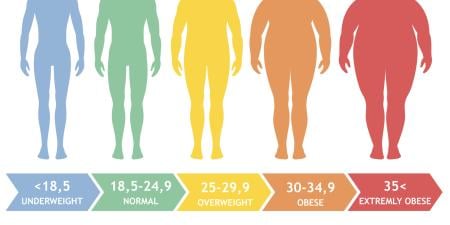
Certain aspects of the obesity epidemic in United States are not in question. We know, for instance, that rates of obesity (defined as BMI equal to or greater than 30) for all sociodemographic groups have risen to a startling degree in the past 50 years, and that 33.8 percent of U.S. adults are classified as obese, as are 16.9 percent of children [1, 2]. The health and psychosocial effects of obesity also are well-documented and include various forms of cancer, diabetes mellitus, cardiovascular disease, osteoarthritis, sleep apnea, asthma, non-alcoholic fatty liver disease, social stigma, and many others [3-6]. Generally accepted methods for decreasing body mass include consuming fewer calories and increasing physical activity.
The solutions to this epidemic of obesity are less clear. Although many individual-level interventions to reduce weight often show impressive short-term results, diet and activity changes are generally not maintained.
The magnitude of the rise in obesity in the U.S., the failure of interventions to sustain reductions in body mass, and the implications for public health—as well as costs to the U.S. economy in terms of health care, absenteeism, and increased disability rates [7-9]—are profound. These statistics and their implications have led to calls for increased intervention by policymakers at all levels of government to improve Americans’ diet and activity level and reduce weight [10-12].
Is it desirable that policymakers play a role in what people eat or how active they are? Many think not. Dietary behavior—and to some extent, physical activity—are intensely personal and are influenced by numerous factors, including genetics, biology, and environment [13]. At issue is the perpetual tension of pluralistic democracies: identifying an appropriate balance between individual liberty and the well-being of the community as a whole. This tension is a common concern for the field of public health, with its focus on the population, rather than on the individual [14]. (Parsing the balance between individual and community rights is not restricted to public health and may be seen in many other policy fields such as, notably and currently, national security.) Certainly, policy action to improve population health has ample precedent. Examples include seat belt laws, vaccinations, speed limits, water fluoridation, vitamin fortification of food, alcohol avoidance while driving, and tobacco taxes and regulations.
So, should government intervene in the case of obesity? In his 1859 treatise On Liberty, John Stuart Mill argued that the only justification for infringing upon personal liberties was prevention of harm to others. This perspective has become dominant in political thinking in the United States [15]. Even freedom of speech—one of the most cherished civil liberties in the U.S.—may be curtailed in certain cases. One may not shout “fire” in a crowded theater, for instance, without justification. Economics offers more detailed criteria for the circumstances under which policy intervention is warranted, in some ways expanding and codifying Mill’s notion of harm to others.
The views of Mill and economists are by no means the only perspectives on which to base the need for policy (intervening to address inequality of opportunity and social injustice are other compelling reasons), but, given their impact on political thought and policy justification [16], they make a useful starting point from which to examine the rationale for public policies regarding obesity.
According to conventional economic theory of perfect markets, the collective decisions of individual, rational actors seeking to maximize utility (i.e., their happiness) create “the invisible hand” of the market, which distributes goods in the most efficient manner [17]. In this case, to be rational means to be capable of assessing one’s own best interests, whether or not others agree with those assessments. However, under certain circumstances, the market “fails,” with resulting inefficiencies. Policy solutions are considered warranted in the event of “market failure.” Market failure can occur when there is information asymmetry (in which one party in a transaction has more information than the other), when there is a monopoly (in which one company or group of companies is so large it can dictate terms to the market), when there are externalities (positive or, more often, negative effects that transactions may have on others), and when there is an attempt to create or maintain public goods, which, though their existence benefits all, few may be motivated to fund voluntarily (e.g., national parks) [16-19].
Given these parameters, does widespread obesity in the U.S. provide a sufficiently strong basis for intervention in the market? Evidence suggests that it does, on three grounds: (1) imperfect rationality (which, though it is not universally accepted as an instance of market failure, undermines fundamental assumptions about the functioning of the market); (2) asymmetric information, and (3) financial externalities.
1. Imperfect rationality. It is well accepted in economic literature that children are not rational actors. In other words, they are not capable of judging their own welfare accurately [20]. Indeed, the brain’s prefrontal cortex—responsible for executive-function activities such as planning and emotional and impulse control—continues to develop throughout adolescence [21, 22]. Recognizing this, there are many instances where society restricts activities for children to a far greater degree than in adults, such as with smoking and alcohol consumption. Imperfect rationality in children has been proposed as an example of market failure in the context of obesity [20, 23-25].
Research from the emerging field of behavioral economics suggests that adults often depart from rational behavior in “highly systematic and predictable ways” [26]. Perhaps most relevant to diet and activity behavior is research from behavioral economics on three manifestations of imperfect rationality: the impact of default options, behavior that is inconsistent over time, and behavior that may be subconscious.
Work in behavioral finance demonstrates that default options greatly influence behavior. For example, automatic enrollment—or not—in 401(k) plans dramatically alters plan participation, which would not be the case if financial investment behavior were fully rational [27, 28]. Similarly, a default food environment that is high in calories and low in nutrients may well affect dietary behavior, and a default physical environment that is not conducive to physical activity may well reduce activity behavior. Research shows a strong connection between food and activity environments and corresponding behavior [29-34], although more longitudinal studies are needed to infer causality.
Another common departure from rational behavior is inconsistency over time. As Thaler and Sunstein have noted, “in the context of inter-temporal choice, people exhibit dynamic inconsistency, valuing present consumption much more than future consumption. In other words, people have self-control problems” [35]. Inconsistency is common in diet and activity behavior; people may value good health, but often make poor short-term diet, activity, or other choices that are out of line with their long-term health goals [36].
Finally, the concept of rational choice assumes fully conscious decision making. However, research suggests that at least some eating behavior may be subconscious [36]. Some innovative recent research by nutritionists—such as studies investigating the relationship between container size and consumption and the effects of self-refilling bowls on diners’ intake of soup [37-40]—suggests that dietary choices are often influenced by social and environmental cues and that many of these choices are subconscious.
2. Asymmetric information. In the context of obesity, there is evidence of information failure, particularly underprovision of information. Cawley has said that government information about diet and physical activity is “underprovided and disseminated” compared with that provided by food and beverage manufacturers [24]. Accessing and using appropriate dietary information may be difficult and time consuming. People may be unaware, for example, of the caloric content of the food they consume; nutrition labels on packaged foods provide calorie and other macronutrient information, but this information may be difficult for some consumers to understand and use [41]. Moreover, nutritional information is less readily available for food prepared outside the home [42], consumption of which has increased greatly in the past several decades [43]. Reduced access to relevant information inhibits accurate assessment of one’s welfare.
3. Financial externalities. Research shows that widespread obesity increases costs related to health care, as well as absenteeism, disability, and reduced productivity at work [7, 44, 45]. Indeed, medical costs related to obesity were recently estimated at as much as $147 billion per year [9]. Further, estimates of lifetime health care costs, assessing the medical-related costs over a lifetime, show that any earlier mortality due to high BMI does not offset health care costs. In fact, lifetime health care costs may average as much as $29,000 more for those with BMIs over 35 than for those of normal weight [8]. Importantly, those who are obese often do not bear the full cost associated with increased weight, unless their insurance plan is cost-adjusted for weight status [46]. Instead, increased health care costs are borne by others, such as employers, those in the insurance risk pool, and taxpayers, depending on the specific plan and health insurance status.
The rationale for policy intervention to reduce obesity rates therefore appears compelling. But what exactly should be done? Adequate discussion of appropriate policy interventions is not possible here, but the following comments may provide starting points for effective decision making. Justification for intervening in the case of children is particularly strong, and precedent suggests that society will more readily accept appropriate restrictions to youth behavior. Adults are less likely to accept the kinds of direct restrictions often considered for children. Instead, policies that harness insights from behavioral science may be especially helpful in nudging behavior towards improvements in activity and diet. Examples of effective policies might include those that:
- alter the environments in which people make diet and activity decisions so that the easiest option is the most healthy;
- create short-term incentives that align with people’s long-term health goals; and
- improve availability of relevant information to facilitate informed, and fully conscious, decision making.
Other effective policies might address inequality of opportunity regarding optimal diet and activity behavior. For example, availability of and access to nutritious foods are restricted in many communities in the U.S. [47]. Rigorous evaluation of policy interventions will be required to assess their effectiveness in altering behavior.
Current rates of obesity in the U.S. and their health and economic implications are sobering. Policymakers at all levels of government are in a position to enact community and other environmental changes needed to support improvements in diet and activity behavior, thereby improving health outcomes for all Americans.
References
- Flegal KM, Carroll MD, Ogden CL, Curton LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303(3):235-241.
- Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010;303(3):242-249.
- Dietz W. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101(3 Pt 2):518-525.
- Kopelman P. Health risks associated with overweight and obesity. Obes Rev. 2007;8(Suppl 1):13-17.
- Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523-1529.
- Pi-Sunyer FX. The obesity epidemic: pathophysiology and consequences of obesity. Obes Res. 2002;10(suppl 2):97S-104S.
- Finkelstein E, Fielbelkorn C, Wang G. The costs of obesity among full-time employees. Am J Health Promotion. 2005;21(1):45-51.
- Finkelstein EA, Trogdon JG, Brown DS, et al. The lifetime medical cost burden of overweight and obesity: implications for obesity prevention. Obes (Silver Spring). 2008;16(8):1843-1848.
- Finkelstein EA, Trogden JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Aff (Millwood). 2009;28(5):w822-w831.
-
Institute of Medicine. Preventing Childhood Obesity: Health in the Balance. 1st ed. Washington, DC; National Academies Press: 2005.
-
Institute of Medicine. Local Government Actions to Prevent Childhood Obesity. Washington DC: National Academies Press; 2009.
-
Trust for America's Health. F as in fat: how obesity policies are failing in America. http://healthyamericans.org/reports/obesity2009/Obesity2009Report.pdf. Accessed January 10, 2010.
- Johnson-Asker WL, Fisher RA, Yaroch AL. Decision making in eating behavior: state of the science and recommendations for future research. Ann Behav Med. 2009;38(Suppl 1):S88-S92.
- Kass NE. An ethics framework for public health. Am J Public Health. 2001;91(11):1776-1782.
-
Stone D. Policy Paradox: The Art of Political Decision Making. 3rd ed. New York: W.W. Norton & Company; 2002.
-
US Office of Management and Budget. Circular A-4. http://www.whitehouse.gov/omb/circulars/a004/a-4.pdf. Accessed January 16, 2010.
- Bator FM. The anatomy of market failure. Q J Econ. 1958;72(3):351-379.
-
Friedman LS. The Microeconomics of Public Policy Analysis. Princeton, NJ: Princeton University Press; 2002.
-
Weimer DL, Vining AR. Policy Analysis: Concepts and Practice. 4th ed. Upper Saddle River, NJ: Prentice Hall; 2005.
-
McCormick B, Stone I, Corporate Analytical Team. Economic costs of obesity and the case for government intervention. Obes Rev. 2007;8 Suppl 1:161-164.
- Best JR, Miller PH, Jones LL. Executive functions after age 5: changes and correlates. Dev Rev. 2009;29(3):1800-200.
- Casey BJ, Getz S, Galvan A. The adolescent brain. Dev Rev. 2008;28(1):62-77.
- Anderson PM, Butcher KF, Levine PB. Economic perspectives on childhood obesity. Econ Perspect. 2003;27(3):30-48.
- Cawley J. An economic framework for understanding physical activity and eating behaviors. Am J Prev Med. 2004;27(3 Suppl):117-125.
- Moodie R, Swinburn B, Richardson J, Somainin B. Childhood obesity—a sign of commercial success, but a market failure. Int J Pediatr Obes. 2006;1(3):133-138.
-
Just DR. Behavioral economics, food assistance, and obesity. Agricultural Resource Econ Rev. 2006;35(2):210.
- Choi JJ, Laibson D, Madrian BC, Metrick A. Optimal defaults. Am Econ Rev. 2003;93(2):180-185.
- Madrian BC, Shea DF. The power of suggestion: inertia in 401(k) participation and savings behavior. Q J Econ. 2001;116(4):1149-1187.
- Frank LD, Kavage S. Urban planning and public health: a story of separation and reconnection. J Public Health Manage Pract. 2008;14(3):214-220.
- Handy SL, Cao X, Mokhtarian PL. The causal influence of neighborhood design on physical activity within the neighborhood: evidence from Northern California. Am J Health Promotion. 2008;22(5):350-358.
- Saelens BE, Handy SL. Built environment correlates of walking: a review. Med Sci Sports Exerc. 2008;40(7 Suppl):S550-S566.
- Morland K, Wing S, Diez Roux A. The contextual effect of the local food environment on residents’ diets: the Atherosclerosis Risk In Communities study. Am J Public Health. 2002;92(11):1761-1768.
- Popkin BM, Duffey K, Gordon-Larsen P. Environmental influences on food choice, physical activity and energy balance. Physiol Behav. 2005;86(5):603-613.
- Larson N, Story M. A review of environmental influences on food choices. Ann Behav Med. 2009;38(Suppl 1):S56-S73.
-
Thaler R, Sunstein CR. Libertarian paternalism. Am Econ Rev. 2003;93(2):175-179:176.
-
Just DR, Payne CR. Obesity: can behavioral economics help? Ann Behav Med. 2009;38 Suppl 1:S47-S55.
- Wansink B, Kim J. Bad popcorn in big buckets: portion size can influence intake as much as taste. J Nutr Educ Behav. 2005;37(5):242-245.
- Wansink B, Painter JE, North J. Bottomless bowls: why visual cues of portion size may influence intake. Obes Res. 2005;13(1):93-100.
- Wansink B, Payne CR, North J. Fine as North Dakota wine: sensory expectations and the intake of companion foods. Physiol Behav. 2007;90(5):712-716.
- Wansink B, Sobal J. Mindless eating: the 200 daily food decisions we overlook. Environ Behav. 2007;39(1):106-123.
- Cowburn G, Stockley L. Consumer understanding and use of nutrition labelling: a systematic review. Public Health Nutr. 2005;8(1):21-28.
- Wootan MG, Osborn M. Availability of nutrition information from chain restaurants in the United States. Am J Prev Med. 2006;30(3):266-268.
-
Variyam JN. Nutrition labeling in the food-away-from-home sector: an economic assessment. Washington, DC: USDA Economic Research Service; 2005.
- Thorpe KE. The rise in health care spending and what to do about it. Health Aff (Millwood). 2005;24(6):1436-1445.
- Sturm R. The effects of obesity, smoking and drinking on medical problems and costs. Health Aff (Millwood). 2002;21(2):245-253.
-
Bhattacharya J, Sood N. Health insurance and the obesity externality. In: Bolin K, Cawley J, eds. The Economics of Obesity. Oxford: Emerald Group Publishing Limited; 2006. Advances in Health Economics and Health Services Research; vol. 17: 279-318.
-
Beaulac J, Kristjansson E, Cummins S. A systematic review of food deserts, 1966-2007. Prev Chronic Dis. 2009;6(3):A105. http://www.cdc.gov/pcd/issues/2009/jul/08_0163.htm. Accessed January 22, 2010.