In the last 50 years, a surge of reproductive technology has revolutionized the practice of obstetrics and gynecology. First, effective hormonal contraceptives were made available to the public in the 1960s and, since their debut, have been used to treat almost every gynecologic abnormality [1]. Second, in the past 30 years, infertility has largely been managed using assisted reproductive technologies (ART), primarily intrauterine insemination (IUI) with recourse to in vitro fertilization (IVF) when insemination fails [2]. As a result, the modus operandi in mainstream gynecology has been to suppress, or to bypass, the woman’s fertility cycle.
Physicians and patients who (1) conscientiously object to the therapeutic use of hormonal contraceptives on the grounds that it subjects patients to ineffective treatment of symptoms rather than treating their underlying disease and (2) morally oppose the ART approach to infertility on the grounds that it jettisons a loving act of marital intercourse, the one context worthy of the conception of a new human being, are now able to pursue an alternative approach that accords with their consciences. NaProTECHNOLOGY (an acronym for natural procreative technology) is a woman’s health science that encompasses a unique medical and surgical application of gynecology. The foundation of NPT is the Creighton Model FertilityCare System (CrMS), see Figure 1, the only prospective and standardized means of monitoring the various patterns of a woman’s menstrual and fertility cycle for the natural regulation of fertility.
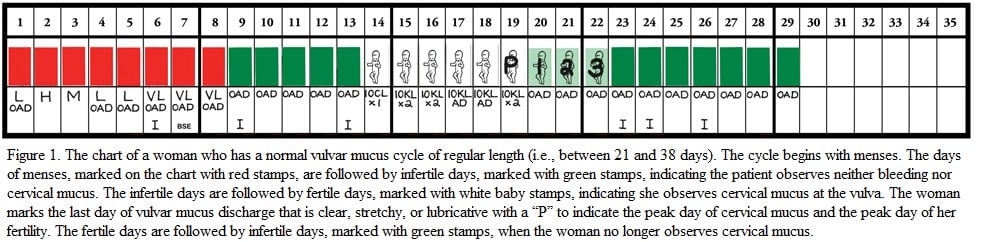
For example, because it views infertility as a symptom rather than a disease, NPT seeks to diagnose and treat the underlying causes of infertility so that the couple can more successfully conceive within their own acts of intercourse, especially during peak-day-focused intercourse. NPT infertility protocols depend on patient-specific charting data. Some observations during the fertility cycle—dry, limited, or continuous mucus; short or variable post-peak phase; premenstrual spotting or tail-end brown bleeding—are external signs of possible underlying disease processes.
A medical interpretation of these abnormal CrMS observations leads to a targeted biochemical and hormonal evaluation, which in turn identifies target organ dysfunctions: decreased production of estrogenic cervical mucus, intermenstrual bleeding or spotting, short or variable luteal phases, and suboptimal levels of the ovarian hormones (estrogen or progesterone). Common treatments for these pathologies include induction or stimulation of ovulation, medications to enhance cervical mucus, and hormonal support in the luteal phase. When these NPT medical approaches to infertility were used in a study of 1,239 infertile couples, they resulted in a live birth rate similar to that of cohort ART treatments [3].
In many cases, medical applications of NPT are sufficient to treat infertility successfully; in other cases, surgical intervention is also required. Surgical NPT is a specialized form of gynecologic surgery the primary aim of which is to reconstruct the uterus, fallopian tubes, and ovaries. The ovarian wedge resection (surgical removal of a portion of an enlarged ovary to restore its normal size), for example, is effective in healing polycystic ovaries (contributing to the long-term treatment of some of the endocrine and menstrual cycle abnormalities associated with polycystic ovaries). It also brings the patient a 70 percent chance of pregnancy i.e., it is twice as effective as clomiphene [4].
A significant benefit of surgical NaProTECHNOLOGY is “near adhesion-free” surgery. One of the biggest pitfalls of surgery, of course, is the formation of postoperative adhesions, which can decrease tubal motility (adversely affecting fertility) and cause small bowel obstructions (that frequently require emergency reoperation) [5]. To prevent these complications, NPT surgical techniques pay meticulous attention to detail, take a systematic approach, and use Gore-Tex adhesion barriers [6]. Published Gore-Tex protocols reveal a statistically significant decrease in subsequent adhesion scores on second-look laparoscopy [7]. For some reason, the use of Gore-Tex has been overlooked in even the most recent adhesion prevention reviews [8]. One even laments that adhesion prevention is a “surprisingly neglected aspect of the treatment of endometriosis,” but the reviewers make no mention of the use of Gore-Tex as an adhesion barrier.
Other techniques of surgical NPT include laser vaporization and pelvic excision and repair surgery (PEARS) of peritoneal or ovarian endometriosis. PEARS is a form of plastic reconstructive surgery of the pelvis with the primary intent of removing diseased tissue within the pelvic organs and repairing organs in a way that does not form pelvic adhesions. PEARS can entail robot-assisted laparoscopy or laparotomy, minimizing postoperative adhesions and optimizing the patient’s chances for pregnancy.
The effectiveness of treating infertility with medical and surgical NPT is comparable to that of ART interventions. The cumulative live birth rate in patients receiving IVF is between 45-55% [10]. In a study population of 1,045 patients treated with NPT infertility protocols, more than 60 percent became pregnant within 24 months and nearly 70 percent within 36 months [11]. The overall �per-woman� NPT pregnancy rate is higher than that of ART due, in part, to the high rate of dropout or discontinuation in patients who undergo IVF treatment [12]. In addition, a meta-analysis comparing conventional surgery and IVF for treatment of endometriosis-related infertility found that the per-woman pregnancy rates with surgery were 55.3 percent while those with IVF were 9.9 percent [13]. However, while it is true patients treated with NPT have significantly lower overall fecundability (a 3.13 percent chance of conceiving within a given period) than those treated with IVF (13.3 percent), it is also true that the number of women who ultimately achieve a pregnancy with NPT is higher than the number who get pregnant using ART [14]. Thus, although achieving a live birth with NPT may take longer, it has a greater chance of occurring than with IVF.
For those interested in training in NPT, the Pope Paul VI Institute and Creighton University School of Medicine offer educational programs for those in primary care or ob/gyn (including fourth-year medical students) to train in the medical applications of NaProTECHNOLOGY [15]. They also offer a 1-year fellowship in the surgical applications of NPT for ob/gyns who have completed their residencies [16].
The Ethos Grounding NaProTECHNOLOGY
The previous thumbnail sketch of some of NPT’s protocols demonstrates NaProTECHNOLOGY’s distinctive medical and surgical infertility applications. But they are just one of its hallmarks. The ethical grounding of NPT’s infertility praxis is also distinctive.
NPT’s moral evaluation of fertility interventions is grounded in the following principles and values articulated by the Roman Catholic tradition, rooted in the nature of medicine, Aristotelian/Thomistic philosophical anthropology, and a personalist procreative ethics [17-27].
In this view, the human person is a body-soul unity. The human body is not regarded as some sort of subpersonal or “lower” bodily nature, detached from the higher spiritual powers of reason and will; we are not persons who have or use our bodies. We are our bodies. The human body is considered one of the realities of personhood, and the human person a bodily one. This view understands human persons, then, as unitary, but composite, beings: embodied, intelligent, and free, with dignity grounded in their capacities, within the concrete circumstances of their lives, to pursue the true good and avoid evil through rational, intelligent, and free choices.
Accordingly, fertility and sexuality are essential aspects of human embodied nature to be used to pursue good. This understanding of the human person means that marital sexual acts, too, unite the bodily and the spiritual. Marital sexual acts have, at once, a bodily or procreative significance—they are bodily acts capable of procreating a new human being—and a spiritual or unitive significance—they are acts of loving union. For the marital act to respect this united nature, husband and wife must engage in sexual intercourse in a way that incorporates both of its meanings (love and procreation), neither procreating like the lower animals—driven by instinct rather than by intelligent love—nor producing life through reproductive techniques that jettison personal bodily union.
Only marriage is considered an appropriate context for the conception of a new human person. The child who is to be conceived is understood to have the right to be conceived, gestated, born into, and raised within marriage, and marriage is understood to entail only becoming a parent with one’s husband or wife. Intrauterine insemination (IUI) and in vitro fertilization (IVF) deprive the child of these circumstances of conception, and, when assisted reproduction techniques use donor gametes, they prevent the couple from becoming parents only through each other. Furthermore, IVF also fails to respect these concepts of human life and bodily integrity by destroying embryonic human beings because of their morphological or genetic abnormalities and by suspending lives through cryopreservation [20]. Upholding this rationally intelligible context for human procreation defines the parameters of NaProTECHNOLOGY.
This procreative ethics requires husband and wife to use their procreative capacities virtuously and responsibly, that is, in a way that furthers relevant concepts of the good. If a couple conscientiously judge the infertility treatment they are considering moral—if they believe it promotes their human flourishing by enabling them to conceive within their own acts of loving bodily union and, therefore, respects their dignity, that of the child to be conceived, and that of their marital acts—they should pursue it. But should the couple conscientiously decide the infertility treatment they are considering is immoral—that it represses their human flourishing by consigning human procreation to an impersonal, sterile and, in the case of IVF, extra-bodily technical process—they should not pursue it.
Similarly, if a physician conscientiously judges that he or she should not provide IUI, IVF, and their variations since these reproductive techniques wrest human procreation from the marital act of intercourse, he or she should avoid it. NPT medical and surgical infertility protocols, on the other hand, accord with these concepts of the personal and procreative dignity of the infertile couple, since they enable them to conceive within their own acts of intercourse.
So, the good news is this: It is possible for physicians who hold the beliefs we detail here to practice medically sound obstetrics and gynecology in line with their well-formed consciences and those of their patients. It is possible to provide medically effective reproductive interventions that also genuinely promote this concept of bodily-spiritual well-being for both patient and physician. In other words, it is possible for physicians who hold these beliefs to honor the capital principle of beneficence that medical codes of professional ethics insist is central to the physician-patient relationship.
References
-
ACOG Practice Bulletin No. 110: Noncontraceptive uses of hormonal contraceptives. Obstet Gynecol. 2010;115(1):206-218.
-
Fertility: Assessment and Treatment for People with Infertility Problems. National Institute for Clinical Excellence; 2004. http://www.nice.org.uk/nicemedia/pdf/CG011niceguideline.pdf. Accessed November 30, 2012.
-
Stanford JB. Outcomes from treatment of infertility with natural procreative technology in an Irish general practice. J Am Board Fam Med. 2008;21:375.
-
Adashi EY. Fertility following bilateral ovarian wedge resection: a critical analysis of 90 consecutive cases of the polycystic ovary syndrome. Fertil Steril. 1981;36:320.
- Mais V, et al. Prevention of postoperative abdominal adhesions in gynecological surgery. Consensus paper of an Italian gynecologists’ task force on adhesions. Minerva Ginecol. 2011;63(1):47-70.
-
Hilgers, TW. The Medical & Surgical Practice of NaProTECHNOLOGY. Omaha, NE: Pope Paul VI Institute; 2004;1001-1005.
-
Hilgers TW. Near adhesion-free reconstructive pelvic surgery: three distinct phases of progress over 23 years. J Gyn Surgery. 2010;26:31.
- Somigliana E, et al. Adhesion prevention in endometriosis: a neglected critical challenge. J Minim Invasive Gynecol. 2012;19(4):415-421.
-
Somigliana, et al., 415.
- Moragianni VA, Penzias AS. Cumulative live-birth rates after assisted reproductive technology. Curr Opin Obstet Gynecol. 2010;22(3):189-192.
-
Hilgers, The Medical and Surgical Practice of NaProTECHNOLOGY, 679.
-
Hogan JW. Identifying and addressing data-analytic challenges in IVF and ART. International Symposium on Frontiers and Reproductive Technology Serona Symposia USA; March 27-31, 2001: Washington, DC.
-
Campbell JS, Pasta DJ, Adamson GD. Preliminary meta-analysis comparing in-vitro fertilization with surgical treatment for moderate and severe endometriosis. J Am Assoc Gynecol Laparosc. 1995;2:s6-s7.
-
Hilgers, The Medical & Surgical Practice of NaProTECHNOLOGY, 690.
-
Pope Paul VI Institute. FertilityCare allied health education. Accessed February 20, 2012.
-
Applications for the NaProTECHNOLOGY fellowship are available by request from [email protected].
-
For an in-depth discussion of conscience, see Mirkes R. The ethics of infertility treatment: an upbeat update. In: Furton EJ, ed. Live the Truth: The Moral Legacy of John Paul II in Catholic Health Care: Proceedings of the Twentieth NCBC Workshop for Bishops.Philadelphia: National Catholic Bioethics Center; 2006: 203-231.
-
For an in-depth discussion of the practice of conscientious reproductive medicine, see Mirkes R. Protecting the right of informed conscience in reproductive medicine. J Med Philos. 2008;33(4):374-393.
-
Keefe CE, Mirkes R, Yeung P. the evaluation and treatment of cervical factor infertility: a medical-moral analysis. Linacre Q. In press.
-
Pellegrino ED, Thomasma DC. The Virtues in Medical Practice. New York: Oxford University Press, 1993.
-
Congregation for the Doctrine of the Faith. Instruction on respect for human life in its origin and on the dignity of procreation. 1987. http://www.vatican.va/roman_curia/congregations/cfaithdocuments
rc_con_cfaith_doc_19870222_respect-for-human-life_en.html. Accessed February 20, 2013. -
Pope Paul VI. Humanae Vitae. 1968. http://www.vatican.va/holy_father/paul_vi/encyclicals/documents/hf_p-vi_enc_25071968_humanae-vitae_en.html. Accessed February 20, 2013.
-
John Paul II. Original Unity of Man and Woman: Catechesis on the Book of Genesis. Boston, MA: Daughters of Saint Paul; 1981.
-
John Paul II. Blessed are the Pure of Heart. Boston, MA: Pauline Books and Media; 1988.
-
John Paul II. Celibacy: Catechesis on Marriage and Celibacy in the Light of the Resurrection of the Body. Boston, MA: Pauline Books and Media; 1986.
-
John Paul II. Veritatis Splendor. Vatican City, 1993.
-
Rhonheimer M, Murphy WF, eds. Ethics of Procreation and the Defense of Human Life. Washington, DC: The Catholic University of America Press; 2010.