Despite considerable evidence of harm from poor dietary choices, many Americans continue to make them. The reasons for our collective unhealthful diet are complex and probably vary considerably among individuals. For some Americans, poor diets may stem from a lack of access to better options [1]. For others, there may be a component of addiction-like behavior driving their intake [2]. Most of us would probably assert, though, that our diets reflect conscious choices about what we like to eat and what’s most convenient for us.
Regardless of the reasons for poor diet, the consequences of our consumption patterns are significant. In the past few decades, there has been explosive growth in the rates of two conditions directly linked to overconsumption of calorie-dense foods—obesity and diabetes. Once developed, these conditions are difficult to treat with medication or lifestyle changes, and affected patients may increasingly require invasive and expensive procedures previously reserved for only the most extreme cases. In order to ensure that the U.S. population is healthy and productive, and to avoid further crippling our economy with ballooning medical costs from diet-related disease, comprehensive and sustainable changes to American dietary habits are needed.
Changes can be attempted in a number of ways, but in general there are two possible approaches: those that target the individual and those that target the population [3]. Individual-level interventions are tailored to one person or family’s needs; for example, a dietitian’s teaching a client what kinds of foods to eat in order for her to lose weight and prevent diabetes, or, more extreme, a bariatric surgeon resecting the patient’s stomach to achieve the same goals. Population-level interventions, on the other hand, target the behavior of an entire group of people through policy changes, without specific attention to individual circumstances.
Millions of Americans are at risk of developing chronic disease due to their dietary habits or are already affected—can you imagine using longitudinal, tailored medical approaches to successfully change the behaviors of each of these people? That kind of intervention would require enormous amounts of time and funding, neither of which is currently in abundant supply [4]. Purely individual-level approaches to preventing and ameliorating the effects of diet-related disease are not likely to be cost-effective, which suggests that population-level or policy approaches would increase the efficiency with which resources are used [5, 6]. Developing food policy, however, is not merely an issue of feasibility or effectiveness. It is also necessary to examine the ethics of using population-level approaches to solve what many politicians and citizens believe to be an individual-level behavioral problem.
In order to do this, it’s worth separating food policies into two general categories, each with very different ethical implications. First are policies that rely on active behavior change by individuals in order to be effective (we’ll call this the “loose” end of food policy), and second, those that automatically change behavior (we’ll call this the “tight” end of food policy). Loose policies could take the form of educational interventions like ad campaigns and school-based programs that provide information to everyone regardless of personal behavior or beliefs, but ultimately rely on individuals to both understand and comply with the message (i.e., it still comes down to the notion of “personal responsibility” and an active choice). Even something like a soda tax could be considered a loose policy; I can still buy a sugary soda if I want one, but the slightly higher price tag might make me think twice about it.
Policies on the tight end of the spectrum, in contrast, remove the option for personal choice, putting responsibility entirely in the hands of the government or other mandating body. New York’s ban on trans fats in restaurants or the removal of red dye #3 by the FDA in the early 1990s are two examples of using a “tight,” mandatory policy to change eating behavior. Rather than requiring action by individuals to be effective, these policies required action at the level of the food producer or supplier, thereby removing the opportunity for individual choice.
The Ethics of “Loose” Dietary Policies
Loose policies that are limited to educational initiatives, particularly if the messages are framed positively (e.g., “Drink more water” instead of “Don’t drink soda”) tend not to generate much friction from an ethical or personal liberties standpoint. Even the most ardent libertarian would argue that consumers’ rights are not violated by the provision of information in order to facilitate good dietary choices. Unfortunately, purely educational policies that generate little political resistance are also likely to generate little change (see figure 1) [6-8]. Providing consumers with information about their dietary choices is an important step, but it’s unlikely to succeed on its own.
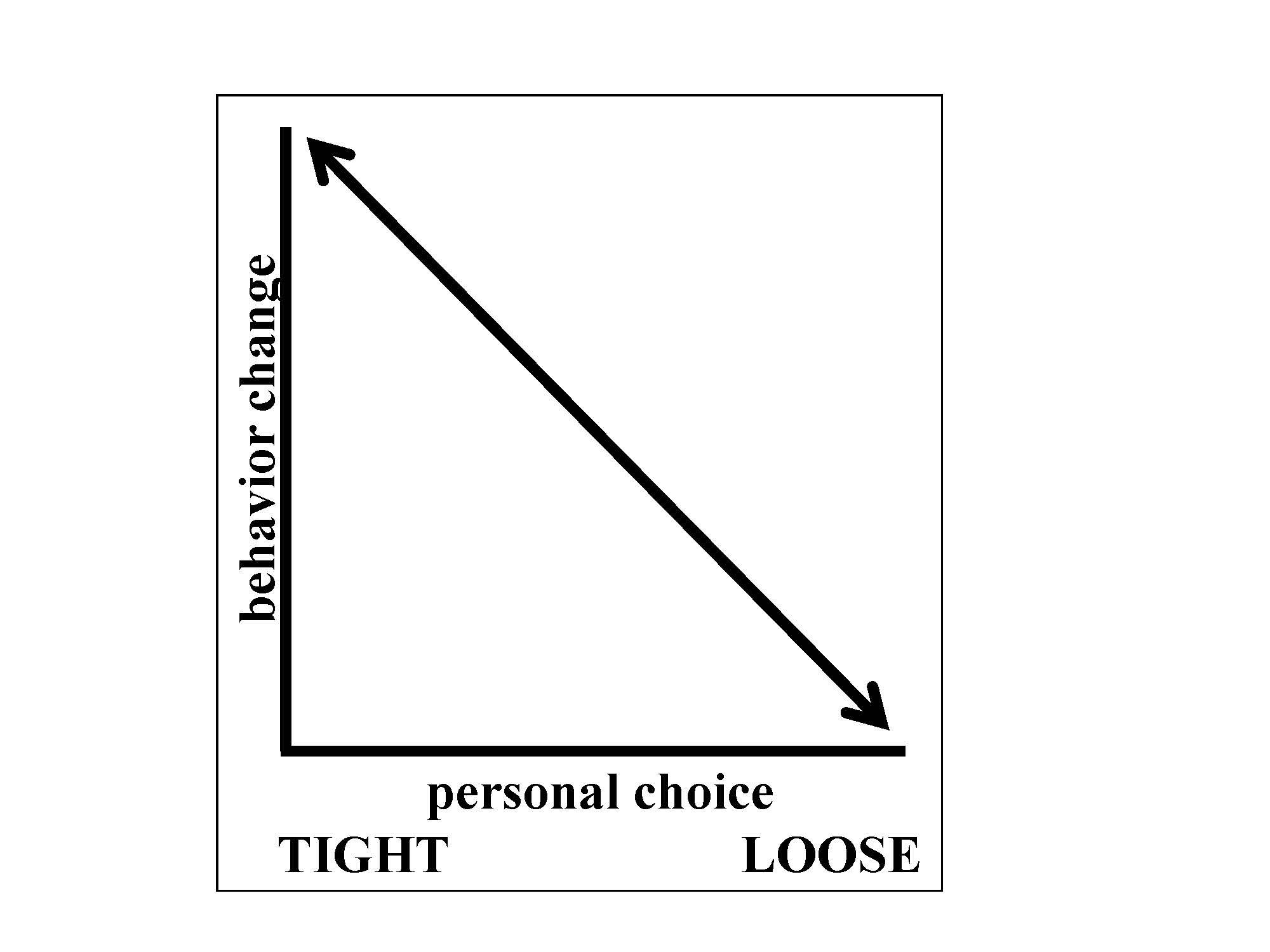
Figure 1. The inverse relationship between protection of personal choice and impact on behavior change as it pertains to food policy.
To achieve more widespread behavior change, informational policies may need to be augmented by more directive policies, such as taxing sugar-sweetened beverages (SSBs). Using SSBs as an example, a tax makes sense from an economic perspective: increase price to drive down demand (and therefore consumption) of products you don’t want people to eat or drink. One can even justify the government’s intervention in the marketplace by virtue of the externalities associated with SSB consumption (chronic disease, e.g.) that are not currently accounted for in the cost of these products [5]. From an ethical perspective, however, things are a little trickier. Whenever a soda tax is discussed, one of the reflex arguments against it is that is unethical because it is regressive. Because sodas are disproportionately consumed by people of lower socioeconomic status, goes this argument, and because the beverages favored by economically better-off people will not be taxed, the poor will bear the burdens of the tax disproportionately. Alternately, even if the poor are not the main or only consumers of soda, the tax will be more likely to “work” on them—to dissuade them from drinking soda, depriving them of the pleasure their better-off fellows derive from it—than on those who are better off.
If we expand on the idea of so-called “sin taxes” to include junk foods such as candy, chips, and other calorie-dense, low-nutrient foods, we quickly find ourselves on a slippery slope where the notion of a regressive tax seems very concerning indeed. For people of low socioeconomic status (SES) who do not have good access to healthful foods, junk food may be the primary source of calories, and, while it is unhealthfu for them in the long-term, it is necessary for survival in the short term. Furthermore, what might be an imperceptible price change to many could be a real shock for a person living in poverty. Thus, without ensuring that those living in poverty have access to healthy and affordable alternatives, policy makers might inadvertently make it harder for them to afford to feed their families by passing an ill-planned junk food tax.
The Ethics of “Tight” Dietary Policies
Mandates—dietary policies on the “tight” end of the spectrum—directly limit consumer choice by, for example, banning an ingredient or an entire product. Although such policies could have a profound effect on the population’s diet, they are viewed by many as too extreme.
Opponents of dietary mandates state that it is not the government’s place to interfere in the personal choices of consumers. They believe individuals should be able to eat whatever they want and that, if they are aware of the potential health consequences, their diets are their own responsibility. By this same logic, if individuals assume complete ownership of their dietary choices, they should also be held responsible for the consequences of those choices. If the healthy present-day “me” eats a dozen donuts every day for 20 years, the future sick “me” should not then expect society to bear the costs of my diabetes and coronary disease, right?
As a society and a profession, however, we’ve decided that those who cannot afford medical care should not die for lack of it, whether or not their condition is a result of their own behavior. As long as that philosophy remains in place, the cost of caring for diet-related illness will probably continue to rise. Eventually, difficult choices will need to be made about what gets paid for and by whom. If the harm caused to society by limiting consumption on the front end is perceived to be less than that caused by limiting medical care on the back end, a resource conservation argument can be made for some dietary mandates (e.g., trans fat ban). It is important to keep in mind, though, the tension between protecting the public’s health and the damage that can be done by removing an individual’s freedom. Mandates are least likely to ruffle feathers when they’re applied to substances that have clear adverse health effects if consumed in anyamount (e.g., trans fats, as opposed to sodium), and those (e.g., red dye #3) for which there are available and comparable substitutes.
A related argument against the banning or direct limitation of certain products is that, while health consequences do result from the overconsumption of unhealthful items, not everyone overconsumes, and, of those who do, not everyone has health consequences. Stated another way—why should responsible, moderate consumers be prevented from drinking Big Gulps because others overconsume them? The same argument is often applied elsewhere—why should responsible gun owners be deprived of their weapons because other gun owners engage in criminal behavior? Why should individual children accept the risks of vaccination to ensure herd immunity? These sentiments express dismay at the prices we pay for living in a democratic society—sometimes what is good for the group might not be the thing we’d like best as individuals. Each of us has a different level of willingness to sacrifice personal liberties for our own good or the good of the population.
The Notion of Personal Freedom in Food Choice
So far, in discussing the various ways that dietary policy might infringe upon personal rights, I’ve been operating under the assumptions that most Americans’ eating habits are based on free choice and that the food marketplace is structured merely to respond to consumer demand.
In reality, there are many Americans who don’t have free choices about their diets. The most extreme case is that of children, whose parents and schools make dietary choices for them, and poor adults who live in food deserts and cannot access or afford to purchase nutritious food. Even the rest of us who supposedly “choose” to engage in dietary indiscretions aren’t actually making completely free choices. As far as food products go, we’re heavily influenced by advertising (hence the hefty budgets dedicated to it by food companies), by price ($0.99 for a hamburger or $3.50 for a salad?), and by the formulations of processed foods, which can appeal to a person’s palate much more strongly than “whole” foods. Price is heavily influenced by the cost of ingredients, in turn influenced by agricultural policies from seed technology to subsidies. We eat a lot of corn syrup not because we love the stuff and demand that manufacturers give it to us, but because farmers know how to grow corn well, it’s subsidized, and therefore corn syrup makes for a much cheaper way for food manufacturers to sweeten their products than using sugar cane.
So, think about it carefully. Is it really your choice to buy that corn syrup-laden candy bar in the grocery store checkout line, or is it an act of impulsivity due to convenience, cost, taste, and proximity (maybe even boredom)? What are your other options? When was the last time you saw an apple, banana or even a bag of trail mix sitting there in the checkout line next to the tabloids? In other words—when you decide what to eat, are you really buying what you want after considering all of your options, or are you just buying what someone else is selling you?
Conclusion
Although policy solutions will likely be necessary to facilitate population wide changes in diet, finding ethical solutions that help more than they harm is going to be complicated. As a policy rises on the effectiveness spectrum, it also generally moves further toward the “restrictive” end of the personal rights spectrum. The key for policy makers is finding the sweet spot between these two opposing interests. That spot will vary depending on what legislation is being considered. For something like trans fats, an intrusive but effective policy was probably justified due to the significant health risks trans fats posed, combined with the ready availability of substitutes. On the other hand, if the government were to try to rid the market of all sugar, there would be angry riots on the Capitol steps.
Before any honest discussion of infringing personal liberties can be entertained, however, the playing field must be leveled when it comes to consumer choice. Until healthful food is widely affordable and accessible to all people, any discussions of how policy might infringe on the right to choose may be misguided.
References
-
Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev. 2009;31:7-20.
- Davis C, Curtis C, Levitan RD, Carter JC, Kaplan AS, Kennedy JL. Evidence that ‘food addiction’ is a valid phenotype of obesity. Appetite. 2011;57(3):711-717.
-
Lewis KH, Rosenthal MB. Individual responsibility or a policy solution--cap and trade for the U.S. diet? N Engl J Med. 2011;365(17):1561-1563.
-
Yarnall KS, Pollack KI, Ostbye T, Krause M, Michener JL. Primary care: is there enough time for prevention? Am J Public Health.2003;93(4):635-641.
- Chokshi DA, Farley TA. The cost-effectiveness of environmental approaches to disease prevention. N Engl J Med. 2012;367(4):295-297.
- Gortmaker SL, Swinburn BA, Levy D, et al. Changing the future of obesity: science, policy, and action. Lancet. 2011;378(9793):838-847.
- Elbel B, Kersh R, Brescoll VL, Dixon LB. Calorie labeling and food choices: a first look at the effects on low-income people in New York City. Health Aff (Millwood). 2009;28(6):w1110-w1121.
- Mozaffarian D, Afshin A, Benowitz NL, et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126(12):1514-1563.



