Opinion 2.077 – Ethical Considerations in International Research
Physicians, either in their role as investigators or as decision-makers involved in the deliberations related to the funding or the review of research, hold an ethical obligation to ensure the protection of research participants. When the research is to be conducted in countries with differing cultural traditions, health care systems, and ethical standards, and in particular in countries with developing economies and with limited health care resources, US physicians should respect the following guidelines:
(1) First and foremost, physicians involved in clinical research that will be carried out internationally should be satisfied that a proposed research design has been developed according to a sound scientific design. Therefore, investigators must ascertain that there is genuine uncertainty within the clinical community about the comparative merits of the experimental treatment and the one to be offered as a control in the population among which the study is to be undertaken. In some instances, a three-pronged protocol, which offers the standard treatment in use in the US, a treatment that meets a level of care that is attainable and sustainable by the host country, and a placebo (see Opinion 2.075, "Surgical Placebo’ Controls"), may be the best method to evaluate the safety and efficacy of a treatment in a given population. When US investigators participate in international research they must obtain approval for such protocols from U.S. Institutional Review Boards (IRBs).
(2) IRBs, which are responsible for ensuring the protection of research participants, must determine that risks have been minimized and that the protocol’s ratio of risks to benefits is favorable to participants. In evaluating the risks and benefits that a protocol presents to a population, IRBs should obtain relevant input from representatives from the host country and from the research population. It is also appropriate for IRBs to consider the harm that is likely to result from forgoing the research.
(3) Also, IRBs are required to protect the welfare of individual participants. This can best be achieved by assuring that a suitable informed consent process is in place. Therefore, IRBs should ensure that individual potential participants will be informed of the nature of the research endeavor and that their voluntary consent will be sought. IRBs should recognize that, in some instances, information will be meaningful only if it is communicated in ways that are consistent with local customs.
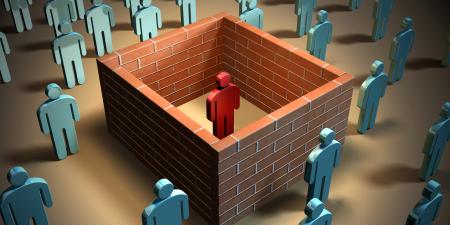
(4) Overall, to ensure that the research does not exploit the population from which participants are recruited, IRBs should ensure that the research corresponds to a medical need in the region where it is undertaken. Furthermore, they should foster research with the potential for lasting benefits, especially when it is undertaken among populations that are severely deficient in health care resources. This can be achieved by facilitating the development of a health care infrastructure that will be of use during and beyond the conduct of the research. Additionally, physicians conducting studies must encourage research sponsors to continue to provide beneficial study interventions to all study participants at the conclusion of the study.