The degree to which “conscience” should guide physician practice has been frequently debated in recent years within medicine, bioethics, and health policy circles [1-3] and has found new life in the debate about various “conscience protection” rules issued by the G. W. Bush and Obama presidential administrations. In these debates, physician “conscience” has been invoked in the medical literature almost exclusively in cases in which physicians attempt to avoid or to decline participation in practices or procedures that they find morally objectionable, often because such practices violate the physician’s religious or cultural practices. In this debate, “conscience” is therefore often associated with religious belief or, at least, with deeply held “values” of the physician in question [4, 5].
Medical educators and physicians, however, do not typically invoke the language of “values” or “conscience” in the context of ordinary medical practice: decisions, for example, about whether to prescribe a benzodiazepine for an anxious patient or an antibiotic for an upper respiratory tract infection are framed as a matter of “clinical judgment” but rarely as a matter of “values” or “conscience.” As a result, it is easy to assume that everyday medical practice does not require either, unless problems or disagreement arise. Conscience, that is, is conceived not as constitutive of and routine within the practice of medicine, but rather as some sort of external referee that interjects itself when clinicians believe particular practices to be morally objectionable.
This bracketed and externalized conception of physician “conscience” reflects more generally the pervasiveness of the fact-value (and science-ethics) divide within modern medicine: ordinary medical practice is an applied science (dealing with “facts”); “values” are, in contrast, the province of ethics, and need to be interjected from the outside, either from the patient (in the form of “autonomy”) or from the physician (often in the form of “paternalism”). Modern medical ethics has grappled at length with whosevalues ought to guide medical practice, but has only rarely challenged the fact-value distinction within which such debates (e.g., between “autonomy” and “paternalism”) are enshrined [6-8]. The recent debates over physician conscientious objection have largely echoed these broader bioethical debates, with similarly inconclusive results.
What would be the implications for medical ethics, however, if “conscience” were not some sort of external moral faculty that trafficked in “values” (rather than “facts”) but, rather, were a quite ordinary part of human decision making, inseparable from the living of everyday life and from the routine, day-to-day practice of medicine? Such a conception of conscience would render it more mundane and unremarkable but would, on the other hand, raise awareness of its quiet but important presence within the daily lives of physicians and medical practitioners. As it turns out, this more integrated conception of conscience was common in premodern moral philosophy. In this brief essay, I will outline the account of conscience given by the premodern philosopher and theologian Thomas Aquinas (~1225-1274), whose work was important in extending the thought of Aristotle into the medieval era, and will briefly suggest how Aquinas’ thirteenth-century conception of conscience might apply to modern bioethics and to the modern education of physicians.
In his work on moral philosophy, Aquinas presents a complex and detailed account of human action which, though dated in some ways by Aristotelian assumptions about biology, is still relevant today. Human knowing, Aquinas stated, can be directed in two ways: speculatively, with regard to what is true (for example, the law of noncontradiction), and practically, with regard to what is good, or what should be done. What is true and what is good are, of course, closely linked to one another, and in fact Aquinas believed that humans are equipped with a disposition (called synderesis) to know certain self-evident abstract practical truths, such as that “the good is to be done, and evil avoided.” [9].
But abstractions like that can only go so far: the biggest challenge in acting well is not formulating abstract moral principles but, rather, applying those principles to concrete situations in the complex context of everyday life. And this relating of abstract principles to real-life situations, the figuring out of what “the good” is in any particular setting, is what Aquinas refers to as conscience (conscientia), the application of knowledge to a particular case [10]. Conscience, then, is for Aquinas not even a power or a faculty at all—it is simply the act by which the action-guiding practical intellect identifies the good (i.e., that which should be pursued) in a particular situation. Applied to medicine, instances of “conscientious objection” (for example, refusing to participate in torture) would certainly involve acts of conscience—but so would instances of prescribing an antibiotic for pneumonia, or counseling a teenager to quit smoking, or operating on an acute abdomen. Conscience in this view turns out to be nothing more, and nothing less, than clinical judgment—identifying what course of action is appropriate in a specific patient case.
Just as modern medical educators know that clinical judgment is neither innate nor infallible, but must be formed and refined over months and years in the context of supervised medical training, so also Aquinas knew that conscience was not infallible either. The ability to exercise conscience appropriately—to consistently recognize courses of action that are good or fitting in particular situations—is in fact a hard-won achievement which Aquinas describes as the virtue of prudence (prudentia). Prudence in Aquinas’ sense, in contrast to a common modern use of the term, does not connote timidity or excessive caution. The prudent physician, in Aquinas’s sense, is not one who is painstakingly risk-avoidant or conservative in decision-making but, rather, one who consistently knows what to do in complex clinical situations: the prudent physician shows consistent “presence of mind” [11].
But this clinical presence of mind (prudence), which names the consistent presence of good clinical judgment (conscience) in the practice of a physician, is not easily achieved. It requires a person to cultivate virtues like courage, self-control, and justice that help orient him or her to things that are truly good, rather than things that only seem so [12]. It requires years of iterative practice and openness to correction by more experienced teachers [13]. And it requires that medical decision making not be reduced to algorithm.
Extending Aquinas’s thinking equating conscience with clinical judgment and vice-versa would have several important implications for medical education and for modern debates about “conscientious objection” within medicine.
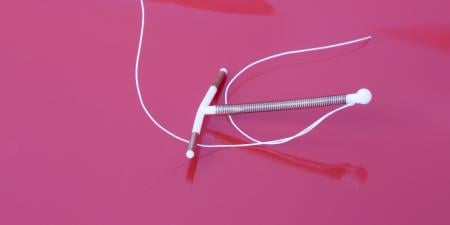
First, “conscience” would no longer be understood as a separate decision-making faculty that comes into play only with regard to morally or socially controversial situations: it simply is clinical judgment. The physician who declines to prescribe oral contraceptives because, for religious reasons, he or she judges that the patient would be harmed by these medications, is exercising clinical judgment, and, conversely, the physician who prescribes a statin for hypercholesterolemia is exercising conscience. Such a reconceptualization does not, of course, resolve the issue of whether the first physician ought to be allowed to decline oral contraceptive prescription, or whether the physician is correct in his or her judgment, but it at least makes clear that physicians who are required to act contrary to conscience are eo ipso being required to act contrary to their clinical judgment—a very serious matter for physician professional identity.
Second, equating conscience with clinical judgment would challenge the way that ethics is marginalized (and marginalizes itself) within contemporary medical educational institutions and their teaching curricula. “Ethics” is not a specialized and esoteric discipline to be invoked only in moments of crisis or “dilemma”; it is, rather, simply an account of what good medical practice looks like in particular situations, even when these situations are pedestrian and uncontroversial. Daily bedside teaching rounds are pervasively about “ethics” even when that word is never mentioned.
Third, equating clinical judgment with conscience makes clear that medical education is at root a process of moral formation, in which promising but naive clinicians who lack the ability to discern the good in particular clinical situations (that is, whose acts of conscience are unreliable) are formed, through hard study and iterative practice under the guidance of competent teachers, to become clinicians capable of consistently knowing and doing the good. Medical education, in other words, is essentially a training of conscience. The consistent and reliable display of rightly-formed conscience over the course a medical career, furthermore, is prudence—arguably the most important characteristic that any physician can ever display.
References
- Wicclair MR. Conscientious objection in medicine. Bioethics. 2000;14(3):205-227.
- Pellegrino ED. The physician’s conscience, conscience clauses, and religious belief: a Catholic perspective. Fordham Urban Law J. 2002;30(1):221-244.
- Lawrence LE, Curlin FA. Clash of definitions: controversies about conscience in medicine. Am J Bioethics. 2007;7(12):10-14.
- Savulescu J. Conscientious objection in medicine. BMJ. 2006;332(7536):294-297.
- Savulescu J. The proper place of values in the delivery of medicine. Am J Bioethics. 2007;7(12):21-22.
- Kaldjian LC. Teaching practical wisdom in medicine through clinical judgment, goals of care, and ethical reasoning. J Med Ethics. 2010;36(9):558-562.
-
Fulford KW, Broome M, Stanghellini G, Thornton T. Looking with both eyes open: fact and value in psychiatric diagnosis? World Psychiatry.2005;4(2):78-86.
- Khushf G. Why bioethics needs the philosophy of medicine: some implications of reflection on concepts of health and disease. Theor Med. 1997;18(1-2):145-163.
-
Thomas Aquinas. Summa theologiae. Ia.79.12.
-
Thomas Aquinas. Summa theologiae. Ia.79.13.
-
Pieper J. The Four Cardinal Virtues. Notre Dame, IN: University of Notre Dame Press; 1966.
-
Thomas Aquinas. Summa theologiae. Ia-IIae. 57.4.
-
Thomas Aquinas. Summa theologiae. Ia-IIae. 52.3; IIaIIae.47.15.