Case
Dr. Lee runs a health care clinic in a suburb of New Jersey. Because it is the only primary care clinic in her small neighborhood, Dr. Lee has given continuous care to many of her patients for a long time. She enjoys working in such an environment; not only does she have strong relationships with most of her patients, but her intimate knowledge of their health history allows her to diagnose and manage many of their problems effectively. To supplement this, she actively keeps up to date with the latest treatments and medical information, especially those that relate to the health problems of her patients in the clinic.
Mrs. Williams, a regular clinic patient, came by because of back pain that she had had for a week. After completing a thorough physical check-up and precautionary X-ray, Dr. Lee concluded that the back pain was due to a slight muscle strain, and she prescribed some analgesics to relieve Mrs. Williams' discomfort until the strain healed.
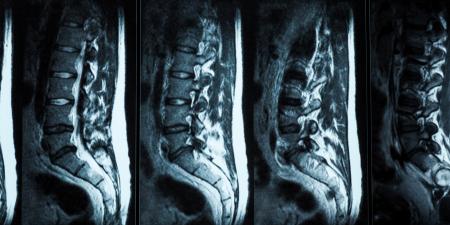
As she did during every patient visit, Dr. Lee asked Mrs. Williams, who was a librarian and 52 years old, if there were any other concerns she wanted to talk about. Mrs. Williams told her that she wanted an MRI of her back. "My friend Laura had some back pain a while back, just like what I have now, and it turned out to be a herniated disc." Dr. Lee was sympathetic to Mrs. Williams' concerns, but she explained that her physical exam did not indicate any need for a scan right now. "From my experience," Dr. Lee said, "a $1,000 MRI is not necessary. I think that it would be better to wait a few weeks to see if the pain, which appears to be due to a muscle strain, subsides before we consider a scan."
Mrs. Williams remained insistent on obtaining a referral. "After all," she argued, "the technology is there to diagnose problems, so why don't we use it, Dr. Lee? Better safe than sorry, right?"
Commentary
The case of Mrs. Williams and Dr. Lee is common throughout the country. It raises many issues, which include public perceptions and expectations of technology, trust in the patient-doctor relationship, lawsuits, cost, marketing strategies by the biomedical and pharmaceutical industries, and concepts of patient empowerment and autonomy.
Expectations
Technology has helped create a more evidence-based model of medicine and has reduced much of the subjectivity in clinical decision making. Improvements in the accuracy of diagnosis and in the effectiveness of treatment continue to raise public expectation of solutions once thought unattainable. Technological "miracles" have created demand for the best and the perfect. But technology's limitations remain under-appreciated or incompletely understood. Advanced diagnostic testing such as magnetic resonance imaging (MRI) is often perceived to be the sole means of establishing a diagnosis or planning treatment. This is not only a misperception of the public, it is also a stumbling block for physicians.
Even when a specific test or scan would provide no added clarity in a given clinical situation, it is still often viewed by patients as more reliable than an unaided physician's assessment. This is a perplexing phenomenon, given the common patient complaint that physicians do not spend enough time listening to them the way an empathetic human would and an instrument most certainly cannot.
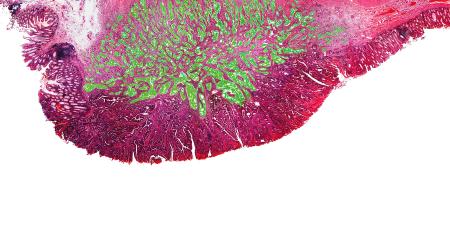
An MRI study is superior to X-ray studies in detecting joint erosion and soft tissue damage, but the correlation of MRI findings with clinical presentation is not reliable [1]. A patient may experience significant disability and pain with minimal signs on radiological studies (X-ray or MRI). Another may have significant signs on an MRI and be relatively asymptomatic. Over-reliance on the MRI or X-ray at the expense of the clinical picture can become a barrier rather than an aid to communication with the patient.
Educating patients about the limitations of the technology, the meaning of the results and the implications of various results for the treatment plan could bring about greater acceptance of the proper timing for the use of the technology.
Patient-Physician Relationship
Mrs. Williams' concern should not be dismissed; anxiety can aggravate her back pain by causing increased muscle tension and strain. Likewise, Dr. Lee's established relationship with Mrs. Williams is based on trust, which is threatened by the possibility that Dr. Lee may be withholding the best care available because she doesn't deem it necessary at this time.
Should Dr. Lee consider an MRI to relieve Mrs. Williams' anxiety and retain her confidence? Not necessarily. Dr. Lee can lessen Mrs. Williams' anxiety by exploring the source of her concern and educating her on the signs and symptoms found during her physical exam and their implications for treatment. Most importantly she must assure Mrs. Williams that her complaints are not being dismissed and that whatever might appear on an MRI would not alter the initial treatment recommendations significantly. More aggressive treatment including surgery would still be preceded by approaches associated with less risk. A trial of analgesics is a good example of a conservative approach. Mrs. Williams' pain and anxiety can be addressed by acknowledging that, although the X-ray showed no changes at this time, her complaints are taken seriously and will be followed systematically.
Defensive Medicine: The Influence of Litigation
Lawsuits have been found to be related more to patients' anger than to adverse outcomes [2]. Although such suits seldom result in decisions against the physician, they can still have a negative impact, resulting, for example, in demands for reporting credentials to hospitals in order to gain privileges and to health insurance plans in order to be included as providers. The very fact of the suit can complicate procedures for gaining future state licenses and may wind up in public online disclosure in some states [3,4]. Attorneys are able to file suits on limited grounds that nevertheless may require a physician's attention for years before being removed from the court file. Aware of these tort abuses, some physicians may decide to give patients what they want rather than risk frivolous lawsuits.
Will an MRI protect Dr. Lee against litigation in Mrs. Williams' case? While a negative MRI result might diffuse her interest in suing, Dr. Lee's attempts to reduce her fear, anger and loss of trust will trump MRI results. It is far better to focus on the patient than on the demanded technology.
Cost
Insured patients' disregard of cost (because they are not paying out-of-pocket) promotes overutilization of expensive tests, as physicians struggle to assure their patients that the best care is not being withheld. While one may believe that "best care" for every sprained knee in the ER includes MRI and other studies to rule out osteosarcoma, acting on such a belief would soon bankrupt the U.S. health care system, and it would delay treatment for patients who must sit and wait while an extensive work-up of all complaints takes place. Physicians must speak out as a group and educate the public on judicious use of medical technology to ensure that proper interventions are available when they truly are needed.
Marketing
Information on the latest drugs and technologies is available on the Internet, in self-help books and even on television. TV ads recommend that patients ask their physician about specific products. Representatives from the pharmaceutical and biotechnology industries approach physicians with gifts intended to sway them to use and prescribe the company's products. Industry's entrepreneurial activities increase public interest in brand name products but also create the fear among prospective patients that they may not have access to the right treatment unless they ask for it themselves—that their physicians may not be knowledgeable about a product or simply may not think that the patient needs it at a given time.
Patient Autonomy Versus Paternalism
This wide access to information has resulted in significant behavior change. Patients now shop for medical information as freely as they do for recipes, which gives them a greater sense of power over their care and an impatience and suspicion of physicians who do not share their views of diagnosis and treatment. Respect for patient autonomy is increasingly coming to mean that the patient informs the physician of the diagnosis and treatment plan. Having a medical opinion informed by years of training, testing and governmental oversight that does not agree with the patient's self-assessment and Internet search has suddenly become "paternalism."
Entitlement Versus Allocations of Resources
The notion of rationing scarce resources is well understood in other nations, but not in America, where needs are believed to be entitlements. Medical care is certainly a necessity. It can even be argued that access to a basic level of medical care should be available to all [5]. Taking this a step further, one can ask whether the most expensive medical care should be available to all. There are likely to be more affirmative answers to that question in America than in any other nation. This is partly due to the high expectations of excellence in America and partly due to the sense on the part of many that they are entitled to have anything they need.
Conclusion
We have looked at a few issues that are raised daily all across the country in cases similar to that of Mrs. Williams and Dr. Lee. The physician has the daunting task not only of communicating effectively with individual patients but of serving the public interest through just allocation of available resources. If health care is going to be optimized for all, an understanding of the proper use and application of technology will need to be guided by those most in the position to do so. Certainly that should include physicians.
References
-
Humphreys SC, Eck JC. Clinical evaluation and treatment options for herniated lumbar disc. Am Fam Physician. 1999;59:575-582; 587-588. Available at: http://www.aafp.org/afp/990201ap/575.html. Accessed January 5, 2007.
- Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Proc (Bayl Univ Med Cent). 2003;16(2):157-161.
-
American Medical Association. American Medical Association's medical liability crisis map. Accessed December 3, 2006.
-
Weiler PC, Newhouse JP, Hiatt HH. Proposal for medical liability reform. JAMA. [Special Communication.] 1992;267(17):2355-2358.
-
Saha P, Saha S. Impact of managed care on the development of new medical technology: ethical concerns. In: Grundfest WS, ed. The role of technology in the cost of health care: providing the solutions. Proc. Health Care Technology Policy II, SPIE. 1995;2499:416-423.