Autism is a complex neurodevelopmental disorder characterized by marked impairments in the ability to interact socially combined with restrictive, repetitive patterns of behavior. Only a few decades ago, the disorder appeared to be relatively uncommon, with a reported prevalence of roughly 3 in 1,000 children prior to 1990 [1]. The most recent prevalence estimate from 2010 indicates that it affects 1 in 68 children in the US [2]. Autism often has profound negative impacts for affected children, their families, and their communities. Most children with moderate to severe autism spectrum disorder will have lifelong impairments in social skills; difficulties in school; cognitive challenges; increased rates of anxiety, depression, and obesity; and decreased rates of employment and independent living [3]. Family members also have higher rates of anxiety, stress, mental illness, and lost productivity due to their child’s special needs [4].
Unfortunately, effective treatments for autism have been elusive. The mainstay of therapy is intensive behavioral intervention—given for 20 or more hours per week—which has been shown to produce important benefits, but response to treatment varies widely, and it is challenging to predict which children will respond [5]. Only two drugs have been approved by the US Food and Drug Administration for the treatment of autism—risperidone and aripiprazole—and both target an associated behavior problem, irritability, rather than the core deficits in social skills and repetitive behavior [6]. Both drugs also have significant side effects, including weight gain and sedation.
It is no surprise, therefore, that parents seek complementary and alternative medicine (CAM) therapies to try to help their affected children. Numerous surveys of parents have found that a very high percentage of children with ASD—up to 95 percent in one study—were using CAM therapies for general health or to improve symptoms of ASD or associated symptoms such as irritability, hyperactivity, GI problems, and sleep disturbances [7-9]. Initially, many considered the therapies classified as CAM to be ineffective, sometimes dangerous, often expensive, and potentially distracting for parents, who often implement the time-consuming but sometimes ineffective behavioral programs. Secretin, for example, is an expensive intravenous drug that was studied in seven randomized controlled trials before all the evidence was systematically reviewed and it was conclusively determined to be ineffective [10]. Chelation therapy is a CAM treatment promoted to remove heavy metals from the blood; it can be dangerous and there is no convincing evidence of efficacy [11]. These high-profile examples of ineffective or dangerous CAM therapies led to a general mistrust of and distaste for anything believed to be a CAM treatment for ASD.
CAM for Abnormal Physiology
But the tide is beginning to shift as evidence accumulates that some CAM therapies are addressing abnormal physiology in autism. Autism is now known to be associated with a number of physiological abnormalities that have been classified into four broad categories: oxidative stress, inflammation or immune dysregulation, mitochondrial dysfunction, and environmental toxicant exposure [12]. CAM therapies that improve these physiological abnormalities hold promise for improving symptoms. Extensive reviews of the evidence for all CAM therapies in ASD have recently been published [13], and a few compelling examples are worthy of discussion.
Oxidative stress refers to an imbalance in the generation and detoxification of reactive oxygen and nitrogen species, mediators known to be associated with cell damage. These reactive oxygen species are a normal part of human physiology, but, if they are not removed appropriately, they accumulate and lead to protein, DNA, and cell damage. Several investigations have found evidence of abnormal oxidative stress in children with autism, including laboratory biomarkers of decreased antioxidant enzymes (e.g., superoxide dismutase, transferrin, and ceruloplasmin) and elevations in biologic measures of oxidative stress (including increased lipid peroxidation and impaired plasma methionine methylation capacity) [14, 15]. Whether abnormal biomarkers indicate a cause or are an effect of autism is not known. Regardless, children with autism who have more oxidative stress have been found to have more severe symptoms [16].
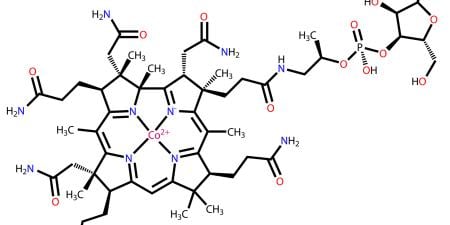
Two CAM treatments—N-acetylcysteine (NAC) and methylcobalamin (B12)—target the problem of oxidative stress. NAC is available over the counter and, when given systemically, acts as a direct antioxidant and an efficient prodrug (an inactive drug converted to an active substance by the body’s metabolic processes) for cysteine, which is a key component of the antioxidant system in the body [17]. A recent, small 12-week randomized placebo-controlled trial showed that NAC is able to reduce irritability in children with autism [18], as are the two approved antipsychotic drugs [19, 20], but with no observed side effects.
Vitamin B12 is a vital cofactor in the antioxidant system that spurs the regeneration of methionine from homocysteine. In a small pilot randomized controlled trial of 30 children with ASD, B12 injections did not improve overall outcomes, but a subset of children supplemented with B12 showed improvements in both measures of oxidative stress and clinical symptoms [21]. This result led to a recent, larger randomized controlled trial that has been completed by our group at the University of California, San Francisco, and initial (unpublished) results suggest that B12 is also effective in improving overall symptoms. Together, the early studies of NAC and B12 are promising examples of CAM therapies that accord with physiological models and are supported by initial evidence.
Inflammation, too, has been shown to respond to a CAM treatment. Perhaps the most exciting treatment study in autism published recently involved a mouse model and treatment with probiotics [22]. Pregnant mice were injected with a chemical (polyinosinic-polycytidylic acid) that stimulates a response similar to a viral infection, which reliably produces infant mice with symptoms that mimic human autism including impaired ability to socialize and repetitive behaviors. Affected mice were also found to have increased intestinal permeability, sometimes referred to as “leaky gut,” which was measured by what occurs when inflammation, which interferes with the normal “tight junction” of the intestinal epithelium, allows large molecules to cross into the bloodstream. The investigators found that treating these mice with a probiotic (Bacteroides fragilis) led to a resolution of the leaky gut (the large molecules were no longer found in the blood); a restoration of normal intestinal flora; and a reduction in anxiety behaviors, communication abnormalities, and stereotypical behaviors. Even more fascinating, the authors then injected into normal mice one of the molecules that was markedly elevated in the blood when the mice had a leaky gut—a metabolite known as 4-ethylphenylsulfate (4-EPS). Mice injected with 4-EPS demonstrated anxiety-like behaviors similar to those seen in the mouse autism model. Although a mouse model clearly does not directly translate to humans, this elegant study provides support for the theory that the abnormal gastrointestinal function so commonly seen in children with autism [23] may contribute to or even cause some of the symptoms.
Conclusion
The use of CAM treatments for autism has been based upon the premise that there are physiological abnormalities in autism, and that if these can be corrected or improved, symptoms may also improve. This is sound reasoning, and some have suggested that the term CAM should be replaced by the term “biomedical” to reflect the underlying goal of treating abnormal biomedical function, as with pharmaceutical drugs. Physiological abnormalities have been shown to be present in autism, and preliminary evidence suggests that correcting them may produce important benefits. Whether one calls them CAM therapies or biomedical therapies, we support the further rigorous, evidence-based investigation of treatments that address physiological abnormalities. It is ethical for physicians to support families considering plausible CAM treatments after a thorough exploration and discussion of potential mechanisms of action, benefits and harms, safety, expense, and how use of these CAM treatments might compete for time and resources with other behavioral interventions. Clearly, we must be cautious not to prematurely recommend therapies that have no or limited evidence, but, when they are held to evidence-based standards, there’s really nothing all that “alternative” about CAM treatments.
References
-
Fombonne E. Past and future perspectives on autism epidemiology. In: Moldin SO, Rubenstein JLR, eds. Understanding Autism: From Basic Neuroscience to Treatment. Boca Raton, FL: CRC Press; 2006:25-48.
-
Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators; Centers for Disease Control and Prevention. Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR Surveill Summ.2014;63(2):1-21.
- Lai MC, Lombardo MV, Baron-Cohen S. Autism. Lancet. 2014;383(9920):896-910.
-
Ganz ML. The costs of autism. In: Moldin SO, Rubenstein JLR, eds. Understanding Autism: From Basic Neuroscience to Treatment. Boca Raton, FL: CRC Press; 2006:475-502.
- Howlin P, Magiati I, Charman T. Systematic review of early intensive behavioral interventions for children with autism. Am J Intellect Dev . 2009;114(1):23-41.
- Bent S, Hendren RL. Improving the prediction of response to therapy in autism. Neurotherapeutics. 2010;7(3):232-240.
- Hanson E, Kalish LA, Bunce E, et al. Use of complementary and alternative medicine among children diagnosed with autism spectrum disorder. J Autism Dev Disord. 2007;37(4):628-636.
- Harrington JW, Rosen L, Garnecho A, Patrick PA. Parental perceptions and use of complementary and alternative medicine practices for children with autistic spectrum disorders in private practice. J Dev Behav Pediatr. 2006;27(2 suppl):S156-S161.
- Wong HH, Smith RG. Patterns of complementary and alternative medical therapy use in children diagnosed with autism spectrum disorders. J Autism Dev Disord. 2006;36(7):901-909.
- Krishnaswami S, McPheeters ML, Veenstra-Vanderweele J. A systematic review of secretin for children with autism spectrum disorders. Pediatrics. 2011;127(5):e1322-e1325.
-
Sinha Y, Silove N, Williams K. Chelation therapy and autism. BMJ. 2006;333(7571):756.
- Rossignol DA, Frye RE. A review of research trends in physiological abnormalities in autism spectrum disorders: immune dysregulation, inflammation, oxidative stress, mitochondrial dysfunction and environmental toxicant exposures. Mol Psychiatry. 2012;17(4):389-401.
- Lofthouse N, Hendren R, Hurt E, Arnold LE, Butter E. A review of complementary and alternative treatments for autism spectrum disorders. Autism Res Treat. 2012;2012(870391):
- Chauhan A, Chauhan V, Brown WT, Cohen I. Oxidative stress in autism: increased lipid peroxidation and reduced serum levels of ceruloplasmin and transferrin—the antioxidant proteins. Life Sci. 2004;75(21):2539-2549.
- James SJ, Cutler P, Melnyk S, et al. Metabolic biomarkers of increased oxidative stress and impaired methylation capacity in children with autism. Am J Clin Nutr. 2004;80(6):1611-1617.
- Frye RE, Melnyk S, Fuchs G, et al. Effectiveness of methylcobalamin and folinic acid treatment on adaptive behavior in children with autistic disorder is related to glutathione redox status. Autism Res Treat. 2013;2013(609705):
- Zafarullah M, Li WQ, Sylvester J, Ahmad M. Molecular mechanisms of N-acetylcysteine actions. Cell Mol Life Sci. 2003;60(1):6-20.
- Hardan AY, Fung LK, Libove RA, et al. A randomized controlled pilot trial of oral N-acetylcysteine in children with autism. Biol Psychiatry. 2012;71(11):956-961.
- McCracken JT, McGough J, Shah B, et al. Research Units on Pediatric Psychopharmacology Autism Network. Risperidone in children with autism and serious behavioral problems. New Engl J Med. 2002;347(5):314-321.
- Owen R, Sikich L, Marcus RN, et al. Aripiprazole in the treatment of irritability in children and adolescents with autistic disorder. Pediatrics. 2009;124(6):1533-1540.
- Bertoglio K, James JS, Deprey L, Brule N, Hendren RL. Pilot study of the effect of methyl B12 treatment on behavioral and biomarker measures in children with autism. J Altern Complement Med. 2010;16(5):555-560.
- Hsiao EY, McBride SW, Hsien S, et al. Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell. 2013;155(7):1451-1463.
- McElhanon BO, McCracken C, Karpen S, Sharp WG. Gastrointestinal symptoms in autism spectrum disorder: a meta-analysis. Pediatrics. 2014;133(5):872-883.