To understand the evolution of dynamic spine stabilization devices, it is helpful to look into the history of spine treatment concepts. Dynamic spine stabilization devices evolved from prior spine stabilization implants involving surgical fusion.
There are two general categories of surgical treatments for spinal problems and pain: (1) decompression of neurologic structures for sciatic and nerve pressure problems, and (2) stabilization/reconstruction or realignment of bony components for structural problems. Treatment alternatives within each category are many, varied, and continually evolving.
Spine stabilization is employed for the structural concerns—instability, pain, and misalignment—in category (2), and, in the past, fusion was the key component in this surgical intervention. Fusion involves joining motion segments (a disc and the vertebrae above and below it) together so that they no longer move at the affixed sites, improving stability and alignment and relieving pain. Original efforts at spine treatment typically followed traumatic events which left bony alignment with suboptimal support. As this technology evolved, it began to be used not only following trauma but also to treat deformity and degenerative/aging problems. Advances in engineering and biomechanic improvements also contributed to its broader use.
The concept of fusing motion segments to improve stability and relieve pain was supported by past clinical and radiographic observation that reduced mobility and sometimes autofusion are part of natural aging. Autofusion was noted to be accompanied by diminished pain but was often also accompanied by overall reduction of activity associated with the aging process.
As engineers developed better materials and improved stabilization support constructs to enhance fusion techniques, earlier methods—which had been seen as an improvement over nonsurgical treatments—came to be considered suboptimal. The earliest stabilization devices to enhance and support fusion also came to be thought suboptimal and this gave way to advancements in fusion technology. After more data collection, it has been found that, while advanced materials have resulted in better structural constructs, they have not produced a satisfactory level of clinical improvement. (It should be understood, however, that not every fusion relieves pain and not every failed fusion results in continued pain.) With time, those segments that fused successfully were subject to wear from the segments above and below them, possibly accelerated because of the fusion. So, more recently, surgical resources have been directed toward developing mechanical reinforcements that maintain motion and enhance and support moveable surfaces. Initially this was attempted by disc replacement, but the technique evolved into use of posteriorly supported motion-retention constructs as well.
The general thinking about structural spine treatment, then, has changed from the earlier notion that the “advantages” of natural aging and degeneration could be achieved through a fusion procedure to current techniques for resurfacing and preserving spinal motion through replacement and motion segment support.
These new mechanical constructs, however, face challenges of their own. Once an “old-style” fusion is solid, the structural implants are no longer subjected to mechanical stresses. In newer motion-retention devices, the implanted device must withstand mechanical forces and loads for a much longer time and continue to perform satisfactorily.
Posterior Motion-Retention Devices (PMRDs)
The augmentation or supplementation of motion through posterior motion activity has developed along several lines. Early engineering assessments looked at how posterior motion joints (facets) wear and whether they are subjected to any greater specific mechanical stresses such as flexion/extension, shear, or axial rotation. Studies in the literature have not found that any one particular motion needs to be augmented or supplemented, and there is some belief that wear is related to both genetics and life experience, so no one solution will work for all patients. It is also speculated that, as early wear takes place, the patient’s body may compensate by greater degeneration and arthritis and, subsequently, reduced motion.
The cost to develop a spinal implant is high, and the investment, risky. Large companies have been averse to developing these technologies in light of stringent government and insurance company regulations. They seem to be more interested in acquiring the technology once it has been designed and approved.
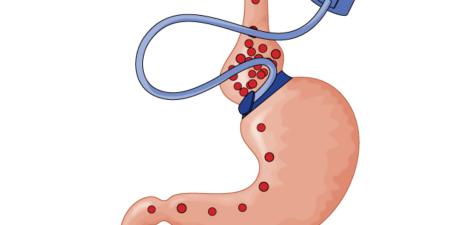
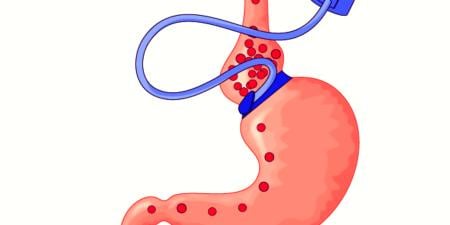
Posterior motion-retention devices (PMRDs) developed from posterior fusion implants, but an understanding of the basic science and mechanics of wear seemed to be lacking. This gap has been filled by creative design solutions. PMRDs are used primarily to augment posterior motion in wearing and degenerating joints and to slow wear and add support. The typical spine implant fusion construct employs mobile-headed screws that affix to the spinal posterior elements of the spine and span a motion segment with a rigid rod. The rigid rod is then locked into the screw head with a capture device, and biologic bone-healing material is placed across the motion segment to encourage a fusion to develop. Some device companies have substituted a more malleable, flexible or stress-sharing support member for the rigid spanning rod. Even though these implants do not mimic typical spinal motion, they may off-load spinal joint motion and help in pain relief.
Government and insurance regulations stipulate that fusion must accompany placement of spinal implants, but some surgeons circumvent these regulations by placing minimal amounts of bone material or biologic constructs, so the likelihood for solid fusion is low and the support members will still allow motion. The motion, however, may not provide the support the spine needs and might be too restrictive or not restrictive enough. If industry were to advise not using bone for such surgeries, it would be suggesting non-FDA-approved treatments and could be held liable. Most so-called “soft fusion” or nonfusion surgical techniques are considered off-label, and surgeons who use them expose themselves to liability, should a support member fatigue and break. Industry has been supplying these flexible members without directly advocating avoiding fusion, which is why the government is watching fusion outcomes closely. Surgeons who use PMRD implants must code their fees to include a fusion procedure, or insurance companies might not pay.
PMRDs are also being developed by privately funded companies, often with venture capital support. These PMRDs are more sophisticated than existing flexible implants manufactured by large device companies in attempting to customize support for specific posterior motions—flexion and extension, axial rotation, and shear. The FDA demands rigorous scientific methodology in manufacturers’ studies of safety and efficacy. Study protocols, determined in concert with the FDA, are designed to prove that outcomes with the new techniques are equivalent to those in fusion techniques. More recently, insurance companies have been modeling their coverage on Medicare rulings, a distinct hurdle because Medicare only judges technologies that affect its typically older patient population. Medicare also demands that technologies accepted for patient use have outcomes that are superior—not just equivalent—to existing technologies.
These private companies have limited resources, usually only enough money to develop one product to a given stage before requiring more funds. Hence, they must come up with creative patient study designs that have a good chance of statistical success. This practical need has prompted clinical studies in which placement of a structural support device such as a PMRD (typically used for mechanical back pain) is coupled with decompression surgery for leg and buttock pain, or what is considered neurologically mediated pain. This is done because relief of neurologically mediated pain is achieved more consistently, so the surgery has a higher likelihood of outcome success and thus economic success.
In summary, the efficacy of treating low back pain by fusion is being questioned, and attempts are being made to solve structural problems through the use of motion retention devices. As a response to the stringent regulation of experimental technologies, industry has developed implants that can be used off-label but marketed in a way that avoids perception or direct evidence of off-label use, prompting the government to step up its oversight and evaluation of outcomes. In some cases where motion-retention devices are used off-label without fusion material being placed, surgeons may be charged with fraud.
The lack of basic science understanding of spine degeneration, such as knowledge about genetics and biochemical and biophysical causes of pain, may be one reason why engineering structural principles alone have not led to success.