Introduction
The magnitude of unmet need for neurosurgery in the developing world is staggering. It is estimated that 2 billion people worldwide lack adequate access to basic surgical care [1], and access to neurosurgical care is even more restricted. For example, the ratio of neurosurgeons to population is 1 to 62,500 in the United States and 1 to 6.4 million in sub-Saharan Africa [2, 3]. In many low- and middle-income countries (LMICs) with some capacity to provide neurosurgical care, subspecialized neurosurgery—such as vascular, functional, epilepsy, and pediatric—is altogether unavailable, and regional disparities may prevent most citizens from accessing available services. Diseases treatable with neurosurgery may be associated with considerable disability and the consequent social stigma [4, 5], robbing individuals and communities of years of productive livelihood. It is not surprising, therefore, that surgical care is increasingly understood to represent a critical component of primary care in LMICs [6-8] and to augment multiple domains of health care [9].
Various models of international aid have been proposed to address the large unmet need for neurosurgical care on the part of the planet’s most vulnerable citizens. We categorize the extant models of neurosurgical international aid on the basis of two components: the depth of the commitment and the breadth of applications provided to the LMIC (see figure 1).
Figure 1. Types of neurosurgery international aid.
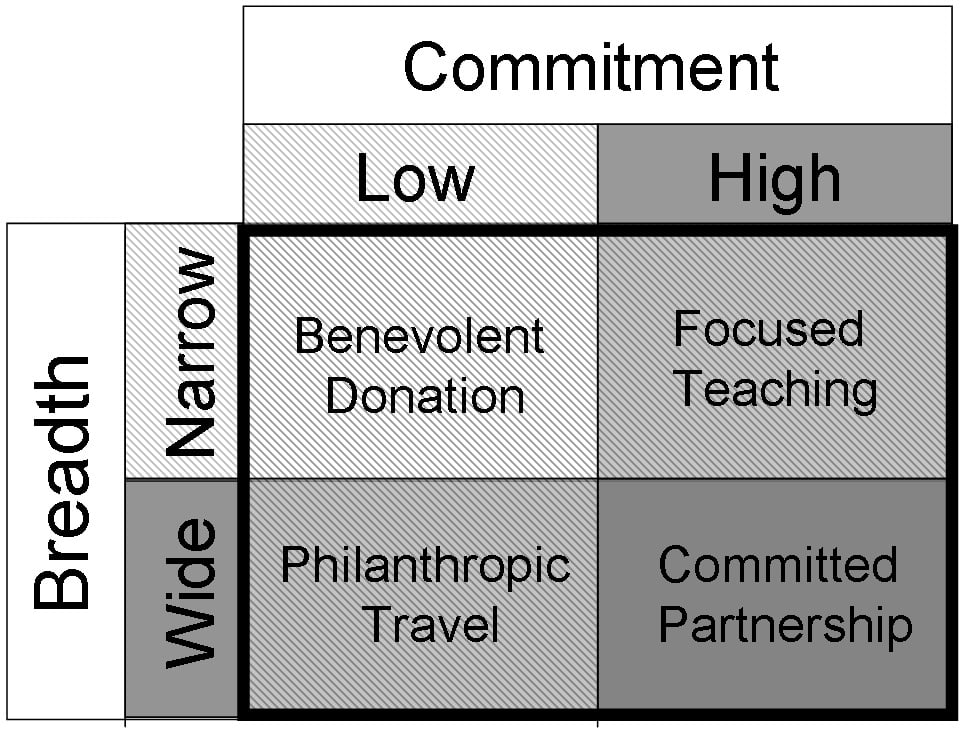
The first model, benevolent donation, refers to the giving of material goods to LMICs; little commitment is involved and the uses of the equipment of goods are often narrowly specific. The second model, philanthropic travel, is characterized by a higher, though still limited, commitment: individuals or groups make short trips to one or more countries to perform or teach as many kinds of neurosurgery as possible; the breadth of skills and applications covered is wide. The third model, focused teaching, describes the making of (typically, but not necessarily, repeated) trips to LMICs to teach a single skill set; the commitment is high and the breadth is narrow. Finally, the fourth model, committed partnership, consists of long-term institutional collaborations between centers in developed countries and LMICs; both the level of commitment and the breadth of applications are high. Here, we summarize these models of providing neurosurgical care in LMICs and discuss ethical challenges and pitfalls associated with each.
Benevolent Donation
The first model of neurosurgery as international aid is the donation of material goods, mainly equipment, to LMICs with variable follow-up and support. This model has been adopted by numerous national and supranational organizations. For example, The United States Agency for International Development (USAID) donated a computed tomography scanner to the CURE Children’s Hospital of Uganda in 2004 [10]. This donation allowed clinicians at the hospital to identify and treat previously undiagnosed diseases amenable to neurosurgical treatment. Such an important basic tool is a rare commodity]; there were only three CT scanners outside Uganda’s capital city as recently as 2011 [10].
Although there is clearly a role for this model of international aid, its limitations are self-evident and raise ethical questions. Do such contributions actually do good? In the aforementioned example, the donation allowed CURE Children’s Hospital of Uganda to expand its capacity and operations by more rapidly diagnosing conditions and expediting appropriate treatments. There are numerous other examples, however, of material donations that are inappropriate for the resource-limited settings, e.g., because they are costly to repair or their use is prohibitively expensive for the local population. In the former circumstance, if equipment breaks down, possibly futile efforts to fix it can drain already quite limited resources. In the latter circumstance, a $60 CT scan, for example, may be beyond the means of the majority of citizens in LMICs [10]. Well-intentioned donations of goods therefore may not actually increase access to health care. A thorough assessment of the sustainability and overall impact of material goods must be performed prior to donation.
Philanthropic Travel
The second, classic model of neurosurgery-related international aid is one in which surgeons or surgical teams make short trips to perform surgery and teach techniques to local surgeons [11-13]. In some cases, participants visit the same location multiple times, which has the added advantage of longitudinal follow-up and monitoring of the initiative’s impact.
There are ethical challenges inherent to this model. Sustainability is a major issue. Some initiatives do not include teaching; merely performing occasional operations on citizens of LMICs does little to improve the overall state of public health and may even lead to poor clinical outcomes [14]. Even if the initiative includes teaching, will the local team be able to perform the procedures independently after the visitors leave [15]? Contributing to these problems is the lack of coordination among international neurosurgical initiatives, of which there are an increasing number. There should be continuity of teaching aided by documentation of accomplishments and challenges at each center so that vital resources are not wasted on redundant or unnecessary teaching.
Other ethical challenges of this model have been categorized loosely as related to the venue and the visitor [15]. The former include the possible diversion of resources from other local priorities, choosing a location that mitigates regional disparities in access to care, and difficulties in ensuring proper informed consent. Among the most important resources in LMICs are highly trained local physicians. By involving them in specific projects related to neurosurgery during a philanthropic visit, one may inadvertently divert their attention from other worthwhile priorities, such as treatment of diseases that do not require surgery. The choice of location is also an important consideration given that certain subpopulations in LMICs, including those in rural areas, are disproportionately affected by disparities in access to surgical care. The location of the mission should aim to mitigate local inequities in access to health care rather than reinforce them. Finally, while a thorough discussion of informed consent in LMICs is beyond the scope of the current article, it is necessary to appreciate that cultural and social factors and resource constraints may modify the three elements of informed consent—voluntariness, capacity, and lack of undue influence.
The latter ethical challenges include the choice of team members (for instance, whether to include allied health professionals such as physiotherapists as part of the mission) and conflicts of interest that may arise if the visit is sponsored by organizations with financial, social, or political interests. While surgery is important, patients with diseases treatable with neurosurgery often also require prolonged follow-up and rehabilitation. It may be ethically dubious—and indeed a disservice to patients—to facilitate the provision of neurosurgery without augmenting the capacity to care for patients following it. The incorporation of a multidisciplinary team as part of the international mission can bridge such gaps in patient care and improve overall patient outcomes. In order to mitigate many of these challenges, an “ethical checklist” has been proposed that gives a priori consideration to them [15].
Focused Teaching
The third model is a variant of philanthropic travel in which surgeons travel to LMICs to teach a narrow, specific skill set. A prime example is teaching local surgeons in developing countries how to perform awake craniotomy [11]. The purposes of this specific skill set are to decrease reliance on intensive care beds and general anaesthesia and to improve patient safety in resource-poor settings [16].
Teaching a narrow (as opposed to a broad) skill set is associated with specific ethical advantages and pitfalls. One significant advantage is the ability to rapidly expand capacity and to perform a particular procedure more efficiently. This may result in decreased morbidity and increased access to care. This is evident in Uganda, where the CURE Children’s Hospital has become a regional referral center for childhood hydrocephalus and has seen greatly improved outcomes, expanded access, and long-term postoperative follow-up of patients [17, 18].
The most significant ethical challenge is prioritizing a small subset of diseases for neurosurgical treatment in settings where there is great need for generalized care. Patients whose need for neurosurgical attention is emergent (for example in the setting of trauma or other life-threatening conditions) may require care that the center is unable—or lacks the funding—to provide it. To overcome these challenges, some surgeons focus on narrow, specific skill sets with broad applications, such as the aforementioned awake craniotomy.
In addition, a comprehensive analysis must be performed to ensure that the intervention is appropriate, sustainable, and desired by the local surgeons. One successful implementation of this strategy was the teaching of endoscopic third ventriculostomy and choroid plexus cauterization (ETV/CPC) for cases of childhood hydrocephalus in Uganda [17, 18]. Prospective databases and outcome recording established that this intervention was indeed beneficial and resulted in greater overall good than harm [17, 18]. The result of this endeavor is a reverse innovation phenomenon whereby the procedure is now gaining greater prominence in the developed world [19].
Committed Partnership
The final model, partnerships between surgical centers in developed countries and LMICs, involves a very significant commitment to a broad group of goals. One example of such a consensual partnership is the East African Neurosurgical Research Cooperative, which was formed by regional centers to advance global health development in neurosurgery [20]. The “twinning” of individual centers in developed countries and LMICs involves continuous support and outcome evaluation and monitoring [21].
This is an excellent model, doing much more than the others to develop and ensure sustainability, but it may have its own ethical challenges. First, it can be unclear what both parties’ responsibilities are if the relationship becomes ineffective or conflicts arise. Such agreements typically also include provisions for the education of surgeons from LMICs in the developed world, which may be associated with specific challenges concerning the appropriateness of certain skills for a given context. For example, microsurgical clipping of an aneurysm may not be relevant in certain LMICs where patients with ruptured aneurysms cannot be treated due to the lack of intensive care expertise, diagnostic equipment such as angiography suites, and equipment such as an operating microscope or microinstruments.
Furthermore, the roles of sponsors and conflicts of interest must also be clearly examined at the onset of the partnership. Typically, committed partnerships are resource-intensive. Their ultimate goal is to allow the local centers in LMICs to become self-sufficient, which may not be achievable if all the funding stems from sponsors in the developed world. Additionally, any perceived conflicts of interest—for instance, from the involvement of pharmaceutical or biomedical companies—will undermine the trust that is necessary to establish such a partnership. Both parties must be aware of and agree to how funds will be generated and consider the long-term sustainability of the endeavor as well as find ways to empower the LMIC center to advance and grow until it becomes self-sufficient.
Discussion and Conclusions
An important consideration for all models is their impact. At present, there are no accepted guidelines or metrics to monitor and evaluate the impact of international neurosurgical initiatives. While the response to the neurosurgical needs of LMICs through various models of international aid is gaining momentum, it is increasingly important to audit and review the results of those initiatives to foster accountability to local surgeons, funding agencies, and visiting teams. At the very least, visiting surgeons must be aware of the potential ethical pitfalls inherent in their chosen paradigm of surgical aid and strive to resolve them to improve access, equity, sustainability, and informed consent processes.
References
- Funk LM, Weiser TG, Berry WR, et al. Global operating theatre distribution and pulse oximetry supply: an estimation. Lancet. 2010;376(9746):1055-1061.
- El Khamlichi A. The World Federation of Neurosurgical Societies Rabat Reference Center for Training African Neurosurgeons: an experience worthy of duplication. World Neurosurg. 2014;81(2):234-239.
- El Khamlichi A. African neurosurgery: current situation, priorities, and needs. Neurosurgery. 2001;48(6):1344-1347.
- Cadotte DW, Viswanathan A, Cadotte A, et al. The consequence of delayed neurosurgical care at Tikur Anbessa Hospital, Addis Ababa, Ethiopia. World Neurosurg. 2010;73(4):270-275.
-
Bramall A, Djimbaye H, Tolessa C, Biluts H, Abebe M, Bernstein M. Attitudes towards neurosurgery in a low-income country: a qualitative study [published online ahead of print May 14, 2014]. World Neurosurg. doi: 10.1016/j.wneu.2014.05.015.
- Farmer PE, Kim JY. Surgery and global health: a view from beyond the OR. World J Surg. 2008;32(4):533-536.
-
Gosselin RA, Thind A, Bellardinelli A. Cost/DALY averted in a small hospital in Sierra Leone: what is the relative contribution of different services? World J Surg. 2006;30(4):505-511.
-
Hackenberg B, Ramos M, Campbell A, et al. Measuring and comparing the cost-effectiveness of surgical care delivery in low-resource settings: cleft lip and palate as a model [abstract]. Can J Surg. 2014;57(3)(suppl 1):S9. http://canjsurg.ca/wp-content/uploads/2014/06/57-3-S1.pdf. Accessed November 24, 2014.
-
PLoS Medicine Editors. A crucial role for surgery in reaching the UN millennium development goals. PLoS Med. 2008;5(8):e182.
-
Dewan MC, Warf BC, Mugamba J. Diagnosing Dandy-Walker Complex by computed tomography: experience in Uganda and recommendations for hospitals in resource-limited settings. J Global Health. 2011. http://www.ghjournal.org/diagnosing-dandy-walker-complex-by-computed-tomography-experience-in-uganda-and-recommendations-for-hospitals-in-resource-limited-settings/. Accessed November 24, 2014.
- Howe KL, Zhou G, July J, et al. Teaching and sustainably implementing awake craniotomy in resource-poor settings. World Neurosurg. 2013;80(6):e171-e174.
- Bernstein M. Ethical dilemmas encountered while operating and teaching in a developing country. Can J Surg. 2004;47(3):170-172.
-
Bedada AG, Hsiao M, Bakanisi B, Motsumi M, Azzie G. Establishing a contextually appropriate laparoscopic program in resource-restricted environments: experience in Botswana [published online ahead of print June 9, 2014]. Ann Surg. doi: 10.1097/SLA.0000000000000691.
- Isaacson G, Drum ET, Cohen MS. Surgical missions to developing countries: ethical conflicts. Otolaryngol Head Neck Surg. 2010;143(4):476-479.
- Howe KL, Malomo AO, Bernstein MA. Ethical challenges in international surgical education, for visitors and hosts. World Neurosurg. 2013;80(6):751-758.
-
Ibrahim GM, Bernstein M. Awake craniotomy for supratentorial gliomas: why, when and how? CNS Oncol. 2012;1(1):71-83.
- Warf BC, East African Neurosurgical Research Collaboration. Pediatric hydrocephalus in East Africa: prevalence, causes, treatments, and strategies for the future. World Neurosurg. 2010;73(4):296-300.
- Warf BC. Hydrocephalus in Uganda: the predominance of infectious origin and primary management with endoscopic third ventriculostomy. J Neurosurg Pediatr. 2005;102(1):1-15.
- Kulkarni AV, Riva-Cambrin J, Browd SR, et al. Endoscopic third ventriculostomy and choroid plexus cauterization in infants with hydrocephalus: a retrospective Hydrocephalus Clinical Research Network study. J Neurosurg Pediatr. 2014;14(3):224-229.
- Hartl R, Ellegala DB. Neurosurgery and global health: going far and fast, together. World Neurosurg. 2010;73(4):259-260.
- Haglund MM, Kiryabwire J, Parker S, et al. Surgical capacity building in Uganda through twinning, technology, and training camps. World J Surg. 2011;35(6):1175-1182.



