While current implementation of consumer-directed imaging centers for disease screening is problematic, the potential benefits of such technology should compel interested parties to figure out how to make it work for patients.
References
- Illes J, Fan E, Koenig BA, Raffin TA, Kann D, Atlas SW. Self-referred whole-body CT imaging: current implications for health care consumers. Radiology. 2003;228(2):346-351.
-
Murphy KM, Topel RH. The economic value of medical research. In: Murphy KM, Topel, RH, eds. Measuring the Gains from Medical Research: An Economic Approach. Chicago, Ill: The University of Chicago Press; 2003:41-73.
-
Racine E, Illes J. Neuroethics for clinicians: healthcare challenges of directly-marketed frontier neurotechnology. In: Singer P, ed. Bioethics for Clinicians. Vol 2. Cambridge, England: Cambridge University Press; In press.
- Illes J, Kann D, Karetsky K, et al. Advertising, patient decision-making, and self-referral for CT and MR imaging. Arch Intern Med. 2004;164(22):2415-2419.
-
Racine E, Van der Loos HZA, Illes J. Internet marketing of neuroproducts: new practices and healthcare policy challenges. Camb Q Healthc Ethics. In press.