In putting together an issue of a medical ethics journal, there are two starting points from which one can work: ethical principles and clinical situations. In the first approach, one chooses an ethical idea and then identifies clinical situations in which that principle plays a central role; those situations can be the jumping-off points for case discussions and other articles. This approach, one could posit, might be preferred by ethicists with backgrounds in philosophy or some other nonclinical field, who have a primary interest in principles and view the clinical world as a realm in which those principles are applied. An example of this approach is the August 2009 issue of Virtual Mentor on the theme of Problematizing the Principle of Autonomy: autonomy, the bioethics concept, was taken as central and its clinical implications examined from there.
The alternative is to begin in the clinical realm, either an area of practice (e.g., surgery) or a situation (e.g., the end of life), and then seek to identify ethical challenges inherent in the practice or situation. A well-executed example of this approach is the Virtual Mentor issue from February 2010 on Ethics and Innovation in Surgery, edited by Catherine Frenkel, a medical student at Albany Medical College (and, coincidentally, a former classmate of mine). This alternative is particularly attractive to clinicians, who encounter ethical dilemmas in practice and seek concepts to help resolve them.
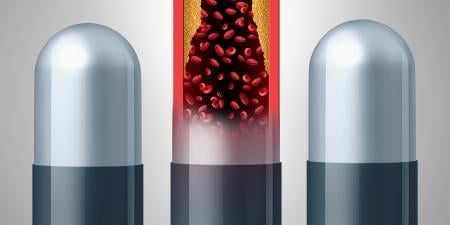
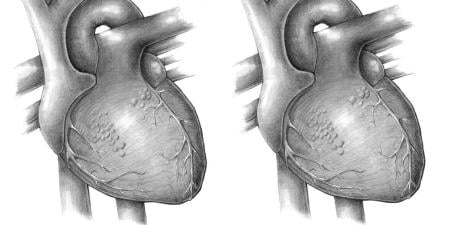
As a future clinician in, with luck, the field of internal medicine, I was attracted to the latter approach when developing this issue of Virtual Mentor. Cardiovascular medicine, a specialty area within internal medicine, is the focus of the issue, and the ethics topics it confronts within the field range considerably—another benefit of the clinical lens. Cardiovascular medicine offers particularly fertile ground, from a clinical standpoint, on which to have an ethics discussion because we are currently contending with the results of what many consider to be a revolution in the field. While specialties like neurology and genetics (another research interest of mine) are still waiting for the big collective breakthroughs in their modern incarnations, cardiology has just recently undertaken a massive leap forward. The data we have about cardiovascular conditions like hypertension, heart failure, and arrhythmias and the corresponding pharmacologic, interventional, and device-based diagnostic and treatment modalities—statins, beta-blockers, anti-arrhythmics, cardiac catheterization, prosthetic valves, cardiac ablation, pacemakers, implantable cardioverter-defibrillators, echocardiography, stress testing, and so on—have exploded in recent decades.
This onslaught of new techniques and related clinical data has put us in the position of feeling as if we have fantastic capabilities, and it is in such a situation that ethics is most important. Indeed, as a matter of historical fact and philosophical axiom, new ethical challenges arise precisely when either our intellectual understanding of or our ability to intervene in a given situation takes a big step forward. This is exactly where the field of cardiovascular medicine stands today.
In this issue of Virtual Mentor—Ethical Challenges in Modern Cardiovascular Medicine—we first examine three dilemmas facing practicing cardiologists today through clinical case commentaries. James N. Kirkpatrick, MD, a clinician and ethicist at the University of Pennsylvania School of Medicine, discusses a case of recurrent infective endocarditis in an intravenous drug user, taking us beyond the knee-jerk feelings many physicians have when they encounter a patient who appears wholly responsible for his or her own medical problems. Dr. Kirkpatrick also considers the widespread concern about inefficient use of medical resources in an American system burdened with astonishing high costs. The clinical pearl, on infective endocarditis, is contributed by Arash Aghel, MD, a fellow in cardiovascular medicine, and Sri Madan Mohan, MD, a cardiologist and assistant professor of medicine, both at University Hospitals Case Medical Center.
Karen Uhlenhuth, a journalist and scientific writer at Children’s Mercy Hospital Bioethics Center, Angira Patel, MD, a fellow in pediatric cardiology at Children’s Memorial Hospital and a clinical medical ethics fellow at the University of Chicago, and John Lantos, MD, a pediatrician and director of the Children’s Mercy Bioethics Center in Kansas City, weigh the costs and benefits of aggressive interventions—specifically statins—to control cardiac risk factors in the pediatric population and the effects interventions like these may have on incentives for less aggressive treatment such as lifestyle modifications.
David Brush, MD, a pulmonary medicine fellow and trained ethicist, and Crystal E. Brown, MD, an internal medicine resident, both at the University of Chicago, discuss the ever-important topic of defensive medicine, specifically with respect to the hot-button issue of possible acute coronary syndrome and cardiac catheterization. On a related topic, the health law section—by Ryan Bailey and Kristin E. Schleiter, JD, LLM, under the auspices of the AMA’s ethics group—recounts the facts and court decision in Riegel v. Medtronic, Inc., a case brought against device-maker Medtronic when one of its cardiac catheters burst during use.
We then turn from individual practice issues to topics concerning the field and its relationship to government, industry, and public health. The journal discussion, by Katherine R. Schlosser, a fourth-year medical student at Case Western Reserve University School of Medicine, and me, analyzes a recent article from Circulation documenting health disparities in cardiology consultation rates between different patient cohorts.
Jeremy A. Greene, MD, PhD, an internist and assistant professor in the Department of the History of Science of Harvard University, chronicles the evolution of the marketing strategy and subsequent scandals of the blockbuster statin Lipitor.
A pair of articles look at the health behaviors of individuals and what interventions from clinicians and government, if any, are appropriate. Mark E. Votruba, PhD, an associate professor of economics and medicine at Case Western Reserve University, provides an economic take on public health measures aimed at altering American dietary choices, using the controversial New York City ban on trans fat as a case study. Jane S. Jue, MD, MSc, an internist who is currently a Robert Wood Johnson Foundation Clinical Scholar at the University of Pennsylvania, identifies the multiplicity of socioeconomic and individual contributors to heart health and disease and the changes that could help reverse the trend toward disease in the United States.
Finally, Stephanie King, a student at The Cleveland Institute of Art, and Sarah Cross, MD, a resident physician in obstetrics and gynecology at Yale-New Haven Hospital, provide art and poetry on the iconography of the heart.
In the end, the goal of this issue is to serve both clinicians—cardiologists in particular—and nonclinician ethicists. For physicians, it can function as a manual of sorts—a guide to a more nuanced understanding of the ethical principles at stake in situations that arise in their practice and in their field. For ethicists trained in philosophy, the law, and other nonmedical fields, the issue can illustrate how ethical questions emerge in practice as our research and clinical capabilities expand. Perhaps in no specialty is this more necessary than in cardiovascular medicine.