The United States’ organ transplantation system suffers under the weight of its exclusive commitment to altruistic organ procurement. The prohibition against any procurement mechanism’s use of “valuable consideration,” including specialized exchanges, incentives, and payments, most likely contributes to thousands of unnecessary deaths each year. These deaths are the unfortunate byproducts of our federal legislative commitment to a purely altruistic organ procurement regime. Despite the low supply and extraordinarily high demand for organs, federal organ transplant law remains imbedded in its 1980s time capsule. This article documents several key weaknesses in the current U.S. transplant system. It concludes by advocating for greater flexibility in the organ procurement system, including proposing a federal carve-out to allow states to experiment with innovative programs.
Americans’ options for obtaining organs are constrained by federal law. The U.S. model emphasizes altruism over flexibility for historic rather than programmatic reasons. The “valuable consideration” prohibition, which anchors the National Organ Transplant Act (NOTA), imposes a prophylactic ban on the exchange of anything that might resemble emotional, monetary, or psychological value [1, 2].
History of the Current Organ Procurement Structure
U.S. transplant policy promotes altruism at all costs; commitment to this model alone cannot be justified on economic, social, or moral grounds. This inflexible procurement model grew out of an isolated instance of mild historic importance, where federal legislators rushed to create a law without the benefit of forethought and deep contemplation. The policy emerged as a federal response to the uninspiring plans of a lone rogue Virginia doctor, Barry Jacobs [3]. Jacobs had previously been investigated for fraud and as a result lost his license to practice medicine. In his new career, he proposed to broker organs [4].
In a 1983 Washington Post interview [5], Jacobs detailed his plan to recruit living organ sellers from developing countries. As a broker, he hoped to earn a few thousand dollars for each transaction. Many human rights activists did not take him seriously, but a few members of Congress galvanized an internal campaign to prohibit any such business plan from taking effect [5]. The result of their efforts is NOTA, passed in 1984 [4], specifically in response to a censured, unlicensed doctor who lacked credibility.
Prior to this time, organ transplantation policy was determined at the local level by states [7]. In 1968, all 50 states adopted the Uniform Anatomical Gift Act (UAGA) [8], signifying that legislators basically agreed on transplant policy. Noticeably, their policies were neutral on the question of incentives, leaving such matters to be addressed on a case-by-case basis at the state level. Indeed, after presenting the model law to their home states for ratification and enactment, legislators sought to work within the spirit of the original draft. Thus, in a radical shift, states that had previously enacted laws to ban payments for organs and body parts—among them Massachusetts, Delaware, Hawaii, Maryland, and New York—repealedthose regulations [9]. In so doing, they, too, were expressly leaving open the question of incentives, payments, and other forms of valuable consideration, at least for the posthumous disposition of organs and human tissues.
NOTA’s Consequences
Despite what might have been the best intentions at the federal level, such as prohibiting black markets or the exploitation of men and women from third-world countries, their rush to legislate has backfired. Noticeably, 30 years later, the government’s altruistically-focused policy contributes to the very exploitation of people of color in developing countries it sought to prevent. The U.S. demand for organs spills over into other nations, where individuals’ poverty and vulnerability make them the voiceless conspirators in a very dangerous enterprise. Ironically, federal efforts to avoid domestic organ sales now contribute to the international human trafficking in organs. Quite possibly, more organs are trafficked now than had Dr. Jacobs been the most successful businessman on earth [10].
As with any business, Jacobs’ enterprise would have been subject to some regulation, and vulnerable to civil liability and criminal penalties for any illegal activities conducted in association with his business. Individuals could have sued Jacobs had he violated contracts, harmed their dignity, or otherwise coerced them. Had he been negligent in the treatment of potential “donors” or recipients, civil law would have been a logical recourse—as well as criminal law. Such forms of private regulation are intended to protect vulnerable individuals from harm by individuals as well as organizations.
There are few domestic disincentives to monitor or police Americans trafficking organs from abroad. Because demand outpaces organ supply, Americans actively participate in black- and grey-market transactions in Asia, Africa, and South America [10]. Frequently, Americans obtain organs from executed political prisoners in China, as well as from destitute men and women in India, Pakistan, South Africa, and Brazil [10]. American patients pay brokers upwards of $150,000 for kidneys and as much as $250,000 for hearts [11]. Rather than waiting more than 6 years for a kidney, patients can obtain this vital organ on the black market in less than 8 weeks [12]. These black-market exchanges are the byproducts or outgrowths of an altruistic system that lacks the capacity to adequately meet organ demand. Thus, our “altruistic” procurement regime contributes to an aggressive, overt system of unregulated, unmonitored, organ markets that undermines the health and dignity of individuals abroad as well as patients in the United States.
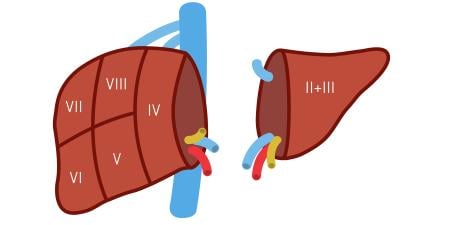
Unsurprisingly, NOTA’s inflexibility prohibits more than financial payments to donors. Years ago, this policy prohibited organ exchanges, such as daisy and domino chains, from forming because “love” was considered a “valuable consideration” [3]. The irrationality of that type of rule-making is more than obvious. In that context, noble programs like the National Kidney Registry—a not-for-profit organization founded by Garet Hil, whose sophisticated computer programming matches people willing to swap organs for their friends and loved ones [13, 14]—could not exist. In February 2012, the New York Times reported on Hil’s most recent pairing of more than 60 individuals. With a private, innovative effort, Hil has advanced transplant procurement more than any federal government efforts. However, his program could launch only after Congress revised NOTA’s prohibitions to exclude daisy chains [3].
Other programs suffered, failed, or could not launch because of NOTA’s strict proscriptions. U.S. organ procurement policy discouraged the Pennsylvania legislature from pursuing a burial benefit program [15], an effort designed to ease the costs of funeral and hospital expenses for families that chose to donate their deceased relative’s organs. The Pennsylvania legislature invested in the effort for nearly a decade prior to conceding that federal law could lead to the incarceration of potential participants, including administrators at hospitals who accepted a payment for medical bills or the relatives that donated organs.
Indeed, the valuable-consideration clause in NOTA operates even at the most innocuous or frivolous level, meaning that receiving a cup of coffee, slice of bread, or movie ticket in exchange for donating a kidney violates the law [16]. Criminal penalties attach to any violation of the law—and the consequences are quite severe: a $50,000 fine and incarceration up to five years [17].
The Altruistic System Operates At Maximum Capacity
Many are harmed by the valuable consideration rule, but who benefits? Arguably, no one; the proscription is overinclusive in prohibiting well-meaning programs that involve no financial exchanges and chilling innovation, and it is underinclusive in tolerating markets for babies, ova, sperm, embryos, and commercialized cell lines and human tissues. Successful organ recipients sometimes register at multiple locations to increase their odds of receiving an organ. Such tenacity takes more than will, but also the type of financial resources often out of reach for poorer Americans. In addition, the waiting time on the lists is so lengthy that health deterioration and becoming too sick for a transplant are associated risks of the U.S. transplant model. These issues dominate the “real-life” concerns of patients and their families.
Much has changed since NOTA’s enactment in 1984. Beyond a doubt, some of this has been positive, including improvements in surgical technology, the enhancement of immunosuppressive medications, and more sophisticated data-collection and sharing mechanisms. These technological advancements (along with a host of others) enhance the transplant process and ultimately save lives.
However, negative externalities dominate many key aspects of contemporary transplant policy. In the 28 years since NOTA’s passage, the demand for organs has not kept pace with supply. In the U.S., thousands die each year waiting for organs. About 7,000 patients die each year after interminable waits on transplant lists [18]. They are not the only patients who suffer under the unbearable weight of an enormously constrained transplant system.
Currently, more than 113,000 Americans wait for organs, but it is likely fewer than 13,000 people in the United States will agree to become organ donors this year [19]. This gap between supply and demand manifests most perniciously in the kidney-transplant waitlist; more than 90,000 patients wait for kidneys [20]. Even that figure misrepresents the true number of people who could benefit from receiving a healthy kidney: nearly 500,000 Americans receive dialysis treatments [2], and many will never be counseled about the option to receive a kidney.
Therefore, the number of deaths on the waitlist provides an incomplete account of the devastating implications of our current transplant policy. Peeling back the veneer of altruism reveals other troubling aspects of the current altruistic organ procurement regime. For example, many other patients who never had access to transplant waitlists die each year; these unfortunate men and women were tethered to dialysis machines several days per week for hours at a time. Some patients describe that process as a death sentence or akin to being medically imprisoned [13].
Burning, bloating, infections, low blood pressure, fatigue, and nausea commonly result from dialysis treatments. Presently, about 500,000 Americans endure this reality [2]. Patients bravely endure these side effects not because dialysis cures the underlying disease—the treatment does not—but because this weekly, if not daily, process keeps them alive. Of these patients, most never made the kidney transplant waitlist because they were too sick, too old, too poor, too uneducated, or simply unable to convince doctors that they were “suitable” for an organ transplant. Some dialysis patients receive organs, but that group represents a tiny fraction of the overall population on dialysis. In reality, rationing is a necessary effect of the U.S. organ transplant policy; too few organs in the supply chain inevitably leads to pernicious forms of rationing and lengthy waitlist queues.
The U.S. kidney transplantation regime particularly disserves African Americans. Blacks wait longer than any other group for kidneys [21], they suffer the highest death rate while on the transplant list [21], and they are more frequently kicked off the list than any other ethnic population [22]. Government explanations for these discrepancies and disparities are inadequate [22]. Bureaucrats frequently point to low donation rates among African Americans as the chief reason why they fare so poorly on the back end [22]. In other words, if more organs from African Americans came into the system, then more organs would come out—or at least it would improve the odds of better HLA “matching” for African Americans. The argument is not illogical on its face. However, it must be understood that the federal transplant system provides only one, poorly planned route into organ donation—altruism; all others are blocked. This affects everyone, not only African Americans.
Federal Funding Bears Little Relationship To Promoting Organ Transplants and Raises Costs
The federal government provides unlimited spending for only one treatment of kidney disease: dialysis [23]. Dialysis does not cure end-stage renal disease or other diseases associated with kidney failure. Federal funds are not allocated toward underwriting daisy chains, despite immediate cost savings. Neither does the federal government offer states financial incentives to create innovative organ-sharing programs. In short, the government has committed its funding primarily toward an important but less-than-ideal solution.
Thus, Americans pay for our antiquated organ procurement policies in key ways. First, Americans pay with their lives; many waitlist candidates and dialysis patients die each year from otherwise treatable diseases. Second, family members suffer the collateral effects of the lengthy waitlist process and the need for caregivers for dialysis patients—some family members stop working to care for their relatives, while others work more to compensate for income loss due to their partners’ disability. Third, the financial costs associated with treating kidney disease take up about 6-7 percent of the Medicare budget [24]. In other words, taxpayers fund dialysis treatments. For each dialysis patient, federal expenditures can range from $60,000-$90,000 per year [25]. The Government Accountability Office (GAO) estimates that federal spending for kidney disease costs taxpayers more than $30 billion per year [26]. Each patient removed from dialysis and given a transplant saves taxpayers $500,000 to $1 million per year [27].
On inspection, serious problems emerge with an “altruism at all costs” organ-procurement model, including the senseless loss of life. At a cost of $30 billion per year, federal expenditures should bear some relationship to the number of lives saved, not simply those put on dialysis.
Moving Forward
The question of how to enhance a system beyond its capacity into one that self-sustains and thrives has defied law makers for nearly 3 decades. Their decision making is beset with challenges, not only from patient-consumers demanding life-sustaining treatments but also from the desire to balance competing political, ethical, medical and social interests.
Exclusive reliance on the present altruistic organ procurement process in the U.S., in light of alternatives, undermines the very purpose of volunteerism and noncoercion by fueling living-donor markets in developing countries. Other options, including directed donations, nonfinancial incentives, financial incentives, job-protection programs, and presumed consent, deserve meaningful consideration. Each of these measures involves risks and must be judged according to what benefits it would bring in light of the burdens experienced or values compromised.
To move forward, states must be released from the shackles put in place by NOTA. The veneer of altruism does not cover preexisting commercial relationships in human biological material, including corporate sales of human tissue, tendons, bones, and heart valves at enormous profit. The human-tissue industry grosses billions of dollars each year with mild regulation from the Food and Drug Administration [28, 29]. Commercial bio-banks buy, sell, trade, and research human biologics unfettered by NOTA’s proscription [30].
On the other hand, the reproduction market successfully commercializes human biologics while maintaining and valuing human dignity. Built into that system are sets of local standards that minimize coercion and exploitation, while promoting healthy biological exchanges. Courts are appropriately utilized to settle disputes when they occur. Ironically, this industry bypasses federal regulation and oversight even when some modest standards might be advisable to reduce dependence on courts to settle disputes. Unburdened by federal intervention, men and women exchange ova, sperm and embryos and rent wombs to create families. When considered, the inflexible federal policy that proscribes all valuable consideration in the organ realm cannot be justified in light of the government’s tolerance of other nonregulated human biological exchanges, most of which do not save lives.
How should the U.S. move forward? The first significant step in relieving organ scarcity involves allowing states to engage in monitored, approved experimentation. These efforts can take place if the federal government permits states to waive out of NOTA. The waiver process is not new; states waive out of federal regulation through an administrative process. Most recently, President Barack Obama announced plans to allow states to waive out of the education regulation No Child Left Behind [31]. Waivers are not provided in lieu of state action on a given issue. Rather, waivers allow states to attempt to achieve federal goals through novel, innovative, untested programs. As a general matter, states with waivers propose meeting federal goals at reduced costs and with maximized participation.
Solutions for the organ shortage in the U.S. are well within reach. With leadership at the highest levels of government, the U.S. can relieve organ demand. As Congress approaches the thirtieth anniversary of the passage of NOTA, it would be wise to revisit the law in light of social acceptance of innovation in the human biologic realm. The introduction of a waiver allowance would permit states like Pennsylvania to introduce dynamic, lifesaving programs. A second step should be the allocation of federal dollars to support programs that increase the number of transplants performed each year and remove patients from dialysis, like the National Kidney Registry. Other efforts should include financially supporting states that launch innovative organ-sharing programs. A final step should involve the repeal of NOTA’s valuable-consideration clause, which has outlasted its purpose and no longer protects vulnerable individuals from the reach of desperate Americans who need kidneys. A better tailored response is needed to reduce human trafficking and save lives.
References
-
Satel S. When Altruism Isn’t Enough: The Case For Compensating Organ Donors. Washington, DC: American Enterprise Institute Press; 2009.
-
Kissling F. Whaddya have to do to get a kidney around here? Salon. March 27, 2009. http://www.salon.com/2009/03/27/my_kidney/. Accessed February 23, 2012.
-
Goodwin M. Confronting the limits of altruism: a response to Jake Linford. St Louis Univ J Health Law Policy. 2004;2(2):328.
-
Goodwin, Confronting the limits of altruism, 327.
-
Goodman E. Life for sale. Washington Post. October 1, 1983: A15.
-
Goodwin, Confronting the limits of altruism, 327 note 2.
-
University of Michigan law faculty. Memorial resolution by the University of Michigan law faculty concerning E. Blythe Stason. Michigan Law Rev. 1973;71(3):451-458.
-
Stason EB. The Uniform Anatomical Gift Act. Business Law. 1968;23:927.
-
Statutes cited in: Denise SH. Note, regulating the sale of human organs. Virginia Law Rev. 1985;71(6):1022-1023.
-
Goodwin M. Black Markets: The Supply and Demand of Body Parts. New York: Cambridge University Press; 2006: 11.
-
Interlandi J. Not just urban legend. Daily Beast. January 9, 2009. http://www.thedailybeast.com/newsweek/2009/01/09/not-just-urban-legend.html. Accessed February 23, 2012.
-
Goodwin, Black Markets, 10-11.
-
Sack K. 60 lives, 30 kidneys, all linked. New York Times. February 18, 2012. http://www.nytimes.com/2012/02/19/health/lives-forever-linked-through-kidney-transplant-chain-124.html. Accessed February 23, 2012.
-
National Kidney Registry. Our story. http://www.kidneyregistry.org/about_us.php#our_story. Accessed February 22, 2012.
-
Goodwin M. Transplant rules are out of touch with reality. Chronicle of Higher Education. January 22, 2012. http://chronicle.com/blogs/brainstorm/national-organ-transplant-rules-are-out-of-touch-with-reality/43306. Accessed February 23, 2012.
-
Goodwin M. Altruism’s limits: law, capacity, and organ commodification. Rutgers Law Rev. 2004;56(2):397.
-
Prohibition of organ purchases, 42 USC section 274(e) (2007).
-
Goodwin, Altruism’s Limits, 311.
-
United Network for Organ Sharing. Transplant trends. http://www.unos.org/. Accessed February 22, 2012.
-
Organ Procurement and Transplant Network. http://optn.transplant.hrsa.gov/latestData/viewDataReports.asp. View data reports. Accessed February 22, 2012.
-
Organ Procurement and Transplantation Network, Scientific Registry of Transplant Recipients. 2004 OPTN/SRTR Annual Report. http://www.srtr.org/annual_reports/2010/ar_archives.htm. Accessed February 22, 2012.
-
Goodwin, Altruism’s Limits, 353.
-
US Government Accountability Office. End-stage renal disease: CMS should monitor effect of bundled payment on home dialysis utilization rates; 2009. http://www.gao.gov/htext/d09537.html. Accessed February 23, 2012.
-
Rubenstein C. Dialysis, where Medicaid steps in. New York Times. January 25, 2004. http://www.nytimes.com/2004/01/25/nyregion/dialysis-where-medicaid-steps-in.html?pagewanted=all&src=pm/. Accessed February 23, 2012.
-
Highbeam Business. Industry reports: idney dialysis centers: SIC 8092. http://business.highbeam.com/industry-reports/business/kidney-dialysis-centers. Accessed February 23, 2012.
-
United States Renal Data System. Chapter 11: costs of ESRD. 2011 USRDS Annual Data Report; vol. 2. US Renal Data System; 2011: 282. http://www.usrds.org/2011/pdf/v2_ch011_11.pdf. Accessed February 23, 2012.
-
United States Renal Data System, 284.
-
Celebrating a history of cell culture (1907-2007). Corning Inc. http://www.corning.com/lifesciences/us_canada/en/about_us/cell_culture_history.aspx. Accessed February 22, 2012.
-
Lee T. From human tissue supplier to R&D contractor to biobank builder, Asterand seeks its future. Chrysalis. March 16, 2011.
-
See e.g., Health controls wanted on sale of human tissue. BBC. June 19, 1998. http://news.bbc.co.uk/2/hi/health/116047.stm. Accessed February 23, 2012.
-
Hu W. 10 states are given waivers from education law. New York Times. February 9, 2012, http://www.nytimes.com/2012/02/10/education/10-states-given-waivers-from-no-child-left-behind-law.html. Accessed February 23, 2012.