The human papillomavirus (HPV) vaccine is unique among vaccines because it can prevent cancer. Yet vaccination rates remain low, and incidence of HPV infection remains high. A lack of education regarding the causal link between HPV infection and cancer and the purpose of the vaccine seems to be partially responsible, complicated by issues related to race, sex, sexual orientation, and public misperception.
Background
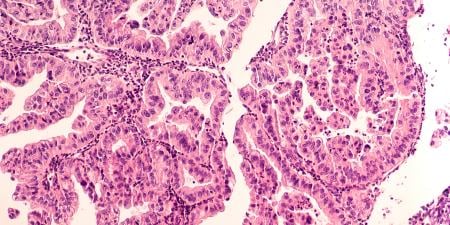
It is estimated that 14 million people acquire new HPV infections annually in the United States [1]. HPV is currently the most common sexually transmitted infection in our country [1-4], with the highest prevalence in sexually active adolescents and young adults [1-3]. There are more than 150 types of HPV, 40 of which infect the genitals [1, 5]. Most HPV infections, whether they carry a high or low risk for cervical cancer, are asymptomatic and resolve spontaneously within 1-2 years [1-3, 6-8]. HPV is considered to be a necessary cause of cervical cancer; infection with high-risk HPV types is found in 99 percent of all cervical cancers [6], and persistent infection with high-risk HPV types contributes to the development of cervical cancer [2, 3, 6, 8, 9], other anogenital cancers [2, 3, 9], and oropharyngeal cancers [1, 9]. However, infection with HPV is not sufficient to cause cervical cancer; many women are infected with HPV but do not go on to develop cancer [6]. It also usually takes decades for cervical cancer to develop after infection with HPV [6, 7]. The extant vaccines are recommended to be given starting at age 11-12, ideally before initiation of sexual activity [2, 3, 7-9, 10], because they do not seem to protect against disease from HPV types that patients are already infected with [6, 7, 10]. However, even if a patient is already sexually active, the vaccine should prevent the patient from being infected with other HPV types [7, 10].
Low Vaccination Rates
One of the main ethical and social questions surrounding HPV vaccination is low vaccination rates. The vaccination rates among adolescents and young adults, for whom the risk of infection is greatest, remain low [2, 4, 6, 11]—lower than was true for other vaccines in their first years of initiation [2, 6]. Some reasons that surveyed parents have cited for not vaccinating their children for HPV include needing more information, no recommendation of vaccination by a physician, and the perception that their daughters are not sexually active [11]. Other barriers to vaccination include low frequency of health maintenance visits, cost (if the vaccine is not covered or the patient is uninsured), and lack of understanding of disease risk [4]. Another possible contributor to low vaccination rates is concern that giving children the HPV vaccine will encourage sexual promiscuity [12]. Similar arguments have been made against discussing safe sex and making condoms accessible to adolescents. But, as clinicians, what we can and should do is educate and equip our patients to protect themselves from acquiring sexually transmitted diseases that could affect them for the rest of their lives. A theoretical risk that a patient will be somewhat more likely to engage in sex because he or she is more protected from adverse health consequences should not supersede a clinician’s duty to offer counseling, education, and interventions to prevent infection with preventable diseases. Parents and patients need to be educated on the burden of HPV infection and the benefits of vaccination.
It has been shown that physician recommendation is a major factor in vaccine initiation [9, 11]. Discussing HPV vaccination at every well-child check starting as early as age 9, but at the very least at ages 11 or 12, should help to increase acceptance of the vaccine and increase vaccination rates.
Recommendations and Utilization Rates by Subpopulation
A second issue surrounding the HPV vaccine is that, although it has been proven that HPV affects both men and women [5], recommendation and promotion of the vaccine for men has lagged behind approval and recommendations for women. While the most recent, nine-valent HPV vaccine was approved in December 2014 for use in both men and women [13], the two earlier vaccines were first approved only for women. When the first, quadrivalent HPV vaccine was licensed in 2006, it was only licensed for use in girls and women [7], and it was not until three years later that it was approved to prevent genital warts in boys and men [14]; a second HPV vaccine—the bivalent vaccine—was licensed in 2009 only for girls and women ages 10-25 [10]. One of the reasons for these discrepancies is that the vaccines have initially or only been studied in women. Clinical trials of the efficacy of the quadrivalent HPV vaccine in boys and men were still being conducted when the vaccine was first licensed for girls and women [3], and the bivalent vaccine has not been studied in men [8].
This lag may be due to the fact that questions remain about whether it is cost-effective to vaccinate boys and men against HPV. Mathematical modeling analyses seem to indicate that vaccination of men and boys is most cost-effective in populations in which the vaccination rate among women and girls is low [1, 14]. When the rate of vaccination is high among women and girls, the cost of vaccinating men and boys may outweigh the reduction of disease, since there should be sufficient herd immunity to protect men and boys from infection [1]. Herd immunity works both ways, however; men and boys can contribute to it, as well as reaping benefits for their own health [2, 15]. Practitioners thus should continue to recommend vaccination to everyone aged 11-26.
Disparities related to other demographic factors have also arisen. African American and Hispanic women have the highest rates of cervical cancer incidence and mortality [12], almost twice as high as the incidence and mortality rates among Caucasian women [16]. Additionally, African American and Hispanic adolescents are less likely than Caucasian adolescents to finish the HPV vaccine series [9, 11]. Men who have sex with men have a higher incidence of anal cancer than men who do not, and nearly all cases of anal cancer in this population are associated with HPV infection [7, 15]. Since the burden of disease from HPV is higher in these populations, it is important to provide education at every visit on the risks of HPV infection and the benefits of vaccination until the series is completed.
Moving Forward
Many great strides have been made to promote the HPV vaccine and incorporate it into the vaccine schedules for both sexes. Yet some stigma still surrounds the vaccine because HPV is primarily a sexually transmitted disease. One of the best ways to combat this stigma is by teaching that HPV infection has a well-established link to various cancers, that it is preventable, and that primary prevention is needed to reduce its incidence. We need to standardize acceptance of the HPV vaccine so that one day the cancers associated with HPV infection will be a distant memory.
References
-
Markowitz LE, Dunne EF, Saraiya M, et al; Centers for Disease Control and Prevention (CDC). Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP). Centers for Disease Control and Prevention. MMWR Recomm Rep. 2014;63(RR-05):1-30.
-
American Academy of Pediatrics Committee on Infectious Diseases. HPV vaccine recommendations. Pediatrics. 2012;129(3):602-605.
-
American Academy of Pediatrics Committee on Infectious Diseases. Prevention of human papillomavirus infection: provisional recommendations for immunization of girls and women with quadrivalent human papillomavirus vaccine. Pediatrics.2007;120(3):666-668.
- Hershey JH, Velez LF. Public health issues related to HPV vaccination. J Public Health Manag Pract. 2009;15(5):384-392.
- Bryan JT. Developing an HPV vaccine to prevent cervical cancer and genital warts. Vaccine. 2007;25(16):3001-3006.
-
Human papillomaviruses. In: Kimberlin DW, Brady MT, Jackson MA, Long SS, eds. Red Book: 2015 Report of the Committee on Infectious Diseases. 30th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2015:576-583.
- Markowitz LE, Dunne EF, Saraiya M, et al. Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2007;56(RR-2):1-24.
-
World Health Organization. Human papillomavirus vaccines: WHO position paper, October 2014. Wkly Epidemiol Rec. 2014;89(43):465-491.
- Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168(1):76-82.
-
Centers for Disease Control and Prevention (CDC). FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2010;59(20):626-629.
- Dorell CG, Yankey D, Santibanez TA, Markwitz LE. Human papillomavirus vaccination series initiation and completion, 2008-2009. Pediatrics. 2011;128(5):830-839.
- Downs LS Jr, Scarinci I, Einstein MH, Collins Y, Flowers L. Overcoming the barriers to HPV vaccination in high-risk populations in the US. Gynecol Oncol. 2010;117(3):486-490.
-
Petrosky E, Bocchini JA Jr, Hariri S, et al; Centers for Disease Control and Prevention (CDC). Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2015;64(11):300-304.
-
Centers for Disease Control and Prevention (CDC). FDA licensure of quadrivalent human papillomavirus vaccine (HPV4, Gardasil) for use in males and guidance from the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2010;59(20):630-632.
- Partridge JM, Koutsky LA. Genital human papillomavirus infection in men. Lancet Infect Dis. 2006;6(1):21-31.
- Perkins RB, Brogly SB, Adams WG, Freund KM. Correlates of human papillomavirus vaccination rates in low-income, minority adolescents: a multicenter study. J Women’s Health (Larchmt). 2012;21(8):813-820.