The health care system may move toward applying value-based purchasing more broadly. If this occurs, those making value-based decisions will need measures of efficiency to provide guidance. Measuring efficiency, whether in health care or elsewhere, involves a comparison of inputs into a process with the outputs of that process. A wide variety of metrics has been used in the academic literature to assess the efficiency of medical care, including but not limited to return on investment, cost-benefit, and cost-effectiveness. In each type of evaluation, analysts make a structured comparison of inputs into the process of providing medical care and improving health (with the resources used often valued in dollars) with the health, productivity, or quality-of-life outcomes of that care.
One difficulty with trying to design a useful measure of efficiency is that there are numerous stakeholders—patients, families, insurers, employers, the government, and the health care providers. Each of these stakeholders may have a different perception of how much it is justifiable or worthwhile to spend on a visit or episode of care. For example, insurers, who pay a large portion of the cost for many services, may be more motivated to reduce costs than patients. Additionally, each stakeholder may prioritize the outcomes of care differently, e.g., the employer may view making the patient more productive as more important than saving medical care costs at present or in the future. In short, considerations of which outcomes are important or which expenses worthwhile are likely to lead to value-laden disputes.
In 2012, the National Quality Forum (NQF) promulgated a set of measures of efficiency [1] that take a different approach than cost-effectiveness measures that might be reported in the academic literature as dollars spent per quality-adjusted life-year gained. From available descriptions [2, 3], it appears the NQF measures are designed to (1) include data on the quantities of various resources used, (2) risk-adjust the resource use for the severity of the condition, (3) apply a standard price so that providers in more expensive areas who use the same resources as providers in less expensive areas would not be considered inefficient simply because their inputs’ prices are higher, and (4) compare the quality of outcomes with the resources used.
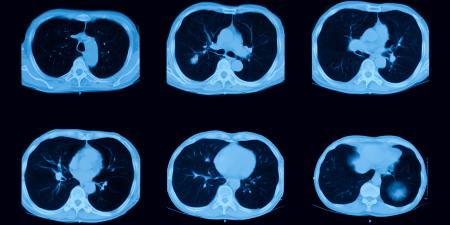
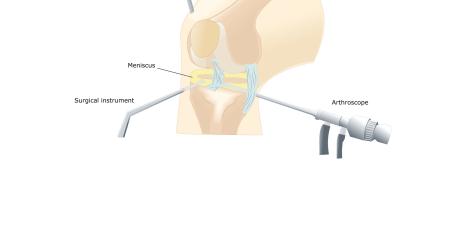
The focus on resource use means that the measurement begins by counting numbers of visits, hospitalizations, and laboratory tests or imaging studies. A visit that involves only evaluation and management with no imaging and no labs is counted differently than a visit that entails labs and other procedures. This is the first step in making sure that the comparison is as logical and as meaningful as possible, focusing on whether there is waste rather than other variations in the price of resources for care.
The process of risk adjustment is necessary because variation in disease severity is associated with appropriate variation in resource utilization. Physicians who treat patients who are more severely ill should not be penalized for this. The process of risk adjustment modifies the quantities of resources to make the comparison fairer.
The application of standard prices is another step in the effort to assure that the comparisons being made are fair and meaningful. Consider the fact that even Medicare has different reimbursement rates in different regions. One simple approach would be to use Medicare national average reimbursement levels. Other reimbursement systems could be employed as well, although many are similar to Medicare. Without a standardized value applied to each resource being measured, different practices could not be compared.
Finally, the combination of quality and resource-use measures allows for the assessment of efficiency. This is the final step in the process of making certain that the use of resources for generating similar outputs is being compared. The objective appears to be to compare the costs of providing the same level of quality. This is a simpler, less value-laden question than comparing the costs of a given treatment with its effects and asking whether it is worth spending a certain amount more to achieve greater health. Instead, when resource-use and quality measures are juxtaposed, the resources used to provide the same level of quality can be compared. The question of what level of quality is appropriate is then separate.
Sometimes when the desire to drive the health care system toward greater efficiency is discussed, there is a concern that the focus is exclusively on costs and that providers (both physicians and hospitals) will have an incentive simply to minimize costs at the expense of outcomes. This is unlikely to be the case when the cost metrics are used in conjunction with quality metrics. It is likely that some costs can be cut by providing care more efficiently, with little impact on outcomes. Cutting costs by reducing the use of needed resources will eventually lead to worse health outcomes. If the quality, as measured by health outcomes, is diminished, the contracting and reimbursement system between insurers and providers will likely penalize the provider—either with reduced levels of reimbursement or with fewer contracts going forward.
Ideas about what levels of quality are acceptable and what is worth paying for can vary among stakeholders. Each stakeholder will have to determine how to incorporate quality into the decision making process. The aspect of the NQF measures that makes them widely useful is the focus on comparing like with like: risk adjusting, standardizing input prices, and comparing only clinicians whose services result in the same outcome ensure that it is not making value judgments.
References
-
O’Reilly K. National Quality Forum adopts cost metrics for value-based purchasing.American Medical News. April 23, 2012. http://www.ama-assn.org/amednews/2012/04/23/prsb0423.htm. Accessed August 31, 2012.
-
NQF endorses additional resource use measures [news release]. Washington, DC: National Quality Forum; January 31, 2012. http://www.qualityforum.org/News_And_Resources/Press_Releases/2012/NQF_Endorses_Resource_Use_Measures.aspx. Accessed October 10, 2012.
-
National Quality Forum. Endorsement summary: resource use measures. http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=69883. Accessed October 10, 2012.