It is increasingly common for representatives of pharmaceutical and medical device companies to attend surgeries for the purpose of observing the use of the company’s product or calibrating the product for the surgeon’s use. The presence of these representatives in the operating room is at times so crucial that without it, the surgery could not proceed [1]. Indeed, the AMA Code of Medical Ethics states that “[m]anufacturers of medical devices may facilitate their use through industry representatives who can play an important role in patient safety and quality of care by providing information about the proper use of the device or equipment as well as technical assistance to physicians” [2]. A few courts have tackled the question of whether liability can attach to medical device or pharmaceutical companies for the actions or omissions of their company representatives who are present in the operating room.
These cases generally fall into two categories. First are those in which plaintiffs allege that the maker of the medical device or pharmaceutical had a duty to prevent the doctor from using its product [1]. Courts have held that a pharmaceutical or medical device company has no duty to supervise or prevent a doctor’s use of those products. Second, plaintiffs have alleged that industry representatives undertook the unauthorized practice of medicine [1]. On this issue, courts have ruled that a company cannot be held liable for the unauthorized practice of medicine merely because its representative is present in the operating room. Rather, the representative must participate in the actual treatment of the patient or exercise medical judgment. The following cases present examples of both theories of liability.
Protecting the Patient-Physician Relationship
Courts have held that pharmaceutical or medical device manufacturers have no duty to supervise a doctor’s use of the company’s products or otherwise prevent a doctor’s use of those products. Such a duty would require the company to interfere in the patient-doctor relationship and exercise medical judgment, both of which the manufacturer is prohibited from doing.
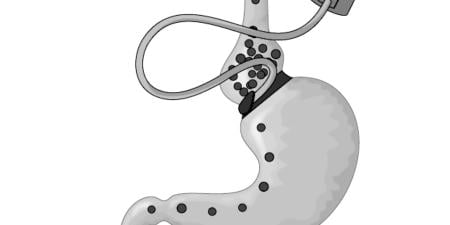
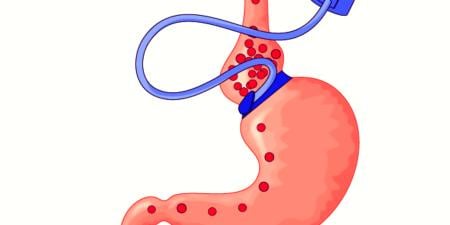
Kennedy v. Medtronic is an Illinois case that involved a death resulting from the cardiac physician’s installation of a Medtronic-manufactured pacemaker into the wrong side of the patient’s heart. Medtronic supplied a clinical specialist who attended the surgery and checked the leads to ensure that they were properly calibrated and functioning. Several months after the surgery, when the unresponsive patient was brought to the hospital, the surgeon discovered his mistake and implanted a new pacemaker. The patient later died of renal and congestive heart failures. The physician admitted that he deviated from the standard of care by inserting the pacemaker lead into the left ventricle [3].
The patient’s daughter sued the device manufacturer, claiming that, by sending a representative to the surgery, Medtronic had voluntarily assumed a duty of care for her father. As such, she argued, Medtronic should have warned the decedent of the dangers inherent in proceeding with the surgery under the conditions present at the clinic. (Part of the conflict revolved around the quality of the health care facility at which the surgery was performed.) Medtronic responded that it had no duty to prevent physician malpractice or guarantee against it. Medtronic further argued that it was exempt from having to warn the decedent or his family of any dangers in proceeding with the surgery [3].
The Illinois Appellate Court found that, for two reasons, Medtronic did not owe the plaintiff’s father a duty of care. First, the decedent’s injuries were not reasonably foreseeable by Medtronic, for Illinois law did not impose a duty to anticipate the negligence of third parties [3]. Second, the burden and consequences of imposing a duty on Medtronic to monitor the conditions under which a physician performs surgery would be substantial because Medtronic would be required to interfere in the patient-physician relationship [1,3]. The court felt that it would be unreasonable—and potentially harmful—to require a clinical specialist such as Medtronic’s representative to delay or prevent a medical procedure simply because she believed the setting to be inappropriate or the doctor unqualified. Requiring such screening would also risk imposing liability on a manufacturer in the event that a manufacturer’s representative refused to provide a device to a physician who the representative deemed unfit to implant the device, and the patient suffered adverse medical conditions as a result. According to the court, the patient’s physician with knowledge of the patient’s medical history is the person best suited to determine a patient’s medical needs [3].
The court also found that Medtronic’s representative had not voluntarily undertaken a duty to do anything more than insure the leads were properly calibrated [1]. This limited and clearly defined role did not entail a duty for the placement of the lead into the correct ventricle of the patient’s heart [3]. Since the representative had not performed her role negligently, liability did not exist [1].
In Swayze v. McNeil Laboratories , the Fifth Circuit Court of Appeals considered whether a pharmaceutical company has a duty to affirmatively prevent a doctor’s misuse of the company’s products. The plaintiff in Swayze was the mother of a boy who died as a result of an overdose of an anesthetic manufactured by McNeil Laboratories [4]. An unsupervised nurse anesthetist, rather than a surgeon or anesthesiologist, had miscalculated the patient’s dosage and administered the anesthetic. Though this use of unsupervised nurse anesthesists was revealed to be a statewide practice, McNeil denied any knowledge of the practice. The plaintiff alleged that McNeil knew or should have known of this practice, and so had a duty to: (1) warn patients directly of the risk of misuse, (2) take additional steps to enforce the requirement that only a physician administer the anesthetic, or (3) withdraw the anesthetic from the market [1, 4].
The court found that McNeil had no duty to enforce its warnings, much less directly warn certain patients, reasoning that it would hesitate to encourage or require a drug manufacturer to intervene in an established patient-physician relationship [4]. It would be impractical and unrealistic, the court stated, to expect drug manufacturers to police individual operating rooms to determine which physicians adequately supervise their surgical teams [1, 4]. The court took note that the harm in this case did not come from adverse side effects of the drug but from the unsupervised administration of the drug [4].
The court also held that McNeil also had no duty to remove the anesthetic from the market [4]. The court reasoned that the problem lay with individual physicians, not the drug itself, and that manufacturers cannot control the individual practices of the medical community [1].
Differentiating between Presence and Practice
Courts have held that companies are not liable for the unauthorized practice of medicine merely because their representatives are present in the operating room. Rather, the representative must participate in the actual treatment of the patient or the exercise of medical judgment for liability to attach.
In People v. Smithtown General Hospital , the Supreme Court of New York considered whether the actions of a general sales manager, who scrubbed in on a surgery to help remedy a problem with his company’s prosthetic hip, constitute the practice of medicine [5].
Smithtown involved a total hip arthroplasty gone awry and a sales manager’s attempt to remedy the situation. The sales manager who supplied the instrumentation was present during the initial surgery and was called back after a post-operative x-ray showed that the patient’s hip joint had been dislocated. The sales manager returned in time to scrub in and observe the follow-up procedure. The surgeon attempted to remove the prosthesis with a mallet, but failed. At that point, the general manager offered to lend a hand and was ultimately successful in removing the prosthesis with the surgeon’s mallet [5].
Before the prosthetic could be reinserted, it had to be cleaned to remove cement that had cured in it. In an effort to clean the prosthesis, the surgeon fractured the patient’s femur. As tension in the room rose and the surgeon contemplated another course of action, the sales manager said that he could “fix the thing” (i.e., the prosthetic hip). With the surgeon’s consent, he spent more than 3 hours removing the cement with tiny curettes, during which time the surgeon reportedly left the operating room. The general manager also treated the patient’s broken femur. When asked whether he or the physician put the prosthetic device in, the general manager replied, “I did.” The general manager had not attended high school or college and had no training in paramedical techniques; his knowledge came “exclusively from reading orthopedic journals, looking at training films, and from implanting prostheses in cadaver bones as a training exercise” [5].
Interestingly, the plaintiff did not bring action against either the general manager or the medical device manufacturer, choosing to sue only the health care professionals who were present during the surgery. The health care professionals were charged with acting in concert with one another in the commission of second-degree assault—not medical malpractice—for allegedly allowing the general manager to participate in a meaningful way in a surgical procedure without the patient’s consent [5].
The court defined the practice of medicine as “diagnosing, treating, operating or prescribing for any human disease, pain, injury, deformity, or physical condition” [5]. The court held that, in this case, the physician “abdicated his role as surgeon in that operating room and permitted the judgment and skills of a layman to prevail.” The general manager’s involvement in the procedure “extended far beyond instruction as to the use or manner of implant of the device he sold.” The court held that a jury could conclude that the salesman’s actions constituted unlawful engagement in the practice of medicine [1, 5]. With regard to the charge of assault, the court held that, while the defendants’ conduct might encourage a malpractice suit, it did not carry the requisite “unlawful intent” sufficient to warrant criminal conviction [5].
References
-
Summerhill MJ, Chandler AM. Company representatives in the operating and treatment room: how to navigate the ever-expanding theories of liability for medical device and pharmaceutical companies. DePaul J Health Care L. 2009;12(2):253.
-
American Medical Association. Opinion 8.047 Industry representatives in clinical settings. Code of Medical Ethics. Chicago, IL: American Medical Association; 2008. http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion8047.shtml. Accessed January 7, 2009.
-
Kennedy v Medtronic, Inc., 366 Ill App 3d 298 (2006).
-
Swayze v McNeil Laboratories, Inc., 807 F2d 464 (5th Cir. 1987). See also: Labzda v Purdue Pharma, LP, 292 F Supp 2d 1346, (SD Fla 2003).
-
People v Smithtown General Hospital, et al , 402 NYS 2d 318 (NY 1978).