What are the goals of medicine? Are they fixed and immutable? Is there consensus concerning them? Current thinking about the goals of medicine should guide health care delivery, research and medical education. The literature on the goals of medicine is sparse, however, and "issues of purposes and values tend to be crowded out by…technical questions" [1] related to science or the organization and financing of health care. Therefore, I wanted this issue of Virtual Mentor to focus on some of the basic questions about medicine and its aims. I also wanted these discussions to be sufficiently concrete to have relevance for practicing physicians; for example, to what extent are physicians obligated to respond to patient demands? This collection of writings aims to link reflections on the goals of medicine with day-to-day decisions regarding patient care and with laws, policies and education methods that directly affect medical practice.
The Hastings Center Goals of Medicine project articulated four goals: (1) the prevention of disease and injury and the promotion and maintenance of health; (2) the relief of pain and suffering caused by maladies; (3) the care and cure of those with a malady and the care of those who cannot be cured; and (4) the avoidance of premature death and the pursuit of a peaceful death [2]. Although we might squabble over wording, the substance of these intentions is difficult to dispute, and these goals provide a starting point for discussion.
Writing for the Hastings goals project, Hanson and Callahan present three very compelling reasons why we—physicians, bioethicists and patients—should care about the goals of medicine. The first is that "it makes no sense to talk about the financing and organization of health care systems unless we understand the purpose of the enterprise" [3]. The second is that "the rapid advances of twentieth-century medicine have generated enormous ethical, cultural, and legal problems—and a remarkable number of them turn on what it is thought right or wrong, good or bad, for medicine to do for people in the name of preserving or improving their health" [4]. The third is that "modern scientific medicine seems to have elevated some goals of medicine—its intent to save and extend life, for instance—over other important goals, such as the relief of suffering and the pursuit of a peaceful death. It is exceedingly helpful to realize or sense the ensemble of medical goals, and then ask how they should fit together" [2]. In addition to addressing specific medical goals, each article in this issue of Virtual Mentor demonstrates how discussion of ethical issues in medicine can always benefit from some thinking about basic goals.
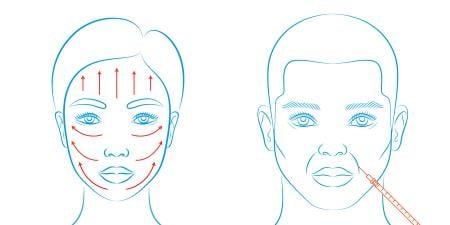
Taking the goals of medicine into consideration can help physicians solve clinical ethical dilemmas. Modern medical technology offers considerable potential to alter and control human life and not simply cure disease. The three clinical cases in this issue illustrate dilemmas faced by physicians when patients request treatments that may not be medically necessary. In each of these cases, a physician struggles to identify the legitimate medical goal. First, physician and attorney Julie D. Cantor discusses a physician's misgivings when a patient mentions cosmetic surgery—a common and socially acceptable practice performed under the aegis of medicine that carries real risk without direct medical benefit. In the second case, a pediatrician faces parents' demand for an immediate medical solution to a yet-undefined problem. Psychiatrist Elizabeth Kieff emphasizes the importance of not letting patients' (or, in this case, parents') requests distract physicians from providing appropriate care. To supplement this case, Sarah Maitre summarizes the complicated diagnosis of attention deficit hyperactivity disorder in the clinical pearl. In case three, a young couple seeks assistance from a reproductive endocrinologist in selecting the sex of their child. Physician and attorney Louise P. King asks whether a physician should provide services that are not medically necessary simply to satisfy patient demands.
In the medical education section, Elliot M. Hirsch explains how empathy can enhance patients' experiences and treatment, stressing that medical care involves more than technical skills. In the journal discussion, Erica Rangel critiques an argument on the definition of cosmetic psychopharmacology (the use of psychoactive substances to effect changes in function for individuals with who do not have diagnoses of mental illness). Absent a diagnosis, prescribing medication can sometimes fulfill legitimate medical goals; in other cases, it may be simply be bad medicine.
In the health law forum, Lee Black traces the development of defensive medicine—a practice that arises from physicians' fear of malpractice lawsuits and distorts the goals of medicine. In the policy forum, Mary Simmerling argues (in the vein of Norman Daniels) that one of the key goals of medicine is to protect fair equality of opportunity and uncovers problems with the current (purportedly equitable) organ transplantation system. In medicine and society, Bruce Jennings reflects on how consideration of goals of medicine should inform end-of-life care decision-making. And Kenneth A. Richman highlights the importance of communication between doctors and their patients about treatment goals in a second contribution to the medicine and society section. Barbara A. Hinze closes out the June 2007 issue with a medical humanities piece that looks at medicine's goal of relieving suffering and how that can be aided by giving patients a voice of their own and understanding their narratives.
As editor of this theme issue, it is my goal that readers be stimulated to consider the core aims of the enterprise of medicine and how those aims should guide decisions at the level of both patient care and public policy.
References
-
Hanson MJ, Callahan D, eds. The Goals of Medicine: The Forgotten Issues in Health Care Reform. Washington, DC: Georgetown University Press; 1999:ix.
-
Hanson, Callahan, xi.
-
Hanson, Callahan, x.
-
Hanson, Callahan, x-xi.