Electrical stimulation of neural tissue by surgically implanted neuroelectronic devices to restore lost neural function has become an integral part of today's medicine. Ethical issues and the current public debate about these implants precipitate around two major questions:
- Does the benefit of the prosthetic implant justify the risk of adverse effects to the individual and to society?
- Is it desirable to enhance human capabilities by neuroelectronic devices?
The objective of this paper is to provide both scientific and moral arguments in this ongoing debate. As with most public discussions, arguments about human-neuroelectronic interfaces are clouded by fears, hopes, market interests and academic endeavors, as well as by philosophical and religious differences of opinion.
The case of the cochlear implant helps to define both questions. There is no doubt that cochlear implants benefit thousands of people without major risk. Still, even the cochlear implant is not universally accepted as a therapeutic intervention by the profoundly deaf. Some see it as an intrusion into their way of life, claiming that the implant threatens to eliminate their standing as a culture and thus compromise their autonomy [1-4]. Moreover, some contend that, in a community of deaf people, (re)gaining hearing for a single individual could be considered an enhancement, an additional capability on top of what other members of the community have, gained by artificial means.
About neuroelectronic implants in general, it is argued that people may be transformed more radically or profoundly than with other techniques of intervention. And it is feared that neural prostheses directly coupled to the brain may threaten personal identity. It is not only among the deaf that this might separate an individual from the community.
Therapy: neural prostheses available today
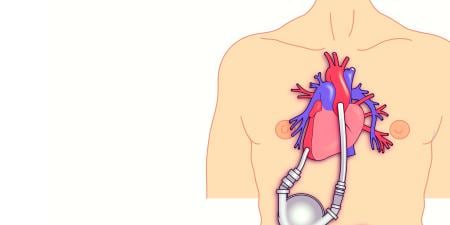
Broadly defined, a neural prosthesis is a device implanted to restore a lost or altered neural function. Neural prostheses work in one of two ways, either (1) by delivering electrical stimulation that excites or inhibits neural tissue or (2) by picking up electricity generated by the brain and using it to control computer cursors, electromechanical devices or even paretic limbs. Until now, both methods have been applied only after pharmacologic options have been exhausted. They have proven to be very effective, most prominently with respect to deep brain stimulation in Parkinson's disease where high-frequency stimulation causes inhibition of the subthalamic nucleus [5]. Despite ethical problems raised by sham surgeries conducted as placebo controls [6-8], the success of these techniques in improving the lives of several thousand patients makes it impossible to ignore the benefit of this option.
Restoring sensory pathways is one of the more classic applications of neural prosthetics. Cochlear implants, introduced into clinical practice in the early 1960s, have become a routine procedure today, especially in children. Multichannel cochlear implants have been provided to hundreds of thousands of patients today, making speech development possible and enabling a majority of them to use the telephone. Auditory brainstem implants with electrodes placed over the cochlear nucleus or even pushed into the brainstem have proven capable of restoring some residual hearing in a few hundred patients who had lost both hearing nerves.
Visual implants, on the other hand, are still investigational and have just entered phase 1 trials. More than 20 research groups worldwide are currently working on electronic implants to restore vision in blind patients. Methods include electrical stimulation at the receptor level (subretinal implants), at the origin of the optic nerve (epiretinal implants), at the optic nerve itself and at the visual cerebral cortex. Another line of research is the fabrication of hybrid implants—neurons cultured on photosensitive silicon chips—with the potential to form a biological connection that restores the whole visual pathway.
While premature enthusiasm with respect to clinical applications has inspired false expectations in the past, research in this field is now progressing more slowly and steadily. Currently, most researchers anticipate that an implant will probably not fully restore vision but may allow a blind person to move freely in a familiar environment, guided by visual perception of contours, outlines and shades of light.
Translating neuronal signals into actions. So-called "brain-computer interfaces" (BCIs) basically work the other way around: rather than stimulating neural structures, they pick up electrical potentials generated in the brain as a byproduct of neuronal activity. This term, as well as the terms "human computer interface" and "brain-machine interface" describe invasive or noninvasive devices that can restore lost motor or sensory-motor functions by translating raw neuronal signals into electrical impulses sufficient to control a computer cursor or reproduce arm and hand movements with artificial actuators [9,10].
In principle, it is also possible to control computer cursors and artificial limbs by eye movements and noninvasive electrodes. But when the recording devices for brain signals are not fully implantable, the computational algorithms are not sophisticated enough to provide a wide range of subtle and distinct movement and there is no sensory feedback from the actuators, so the acceptance of these implants would remain rather limited, even if the neurosurgical procedures were free of risks—which in fact they are not.
Safety
Neural prostheses have a general disadvantage over other methods employed to restore or even enhance neural function: they typically involve an invasive surgical procedure. Given that risk, why would anyone seriously choose surgical connection of artificial devices to the human brain? The answer, in large part, is that these implants restore neural function where all other methods fail, function continuously without the patient having to attend to them or interrupt or alter his or her normal behaviour, can be completely hidden under the skin, and can be turned off easily.
Surgical risks, such as hemorrhage and infection, are minimal with deep brain stimulation and less-than-minimal for vagal nerve stimulation like that used for control of epileptic seizures. The main difficulty with risk assessment in these medical technologies is our limited understanding of the physiological mechanisms involved and the neural circuitry upon which they act. Stimulating neural structures with an electrical current without knowing all the physiological mechanisms that may ultimately be turned on or off by this stimulation is bound to cause some unforeseeable effects, especially if the targets are small and located in brain regions with dense neuronal packing.
Patient satisfaction with the treatment result is often quite high, but relatives and friends sometimes complain of personality changes in the patient, ranging from transient confusion and bradyphrenia to euphoria or depression. These changes, however, occur in a minority of patients, and it is unclear whether the electrical stimulation per se directly causes them. It may be that when some symptoms are eliminated through electrical stimulation, other aspects of the disease are unmasked (e.g., depression is recognized only when movement disorder is improved). It is also possible that psychosocial changes (e.g., acting out) are epiphenomena related to the relief of the patient's symptoms.
Still, the vague fear that, due to the treatment, a patient may no longer be "who I used to be" could prevent individual patients from undergoing these medical procedures and lead to disapproval from the general public. During the research phase, therefore, any new central neural prosthesis should be monitored systematically for subtle side effects that affect personality and mental capacities related to personhood.
Ethics committees as well as official agencies like the FDA demand careful study designs to evaluate new technologies. These demands have been met in the past, and it is safe to say that, for sensory prosthesis like the cochlear implant, the risks and adverse effects are negligible today.
While placebo-controlled studies are hardly possible when surgery is involved, intelligent study designs like crossover paradigms, where a device is implanted but not activated in half of the patients for a limited time, can make up for this drawback. As long as the risks and side effects are acceptable, the main question will always be whether the new treatment modality helps any better than other, less invasive or less risky measures.
Limitations and trends
As Hollywood's cyborgs and man-machine creations become more and more confused with reality in the public eye, it is worthwhile to consider some of the limitations of neural prostheses today.
- Sensory implants contact the neural tissue with a relatively small number of electrodes compared to the multitude of anatomical neurons involved in the sensory pathways.
- Implants are placed in sensory pathways that have been severed. With a lesion in the central nervous system there usually is little chance of natural regeneration. Other elements in the severed pathway may degenerate, too, when not in use.
- Electrodes contacting the neural tissue are prone to rejection and degradation. On the other hand, they may also damage the neural tissue that they are supposed to stimulate.
- The neural interfacing of electrodes is far from mimicking the anatomical and physiological connections in a neural network.
- Refractory properties limit the number of electrical impulses a neuron will respond to in a given time interval.
- Output functions of brain-computer interfaces tend to be rather slow. Even with a well-tuned 96-electrode, BCI speed is limited to 6.5 bits per second or approximately 15 words per minute typed with a key selection system [11].
Moreover, size, biocompatibility, durability and energy supply are basic problems for all neuroelectronic implants, but, considering recent developments, it does not appear these will remain critical in the long run.
Current research
Apart from improving and miniaturizing technical details, there are two promising lines of research aimed at improving the performance of neuroelectronic interfaces. The first approach is to obtain more information on the structural organization and the working principles of neuronal networks and their function. For example, with a technique they call "linear decoding," researchers at the University California, Berkeley, were able to reconstruct actual moving images from electrophysiological recordings by means of electrodes placed in a cat's lateral geniculate ganglion, a neural structure connected to the cat's optic system [12]. They have also shown that it is possible to map non-linear neuronal responses to visual stimuli in the visual cortex.
A group in Germany has recorded electrical brain activity in response to rising and falling tones from the auditory cortex in gerbils. Interestingly, when the auditory cortex itself was stimulated with similar electrical signals at the same location, the animals were able to discriminate rising and falling tones in the absence of any sound presentation [13].
Experiments like these lead to the second approach—attempts to model neurobiological structures based on their morphological and functional characteristics ("morphing"). One example from the University of Pennsylvania is the creation of an artificial retina, a silicon-based microchip that includes 3,600 output "cells," simulating characteristic responses to light stimulation of the four major clusters of retinal ganglion cells [14]. With their axonal processes, these cells account for 90 percent of the fibres of the optic nerve. The "neuromorphic" chip consumes only one-thousandth of the power required by a regular PC.
One of the most ambitious projects in this respect combines methods of computational neuroscience with computer engineering to "morph" memory functions of the hippocampus with computer hardware and software at the University of Southern California [15]. At present, it is hard to see how such an artificial neural network could be functionally interfaced with the human brain. Moreover, human memory is based on continuous changes in the efficacy and qualities of cellular and molecular processes. A "memory chip" would have to adapt continuously to such changes. There is no way of knowing where research of this kind may take us in the future. Considering the complexity of the task, it comes as no surprise that the answers range from "nowhere" to a "superhuman race" and that these answers are based mostly on matters of belief rather than scientifically proven facts.
Where do we go from here?
Even if the restoration of lost or disturbed neural function by neural prosthesis is a temporary phase before better treatments are made available through biotechnology, neural prosthesis will be a dynamic and growing field in medicine for many years to come. Clinical indications will be extended, e.g., to electrical brain stimulation in epilepsy and in the treatment of migraine, depression and obsessive-compulsive disorder.
Microtechnology now makes it possible to minimize electrodes and enlarge their active surface by laser treatment. Coating of the electrodes with growth factors appears to improve the electrical contact to the neural structures, and conductive varnish with nanoparticles reduces the breakdown of electrodes by living tissue. Neurons cultured on nanofibres develop neurite extensions, and the artificial material employed counteracts astrocytic scar formation at the same time [16].
Neural cells can be grown onto silicon chips and promote fibre growth connecting the implant to the nervous system. "Artificial synapse chips" capable of communicating with the nervous system on a chemical (electro-osmosis) rather than electrical basis are being developed [17].
Microfluidic implants can serve both as neural prosthesis and as focal drug delivery systems. They are composed of electronic implants combined with mechanical actuators capable of releasing a variety of different chemicals, e.g., neurotransmitters or drugs, in a very small volume of biological tissue.
Treatment versus enhancement
The interventions that have just been described appear to be in line with the prevention and treatment goals of medicine, and society will probably not have major objections to neuroelectronic implants as therapeutic devices [18]. Use of technical intervention to improve the physical, cognitive or psychological aspect of an individual beyond what is considered "normal" may be different. While the distinction between treatment and enhancement may be difficult in borderline cases, it can safely be assumed that enhancing healthy human beings is not part of the responsibility of health care professionals, which is to treat and prevent diseases and to restore function that is normal for an individual of a given age and sex. Enhancement with neuroelectronic devices would not fall under the obligatory force of the principle of beneficence in medicine. Respect for autonomy—especially with regard to enhancement of children—and questions of distributive and social justice will undoubtedly clash in the debate over enhancing human beings with neural implants.
When we look ahead to possible enhancement with electronic devices directly coupled to the human brain, is the first question that comes to mind really whether there should be limits to enhancements in the interest of remaining human? Or is the first question: Do we really want to be enhanced with surgically implanted devices when it might be possible to achieve these gains by noninvasive devices or even by pharmacological means? Infrared vision, perception of radio-frequency signals, ultrasound hearing and even invisible communication can all be accomplished by small external devices today. Enhancing well-being, motivation and cognition by administering drugs—in other words "doping"—is well established.
Ethical analysis is essential
Finally, with every new step in the development of technologies, there will be a potential for abuse. To many, enhancement by connecting electronic devices to the human body and brain will appear, at least prima facie, morally suspect. Others have argued that these enhancement technologies offer an opportunity to make life more worthwhile, provided that society responds appropriately to the implicit social challenges, including that posed by distributing these technological interventions justly.
A variety of science fiction scenarios involving cyborgs and the imminent transformation of the human race into a semi-electronic species has left the public rather perplexed and provoked reactions against scientific progress in the field of neural prosthetics. Even though neuroelectronic technology is available, few human beings would choose to be permanently enhanced by implanted electronic devices. And as long as technology does not progress to the point where implants have advantages unsurpassed by less-invasive means, concerns about an enhanced transhuman race can be put off until later.
Ethical analysis should strive to separate realistic forecasts from the more speculative ones. Still, we should be aware of the accelerating pace of implant technology, driven mainly by trends in microcomputing, neuroscience and medicine. While there is certainly no point in trying to stop the development of central neural implants, an early and thoughtful discussion of their potential benefits and risks must lay the groundwork for a responsible application of this very promising technology.
References
- Crouch RA. Letting the deaf be deaf. Reconsidering the use of cochlear implants in prelingually deaf children. Hastings Cent Rep. 1997;27(4):14-21.
- Lane H, Grodin M. Ethical issues in cochlear implant surgery: an exploration into disease, disability, and the best interests of the child. Kennedy Inst Ethics J. 1997;7(3):231-251.
- Lane H, Bahan B. Ethics of cochlear implantation in young children: a review and reply from a Deaf-World perspective. Otolaryngol Head Neck Surg. 1998;119(4):297-313.
-
Englert H. Hört, hört! Gehirn & Geist. 2006;7-8:63-70.
- Benabid AL, Deuschl G, Lang AE, Lyons KE, Rezai AR. Deep brain stimulation for Parkinson's disease. Mov Disord. 2006;21(Suppl 14):S168-S170.
- Boer GJ, Widner H. Clinical neurotransplantation: core assessment protocol rather than sham surgery as control. Brain Res Bull. 2002;58(6):547-553.
- Edward SJ, Stevens AJ, Braunholtz DA, Lilford RJ, Swift T. The ethics of placebo-controlled trials: a comparison of inert and active placebo controls. World J Surg. 2005;29(5):610-614.
- Horng S, Miller FG. Ethical framework for the use of sham procedures in clinical trials. Crit Care Med. 2003;31(Supp 3):S126-S130.
- Friehs GM, Zerris VA, Ojakangas CL, Fellows MR, Donoghue JP. Brain-machine and brain-computer interfaces. Stroke. 2004;3511(Suppl 1):2702-2705.
- Lebedev MA, Nicolelis MA. Brain-machine interfaces: past, present and future. Trends Neurosci. 2006;29(9):536-546.
- Santhanam G, Ryu SI, Yu BM, Afshar A, Shenoy KV. A high-performance brain-computer interface. Nature. 2006;442(7099):195-198.
- Stanley GB, Li FF, Dan Y. Reconstruction of natural scenes from ensemble responses in the lateral geniculate nucleus. J Neurosci. 1999;19(18):8036-8042.
- Ohl FW, Scheich H, Freeman WJ. Change in pattern of ongoing cortical activity with auditory category learning. Nature. 2001;412(6848):733-736.
- Zaghloul KA, Boahen K. Optic nerve signals in a neuromorphic chip II: Testing and results. IEEE Trans Biomed Eng. 2004;51(4):667-675.
- Berger TW, Ahuja A, Courellis SH, et al. Restoring lost cognitive function. IEEE Eng Med Biol Mag. 2005;24(5):30-44.
- Webster JT, Waid MC, McKenzie JL. Nano-biotechnology: carbon nanofibres as improved neural and orthopaedic implants. Nanotechnology. 2004;15(1):48-54.
- Peterman MC, Noolandi J, Blumenkranz MS, Fishman HA. Localized chemical release from an artificial synapse chip. Proc Natl Acad Sci USA. 2004;101(27):9951-9954.
-
Jones DG. Enhancement: are ethicists excessively influenced by baseless speculations? Medical Humanit. 2006;32(2):77-81.