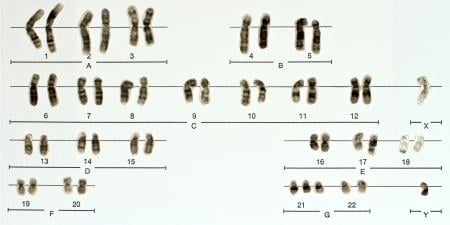
People are increasingly obtaining genetic information about themselves that, unlike other medical information, may directly concern not only them, but also their biological relatives [1]. This aspect of genetic information poses ethical issues for physicians by challenging the limits of medical confidentiality when it comes to genetic test results [1]. While recognizing the need for confidentiality [2], the Code of Medical Ethics of the American Medical Association stresses that pre- and post-genetic counseling must include implications of genetic information for patients’ biological relatives [3]. According to the code, physicians should tell patients who are considering undergoing genetic testing the circumstances under which they would expect those patients to notify biological relatives of the availability of information related to risk of disease [4].
Legal Decisions on the Duty to Warn
It was not until 1995 that the courts recognized a legal duty to warn both a patient and the patient’s immediate blood relative that they may be at risk from a genetically transmissible condition [5]. This duty stands, irrespective of the duty of confidentiality between patient and physician, and regardless of whether a treatment relationship exists between the physician and the patient’s relatives. The two primary cases that established this duty both recognized a duty to warn, though they arrived at different conclusions about what that warning might entail.
Pate v. Threlkel. In Pate v. Threlkel, the Supreme Court of Florida found that a physician has a duty to warn patients of the genetically transferable nature of the condition for which they are being treated [6]. Though this duty extends to informing the patient’s children, the court held that the duty is satisfied by warning the patient of the familial implications of genetic testing [6].
Three years after her mother, Marianne New, was treated for medullary thyroid carcinoma, a genetically transferable disease, Heidi Pate learned that she had an advanced form of the disease [6]. Pate and her husband filed suit against the physicians who had treated her mother, alleging that: (1) the physicians knew or should have known of the likelihood that New’s children would inherit the condition; (2) the physicians were under a duty to warn New that her children should be tested for the disease; (3) had New been warned 3 years prior to her discovery of her condition, she would have had her children tested at that time; and (4) if Pate had been tested at that time, she would have taken preventive action, and her condition would have most likely been curable [6]. Pate was an adult at the time New was undergoing treatment for medullary thyroid carcinoma [6].
The court first determined whether New’s physicians had a duty to warn New of the genetically transferable nature of her disease. The court answered this question in the affirmative, since a reasonably prudent physician would give such a warning to his or her patient in light of all relevant circumstances [6]. The court then moved on to the question of whether, given the duty to warn a patient of the genetically transferable nature of her disease, a physician also has a duty to warn the patient’s children or other third parties [6]. This question was a matter of first impression in Florida, meaning that it was the first time the court was presented with the issue.
The court recognized that the prevailing standard of care—a duty to warn the patient—was “obviously developed for the benefit of the patient’s children as well as the patient” [6]. The court further found that, when the physician knows of the existence of these third parties, the physician’s duty to warn extends to them [6]. This holding, however, did not require that the physician himself warn the patient’s children of the disease; sharing this information with third parties without the patient’s permission would conflict with Florida’s confidentiality statute [6]. In circumstances where the physician has a duty to warn of a genetically transferable disease, the Patecourt said that duty could be satisfied by simply notifying the patient [6].
Safer v. Estate of Pack. Shortly after Pate, the court in Safer v. Pack held that a physician’s duty to warn those known to be at risk of avoidable harm from a genetically transferable condition might not be satisfied by telling only the patient [7].
The plaintiff in Safer suffered from cancerous blockage and multiple polyposis of the colon, a condition her father had been treated for when she was a minor [7]. Pack brought suit against the estate of her father’s physician (who died in 1969), alleging that the disease was hereditary and that the physician had breached duty to inform those who were potentially at risk of developing the condition [7].
While the court warned that an overly broad and general application of the physician’s duty to warn might lead to confusion, conflict, or unfairness, the court was confident that the duty to warn of avertable risk from genetic causes was sufficiently narrow to serve the interests of justice [7]. The court employed the concept of a “genetic family”—the idea that genetic information is not just personal medical information but is simultaneously personal and familial [8]—in extending the duty to warn beyond the patient to members of the patient’s immediate family [7]. The court took a step beyond Pate by noting that the duty to warn could not always be satisfied by informing the patient of the transferable nature of his or her disease [7].
Ethics Policy on the Duty to Warn
In the wake of Pate and Safer, the American Society of Human Genetics (ASHG) published a policy paper that reaffirmed the general rule of confidentiality and set forth factors defining the circumstance under which a physician should directly warn the patient’s immediate family. The ASHG policy favors discretion on the part of physicians in disclosing information about genetically transferable conditions to those at risk for developing them [8]. ASHG recommended a two-part approach to disclosure that respects the confidentiality of genetic information while acknowledging that the information is both individual and familial in nature [8].
ASHG’s policy first provides that physicians, under a standard duty of care, must inform patients prior to and following testing about the familial implications of genetic testing [8]. This step, similar to that found in AMA Opinion 2.131, preserves the duty of confidentiality while providing the patient with information necessary to inform or not to inform his or her family of test results [4]. But the ASHG goes further. After satisfying the duty to warn the patient, ASHG says, the physician can use the discretion to notify at-risk members of the patient’s family when four factors are present:
- Attempts to encourage disclosure on the part of the patient have failed.
- The harm is highly likely to occur and is serious and foreseeable.
- The at-risk relative is identifiable.
- The disease is preventable, treatable, or medically accepted standards indicate that early monitoring will reduce the genetic risk [8].
Similarly, the President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research suggested that disclosure without the patient’s consent is only justified if: (1) reasonable efforts to elicit voluntary consent to disclosure have failed; (2) there is a high probability both that harm will occur if the information is withheld and that the disclosed information will actually be used to avert harm; (3) the harm the identifiable individuals would suffer would be serious; and (4) appropriate precautions are taken to ensure that only the genetic information needed for diagnosis or treatment of the disease in question is disclosed [1]. Unlike the courts in Pate and Safer, the AMA and other organizations clearly recognize and respect a physician’s duty of confidentiality, particularly with regard to highly sensitive genetic information. Only when the third-party interests are so great as to override this duty of confidentiality should a physician balance a competing duty to warn.
References
-
American Medical Association. Council on Ethical and Judicial Affairs. Report 9 (A-03). Disclosure of familial risk in genetic testing. Chicago, IL: American Medical Association. 2007. http://www.ama-assn.org/ama1/pub/upload/mm/code-medical-ethics/2131a.pdf. Accessed August 10, 2009.
-
American Medical Association. Opinion 2.137. Ethical issues in carrier screening of genetic disorders. Code of Medical Ethics. Chicago, IL: American Medical Association. 2007. http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion2137.shtml. Accessed August 10, 2009.
-
American Medical Association. Opinion 2.12. Genetic counseling. Code of Medical Ethics. Chicago, IL: American Medical Association. 2007. http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion212.shtml. Accessed August 10, 2009.
-
American Medical Association. Opinion 2.131. Disclosure of familial risk in genetic testing. Code of Medical Ethics. Chicago, IL: American Medical Association. 2007. http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion2131.shtml. Accessed August 10, 2009.
-
Wolf SM, Paradise J, Nelson CA, Kahn JP, Lawrenz F, eds. Symposium: incidental findings in human subjects research: from imaging to genomics. J Law Med Ethics. 2008;36(2):216-283.
-
Pate v Threlkel, 661 So2d 278 (Fla 1995).
-
Safer v Estate of Pack, 677 A2d 1188 (NJ Super Ct App Div 1996).
-
Kovalesky ML. To disclose or not to disclose: determining the scope and exercise of a physician’s duty to warn third parties of genetically transmittable conditions. U Cincinnati Law Rev. 2008;76:1019-1041.