The University of Washington School of Medicine (UW SOM) is a regional primary care medical school serving five states in the Pacific Northwest United States. Washington, Wyoming, Alaska, Montana and Idaho (WWAMI) together constitute over 25 percent of the land area of the United States, with 35 percent of this region’s population living in rural areas. The mission of the school includes “meeting the health care needs of our region, especially by recognizing the importance of primary care and providing service to underserved populations.”
In “Who Is Caring for the Underserved?” Grumbach et al. state:
Earning potential, lifestyle preferences, clinical infrastructure, and cultural barriers perpetuate physician maldistribution in the United States. History has shown the fallacy of expecting growth in physician supply to spontaneously ameliorate this maldistribution through a policy of passive diffusion of physicians to underserved communities…. Achieving a more equitable pattern of service to needy populations will require ongoing, active commitment by policy makers, educational institutions, and the professions to a mission of public service and to implementation of the incentives and support required to promote care to the underserved [1].
Fostering Student Interest in Underserved Care
Founded in 2006, the University of Washington School of Medicine Underserved Pathway (UP) provides curricular focus and support to students interested in the health and care of underserved populations. Between 2008 and 2009 the first 14 UP students graduated. Initially funded with Health Resources and Services Administration Title VII funds, Underserved Pathway faculty currently receive funding from the dean of the School of Medicine with staff support provided by the Department of Family Medicine.
The UP helps prepare future physicians to work with underserved populations by providing a foundation of practical knowledge and real-world experiences. As an elective, longitudinal, supplemental curriculum in the School of Medicine, the UP is open to all medical students. Students can complete the pathway or take advantage of the offerings without earning a certificate of completion [2].
UP goals are that students acquire a knowledge base about underserved communities and populations, have the opportunity to discuss issues affecting these communities with other students, and reflect on their role as future physicians. The hope is that students will ultimately practice in these areas. Longitudinal data regarding UP student residency choice and practice patterns is not yet available.
What is Meant by “Underserved”?
The UP defines “underserved” as individuals or populations who are disadvantaged because of inability to pay, lack of access to comprehensive health care, or other disparities for reasons of race, religion, language group, or social status.
Structure of the Underserved Pathway
UP staff and faculty assist each student to design a pathway tailored to his or her interests and career goals. Students may study broadly, focus on a specific populations or communities that interest them, or explore health policy and advocacy.
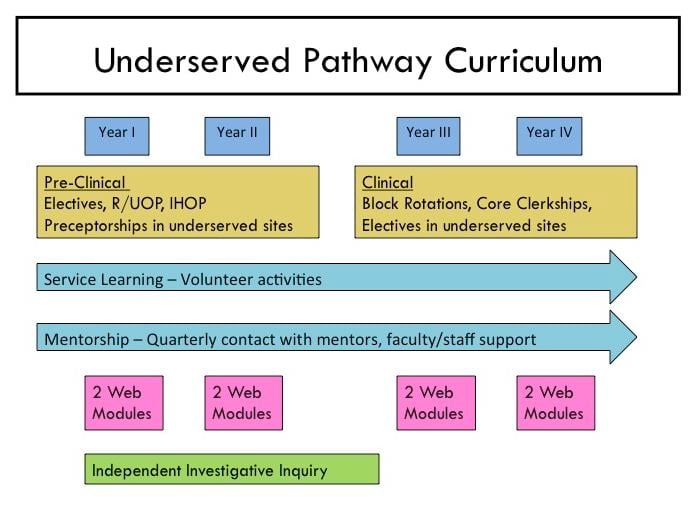
Several core elements characterize the UP (see fig. 1), providing pedagogic and practical grounding in the fundamentals of caring for the underserved.
- Service and Engagement: UP students complete 24 hours of service-learning activities through approved university or community-based programs. Activities include direct patient care, health education outreach, fundraising, and advocacy events.
- Mentorship: Mentors are typically practicing physicians who offer valuable insights into what it means to care for underserved populations. Students are in contact with their mentors quarterly. Most students develop a mentor relationship through experiences during their first year. Mentors are assigned to any second-year student who has not identified one.
- Required Coursework includes two main components:
Web-based curriculum. Web-based coursework serves the student population who rotate throughout the five-state region of the UW SOM. Students complete at least eight (of 13) UP modules. To complete a module, students either submit a brief reflective essay to which faculty advisors respond or take a quiz on the material covered. Faculty teach one module in person each quarter so students can meet and discuss the content of the module with their teacher and peers.
Current modules address government programs that provide coverage for underserved populations, care for individuals with disabilities, how race and ethnicity affect health and health care delivery, impact of chronic poverty, intimate partner violence, substance abuse, health care issues faced by people with HIV/AIDS, health literacy, concepts in public health epidemiology, and selected rural health topics.
Clinical and nonclinical courses. UP students select from existing courses that either have a related thematic focus or take place in a setting that cares for people who are vulnerable or underserved. This includes two credits of nonclinical electives from among more than 50 available courses. Advocacy and interdisciplinary care are modeled through many of the conjoint electives.
Students must complete 12 credits of clinical courses (including clerkships, subinternships, and advanced preceptorships) in underserved settings. The Rural/Underserved Opportunities Program (R/UOP) is an elective immersion experience in community medicine for students between years 1 and 2. During this 4-week rotation, students live in rural or urban underserved areas throughout the WWAMI region, providing care alongside practitioners in those communities.
- Scholarly Work. All UP students must complete a scholarly project known as the Independent Investigative Inquiry. They may satisfy this requirement through a hypothesis-driven inquiry, a critical review of a given literature, or an experience-driven community project through either R/UOP or an International Health Opportunities Program (IHOP) that promotes community health in a developing country. The project must address an issue that is relevant to the care of medically vulnerable populations.
Figure 1. Core elements of the Underserved Pathway.
Evaluation Methods
Completion of the UP is based on fulfillment of the required elements. Students do not receive grades or credit; they receive a certificate of completion, and recognition is included in the medical student performance evaluation (dean’s letter) upon successful completion of pathway requirements.
Program Improvement
The pathway conducts exit interviews with all graduating UP participants and with any student who leaves the pathway without completing it. These interviews gather feedback about student experiences and explore potential enhancements of the UP. All modules and coursework have built-in evaluation surveys which students are encouraged to complete.
Future Developments
Future activities of the Underserved Pathway include review of existing and development of new online modules, continued expansion of the mentorship network, and standardization of the program evaluation process. Since its inception, the UP has also worked close with the other School of Medicine pathways, including the Indian Health Pathway [3], the Global Health Pathway [4], and the Hispanic Health Pathway [5].
The Underserved Pathway is now a fundamental requirement of the curriculum for a new UW SOM program called TRUST. The Targeted Rural Underserved Track (TRUST) grants admission to a cohort of medical students through a secondary application and separate interview process. TRUST guides qualified, committed students through a special curriculum that connects underserved communities in Washington and Montana to the UW SOM and its network of affiliated residency programs to help meet the workforce needs of the region. As TRUST develops, it will expand to include Wyoming, Alaska, and Idaho [6].
References
- Grumbach K, Hart LG, Mertz E, Coffman J, Palazzo L. Who is caring for the underserved? A comparison of primary care physicians and nonphysician clinicians in California and Washington. Ann Fam Med. 2003;1(2):97-104.
-
University of Washington Department Family Medicine. The Underserved Pathway. http://depts.washington.edu/fammed/predoc/programs/upath. Accessed July 14, 2011.
-
University of Washington School of Medicine Native American Center of Excellence. Indian Health Pathway. http://faculty.washington.edu/dacosta/nacoe/ihp.html. Accessed July 14, 2011.
-
University of Washington School of Medicine & School of Public Health Department of Global Health. The Global Health Pathway (GHP). http://globalhealth.washington.edu/students_programs/cert_path.php. Accessed July 14, 2011.
-
University of Washington School of Medicine. Hispanic Health Pathway. http://faculty.washington.edu/dacosta/HHP/index.html. Accessed July 14, 2011.
-
University of Washington School of Medicine Department of Family Medicine. Targeted Rural/Underserved Track. http://depts.washington.edu/fammed/predoc/trust. Accessed July 14, 2011.



