Despite today’s technically advanced approaches and methods for treating the human body, the end goal of medicine remains the same as it has been from the earliest of times, even before the existence of a Hippocratic Oath. In fact, as one source says, “an innate instinct for self-preservation [exists] among all mammals,” and there is no reason to doubt that early Homo sapiens possessed the rudimentary skills to try to preserve life in case of an injury [1]. As humans moved away from the hunter-gatherer society and into settled social groups, individuals focused their energies on specific tasks, and occupations began to take shape. Medicine followed the societal trend of specialization and, as knowledge grew and technology advanced, the number of different ways to treat the same problem proliferated. Contemporary medicine encompasses many types of care, and today’s physicians compartmentalize the body, concentrating on small areas and specific modalities of treatment.
Medicine’s two branches—the less invasive medical methods and the more invasive surgical methods—have been around since before the existence of written language. Surgery, however, was not viewed as belonging to the same sphere as medical treatments until relatively recently, and, even now, a sharp distinction exists between surgeons and other medical doctors. Analyzing the history of surgery can help explain the separation between medical and surgical treatments and why the two fields, although viewed quite differently, fit under the umbrella of medicine.
Surgery—i.e., the use of physical objects in a normally traumatic way to provide treatment—is not new. Evidence exists that circumcisions were done in Ancient Egypt using sharpened rocks and crude stone instruments as long ago as 10,000 BCE [2]. Skulls from ancient civilizations show holes to excavate clots and relieve abnormal intracranial pressure, a process known as trephination. These early peoples had some idea that elements in the body can cause harm and that their removal could decrease pain. While the methods worked often enough to encourage their continued use, most of the time they made the situation worse. For illness with no obvious cure, there was always prayer. Native Americans were well known for using surgical methods in conjunction with religious intervention to heal wounds received in war [3].
The separation of religion from medicine occurred in Ancient Greece [4]. Not only did the Greeks rely on physical methods of treatment and evaluate them empirically, they tried to understand why people were getting sick. Their answer—the Theory of the Four Humors/Elements and how the balance of these humors affects health—governed treatments during that time period and became the basis of today’s internal medicine.
Greek physicians dabbled in surgery but mostly turned to less invasive treatments such as ingestible herbs and topical applications of salves and poultices. Hippocrates preached about the merits of a “suitable diet, rest, and exercise” [5]. While surgery was sometimes effective, especially in the removal of foreign objects, it was not the focus of physicians’ practice. In fact, early versions of the Hippocratic Oath warned physicians against the use of surgery [6]. The warning was meant to force doctors to acknowledge their limitations and also reflects the fact that so little was known about surgery at the time that it was considered unwise for physicians to engage in it.
Like other formal studies, surgery and medicine took a step backwards during the medieval era, surviving in limited areas of the known world, such as Southern Italy, the Byzantine Empire, and the Arabian countries. It was not until the Renaissance that medical knowledge started to flourish again. New universities gave those who wanted to practice medicine a forum for practical as well as theoretical learning through public dissections and an emphasis on the importance of anatomy. The Renaissance approach to learning stressed “seeing to believe,” and firsthand accounts, rather than what was passed down from previous generations, came to be considered the basis of knowledge. Concepts of physiology were formed “as the secrets of anatomy began to be revealed in even greater detail” [7]. Both medicine and surgery increasingly emphasized empirical observation, a path that would lead them to the scientific disciplines they are today in Western societies.
Universities established during the Renaissance did not offer formal education to surgeons, however. The manual nature of surgical work caused it to be viewed as a trade rather than an art and thus unsuitable for teaching in universities. Instead, surgical skills were learned by apprenticeship. Though leading French and Spanish physicians were often experts in anatomy and practiced both gross dissection and as well as some surgery, their real interests lay strictly in the field of medicine. Most physicians still felt that “there [was] no more science in surgery than in butchering” [8]. The same was true “in England, [where] people never accepted…that surgeons were the equals of doctors…and the internists…formed an association which eventually became the Royal College of Physicians.” [9]. To help bolster their standing and give them some credibility and political power, the surgeons joined the Company of Barbers and formed the United Company of Barber Surgeons in 1540, a group dedicated to performing surgery and extracting teeth [10].
The distinction between surgeons and physicians was maintained in hospitals, the establishment of which began during medieval times and continued through the Renaissance. At first, hospitals were small places, often located in churches, but the 12th and 13th centuries saw the formation of many large hospitals throughout Europe, especially in London [11]. Hospitals gave physicians a specific place in which to practice. In contrast, the barber-surgeons plied their trade in commercial establishments, identifying themselves with the red-and-white-striped poles still used by some barbers today.
In England, the reputation of the surgeons began to rise slowly during the Renaissance, as they gained the respect of various kings and made breakthroughs like raising the success rate of Caesarean operations. Surgery also owes much to Ambroise Pare, regarded by many as one of the Renaissance’s greatest surgeons. He trained with the barber-surgeons and became a field surgeon in the French army. He wrote several books on anatomy and wound treatment in the field. Though he had no formal education, he was made a member of the College of Saint Come in Paris, an unheard-of event at the time. Eventually Pare became the personal physician to four successive French kings [12].
In addition to improvements in surgery itself, two medical advances—effective anesthesia and antiseptic techniques—greatly benefited patients undergoing surgery. Previously, hashish, mandrake, and opium were the only drugs available to induce analgesia. Into the late 18th and early 19th centuries, many patients died from the intoxication effects. Producing effective analgesia and paralysis with less risk increased the willingness of patients to undergo surgery. Joseph Lister’s mid-19th-century advances in bacteriology, the prevention of hospital-induced infections, adequate prevention and treatment of wound infections, and antiseptic methods of performing surgery helped decrease the complication rate, increasing the likelihood hospital patients would actually benefit from surgical treatments.
Eventually, surgeons were given more formal standing and established respected professional societies. In 1745, English barbers and surgeons parted ways and formed separate groups; the Company of Surgeons received its royal charter in 1800, expanding from the Royal College of Surgeons in London to the Royal College of Surgeons of England in 1843 [13, 14]. By the beginning of the 19th century, training had unified so that surgeons and medical doctors went through the same medical school or university training, received the same degree authorizing them to practice medicine, and practiced in the same institutions. For the most part, surgeons and internists are now both known as “doctors.” Even now, some separation remains. In England, internists are given the title “Doctor” while surgeons are often referred to as “Mister,” a throwback to the age of barber-surgeons.
Many of the 20th century’s greatest life-saving interventions—from organ transplantation and open heart surgery to laser and laparoscopic surgery—were surgical techniques and devices, and the technological explosion of the 21st century leaked into surgery, leading to procedures never previously thought possible. Perhaps the words of one medical historian are correct: “Surgeons have always been quick to adapt to new technology…it should perhaps be noted that physicians were rather more tardy” [15].
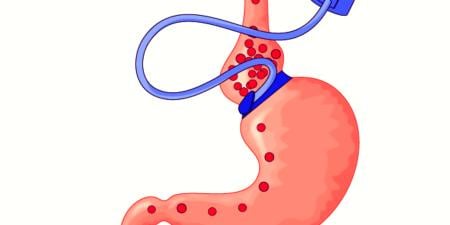
As surgery continues to advance, cases that involve minimal access, laparoscopic instruments, and even robotics are becoming common. Internists have even begun to take up certain surgical techniques. Cardiologists can place stents in the coronary arteries and perform femoral cut-downs to gain access to the aorta; gastroenterologists use endoscopes to look at and treat almost all the parts of the digestive tract and to place feeding tubes; and interventional radiologists drain abscesses, insert and remove feeding tubes, break up clots, and even fix aortic aneurysms using various endovascular techniques [16]. Internists and other medical specialists can no longer be said to diagnose and treat illnesses using only their knowledge of physiology and pharmacology.
Is surgery’s transition from outsider to insider to “top dog,” so to speak, beneficial? A surgeon’s salary is almost directly proportional to the number of procedures he or she completes. Thus, a surgeon has a financial self-interest that may come ahead of the patient’s well-being. At the same time, a medical doctor who uses an invasive procedure will earn substantially more than he or she would for delivering less invasive care. If anything, some internists may have a greater incentive for using surgically based procedures. Whether this trend benefits the patient and should be embraced or rejected is a question that requires more thorough analysis. But surgery and medicine are joining hands to find new and better ways of treating patients. It is time to stop defining a patient’s treatment as either surgical or medical and to use the two approaches in conjunction to provide the best care possible.
References
-
Ellis H. A History of Surgery. London: Greenwich Medical Media; 2002:3.
-
Ellis 5.
-
Rutkow IM. American Surgery: An Illustrated History. Philadelphia: Lippincott-Raven Publishers; 1998:3-7.
-
Ellis 20.
-
Ellis 21.
-
Hippocratic Oath. Encyclopedia Britannica Online. http://www.britannica.com/EBchecked/topic/266652/Hippocratic-oath. Accessed January 20, 2010.
-
Haeger KM. The Illustrated History of Surgery. 2nd ed. London: Harold Starke Publishers; 2000:117.
-
The history of surgery: a brief account of how an esteemed art and science came to be what it is today. Saint Louis University School of Medicine. http://www.slucare.edu/pdf_nov5/history_surgery.pdf. Accessed December 15, 2009. Page 8.
-
Haeger 101.
-
Surgery. Encyclopedia Britannica Online. http://www.britannica.com/EBchecked/topic/575155/surgery. Accessed January 20, 2010.
-
Mayeaux EJ Jr. A history of Western medicine and surgery. Department of Family Medicine and Comprehensive Care, Louisiana State University Health Sciences Center. http://lib-sh.lsuhsc.edu/fammed/grounds/history.html. Accessed December 15, 2009.
-
Ambroise Pare. Encyclopedia Britannica Online. http://www.britannica.com/EBchecked/topic/443426/Ambroise-Pare. Accessed January 20, 2010.
-
Royal College of Surgeons of England. History of the College. Royal College of Surgeons of England. http://www.rcseng.ac.uk/about/history. Accessed January 20, 2010.
-
Blandy JP, Lumley JSP. The Royal College of Surgeons of England: 200 years of history at the millennium. London: Wiley-Blackwell; 2000:26.
-
Ellis 251.
- Mueller RL, Sanborn TA. The history of interventional cardiology: cardiac catheterization, angioplasty, and related interventions. Am Heart J. 1995;129(1):146-172.