Abstract
Preferential treatment of patients whom we deem “very important” is a practice that is common in our health care system. The impact of this designation and the care that results is rarely studied or scrutinized. Although we assume that this type of treatment results in superior outcomes, this assumption can be wrong for a variety of reasons, which we discuss here. In addition to expressing unjust preferential treatment for some patients and not others, VIP medicine could compromise patient safety.
Case
Javier, the surgical pathology resident on duty, gets a call about a biopsy performed for a “VIP” patient who is an important hospital donor. A handwritten note from the department chair accompanies the specimen: “Take good care of Mr. Armstrong and make sure his biopsy gets read immediately.” The laboratory technician has already gone home, and Javier wonders why this biopsy should be handled more quickly than others. “All of the patients whose samples are in this lab want their results as soon as possible,” Javier reasons. “They’re all worried about their results. Why should I prioritize Mr. Armstrong’s sample?” He is, however, concerned about the personal and professional consequences of defying orders from the chair of his department. He feels pressured, and he wonders what to do.
Commentary
It is common practice to treat VIP patients differently from the time they enter the system until the day they are discharged. There are many ways in which status and privilege—most notably, the ability to pay—enter into the health care system and affect patients’ access to care [1]. Preferential treatment of VIPs can either be blatant, as in the case of celebrities or donors, or more insidious, as when members of the health care team are expected to treat other physicians or their family members preferentially [2-4]. When confronted with the care of a VIP patient, we, as clinicians, feel pressure to provide care that is seamless, hassle-free, and error-free. Although this is what we want for all of our patients, we believe that such care is impossible in our current system, and so we try to circumvent the problems that we know exist. In trying to rectify the inefficiencies and problems that we know about in treating VIPs, however, we might bypass standard protocols and create new problems with “work-arounds,” actually increasing potential for error and harm [5].
Care of the VIP Surgery Patient
VIP surgery patients might be celebrities, donors, or politicians. Alternatively, they might be neither famous nor wealthy; they can be our colleagues or their family members. There are numerous ways in which VIP patients might receive preferential treatment on a surgical service that affects the care provided in pathology. For example, surgery and pathology intersect in the area of frozen section diagnoses. Prioritization of VIP surgery patients, from whom specimens are obtained, can directly or indirectly lead to VIP demands on pathologists.
VIP patients’ surgeries can be scheduled more quickly, displacing other patients in a crowded operating room (OR) schedule—an aspect of VIP care that violates the principle of social justice and our sense of fairness. We accept that patient surgeries may be prioritized based on the acuity of medical condition or, for elective procedures, on a “first come, first served” basis, but VIP patient surgeries might be scheduled sooner simply on the basis of the patient’s status. This accommodation could easily delay surgery for a non-VIP patient who needs it more urgently, which could lead to long-term harm. For example, delaying surgery could increase the likelihood of spread for certain types of cancer. A systematic practice of prioritizing patients based on social status or other nonclinical characteristics effectively increases disparities in the quality of care patients receive and in their clinical outcomes.
Scheduling is not the only way that VIP patients are treated differently on surgical services. VIP patients in teaching hospitals might demand that attending physicians operate without the assistance of residents or fellows. This demand, if met, can disrupt the procedures and quality assurance practices in place for surgical care, since academic medical centers rely on trainees as surgical assistants, and most surgeries cannot be performed without their assistance in any setting. This deviation from routine practice could compromise safety and quality in ways not anticipated by the patient at the time of a request. Since trainees play a vital role in the delivery of health care in an academic setting, steps and procedures can be missed if they are asked not to participate.
Care of a VIP Pathology Patient
Preferential care of the surgical biopsy patient can similarly lead to requests for special treatment of samples obtained during the procedure. A surgeon might ask for a frozen section, a technique that is used to make a rapid, if preliminary, diagnosis, while the patient is still in the operating room. This technique is appropriate if biopsy results will change the course of the surgery. For instance, a lymph node dissection might be necessary for certain types of cancer, but it is not necessary for others. Instead of using the biopsy to guide further surgery, the surgeon of a VIP patient might use it solely to inform the family quickly of a diagnosis. This can be harmful; initial frozen section diagnoses may be inaccurate after being fully processed [6]. This discrepancy could lead to emotional distress on the part of the patient or the family.
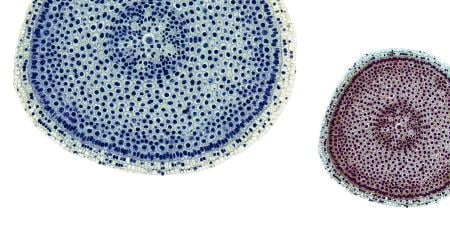
In addition to misuse of frozen section diagnosis, surgeons might ask that biopsy specimens be rushed just so that a diagnosis is available sooner. Under normal circumstances, a biopsy sample is obtained in the operating room, during the surgical procedure. It is placed in a fixative (formalin in most cases) and sent to be examined, described, cut, and placed in cassettes. These steps comprise what is known as “grossing the specimen.” On day two, after the sample has been processed and encased in paraffin, the histotechnologist cuts the paraffin block and makes glass slides, which are then delivered to pathology trainees (residents and fellows) in academic centers, who study them after having reviewed the patient’s history. On day three, the trainees present the case to the attending pathologist, and a final report is issued to the clinician who ordered the biopsy. In some cases, additional days could be needed for ancillary studies—special stains, immunohistochemical studies, fluorescence in situ hybridization studies, polymerase chain reaction assays—of the tissue. If complex testing is required, the results might not be available for 7 to 10 days or longer.
The desire to spare a VIP patient this typical waiting time for the biopsy results is understandable, but shortening the time could negatively affect processing and review of the samples and the diagnosis. For example, a suboptimal fixation of a specimen for morphologic examination could result in misdiagnosis. The typical workflow could be disrupted such that some technicians are involved in steps (e.g., grossing, preliminary histopathologic review) typically performed by others [7]. Or the time residents and fellows take to preview cases could be shortened, such that the relevant patient history might not be as thoroughly investigated as it would be when the trainees do not feel rushed. Even if an attending pathologist follows all of the steps that trainees usually perform for non-VIP patients, the case review could be missing an extra level of scrutiny by other members of the team. The attending pathologist might assume more primary responsibility for the preliminary diagnosis of a specimen and for ordering immunohistochemical and ancillary studies and might not follow the typical procedures, all of which could lead to actual delays in diagnosis. An attending pathologist might sidestep typical studies or processes in order to more quickly issue a report on a specimen; this could lead to inaccurate diagnosis and its harms. On the other hand, the stress of caring for a VIP and the fear of error could lead to unnecessary immunohistochemical stains and molecular tests that could result in more incidental findings or possibly even the wrong diagnosis.
Some of these same opportunities for error arise in situations in which a patient insists that an attending physician in internal medicine perform a procedure, such as a bone marrow biopsy, that she or he might not have performed in many years, or might not have performed using up-to-date techniques. Guzman and colleagues refer to this phenomenon as “chairperson’s syndrome” and urge hospitals to avoid assuming that VIP patients should be treated only by the most visible clinicians or senior attending physicians [8]. Excluding trainees might have negative consequences for VIP patients, especially when trainees are integral to the care of patients in our hospitals and, therefore, use their skills and knowledge of lab procedures more routinely than their faculty [9].
Professional and Institutional Factors Contributing to Preferential Treatment of VIPs
Medical hierarchy. In addition to ethical issues related to the care of VIPs, the case of Javier includes a situation in which the trainee does not feel comfortable doing what is asked of him by an attending physician. The organizational structure of medicine is rigidly hierarchical—especially in teaching hospitals where a team might consist of members at all levels of training, from medical students to attending physicians. Trainees often do not feel comfortable disagreeing with a plan set by an attending physician for many reasons [10], including lack of confidence, limited experience, and fear of retribution [10-13]. The trainee is in a vulnerable position since he or she relies on the attending physician for grades, promotion, or recommendation letters. Furthermore, attending physicians are not required to consider opinions of trainees, so if someone does have the courage to express an alternative view, his or her opinion might not, in the end, make any difference. For these reasons, trainees often “pick their battles” and acquiesce to requests that they perceive as misguided but not critically threatening to patient care quality, illegal, or unethical [10]. In the worst case, VIP pressures might induce trainees to accept instructions that truly are unethical, which can, in turn, produce moral distress and, possibly, patient harm. If situations that cause moral distress are repeated over the long term, trainees can develop moral desensitization (i.e., acceptance over time of what was once found morally unacceptable) and consequently view requests for special treatment of VIPs as a trivial exception to practice routines when they themselves rise in the hierarchy.
Residents’ acquiescence to attending physicians’ instructions with which they disagree can pose difficult problems, such as fear of retaliation or reprisals. Attending physicians might have not completely considered the ethical implications of VIP care or might have come to accept that it is condoned by the institution and, for the same reasons as those of their trainees, might not have questioned it with their own authority figures.
Hierarchy does not exist only between trainees and attending physicians. Attending physicians have similar concerns when it comes to requests from departmental chairs, hospital administrators, deans of medical schools, or hospital executives. Requests to give special treatment to a patient often come from the development or fundraising office and are sanctioned by hospital leadership, creating a culture in which an attending physician can feel powerless to say no to VIP requests and accept them as a normal part of practice.
Solicitation of donations. Most hospitals have development offices that seek contributions from wealthy donors [14-15]. Donors have a variety of personal or professional reasons for wishing to contribute to large academic or other medical centers; in some cases, they might be “grateful patients.” These people might be approached following medical care and asked to fund a particular physician’s research or to give to other areas relevant to their personal medical history. Although these fundraising practices are not inherently unethical, careful planning is required to ensure that privacy and confidentiality are not breached in finding and soliciting these patients [14]. The same concerns with VIP care also exist with this group of patients.
Recommendations
As in the case of Javier, it is difficult to resist prioritizing a VIP’s care on a case-by-case basis. Instead, institutions should actively discourage any systematic prioritization of VIP patients. Development offices should not facilitate scheduling or be allowed to interfere with policies and procedures that apply to patients served by an institution. Hospital administrators and executives might not understand the possible harms that assumptions or unspoken promises of preferential care can cause to a system already rife with disparities. In addition to the obvious concerns about fairness and justice, the increased risk of error, discussed earlier, might not be understood or anticipated by those not involved in the day-to-day care of patients. Patient education might also be needed so that donors and other VIPs do not have unrealistic expectations about access and care. For example, preoperative informed consent discussions could correct the misconception that residents are underqualified [16] or that rushing biopsy results is harmless. The fact that the hospital follows a standard procedure for planning medical care might inconvenience VIPs, but the rationale is compelling and could even be reassuring to a person requesting exceptional service [7, 17]. If the wait for lab results or other inconveniences are truly burdensome, attempts should be made to fix the problem for all patients.
If patients are celebrities or familiar political figures, reasonable attempts should be made to protect their privacy [4-5, 7]. However, expressions or endorsements of favoritism should not be tolerated by organizations or by professionals. It is difficult to resist pressure that members of a medical team might feel when treating a colleague or a colleague’s family member. The adaptations that might be required to favor a VIP patient can be a source of harm, so organizations and professionals should resist the temptation to capitulate to favoritism requests that prompt deviations from typical workflow. Practices and procedures that are efficient and motivate team-based quality performance should be followed to reduce both the potential for stress on the part of the professional and the potential for harm to the patient [2, 5, 9, 17, 18].
References
- Nesbitt S, Palomarez RE. Review: increasing awareness and education on health disparities for health care providers. Ethn Dis. 2016;26(2):181-190.
- Domeyer-Klenske A, Rosenbaum M. When doctor becomes patient: challenges and strategies in caring for physician-patients. Fam Med. 2012;44(7):471-477.
- Philips JB 3rd. Caring for other physicians. N Engl J Med. 1983;308(25):1542-1543.
- Schneck SA. “Doctoring” doctors and their families. JAMA. 1998;280(23):2039-2042.
- Alfandre D, Clever S, Farber NJ, Hughes MT, Redstone P, Lehmann LS. Caring for “very important patients”—ethical dilemmas and suggestions for practical management. Am J Med. 2016;129(2):143-147.
- Mahe E, Ara S, Bishara M, et al. Intraoperative pathology consultation: error, cause and impact. Can J Surg. 2013;56(3):E13-E18.
- Guzman JA, Sasidhar M, Stoller JK. Caring for VIPs: nine principles. Cleve Clin J Med. 2011;78(2):90-94.
-
Guzman, Sasidhar, Stoller, 92.
-
Mariano EC, McLeod JA. Emergency care for the VIP patient. In: Vincent JL, ed. Intensive Care Medicine: Annual Update 2007. Berlin, Germany: Springer-Verlag; 2007:969-975.
- Bould MD, Sutherland S, Sydor DT, Naik V, Friedman Z. Residents’ reluctance to challenge negative hierarchy in the operating room: a qualitative study. Can J Anaesth. 2015;62(6):576-586.
- Belyansky I, Martin TR, Prabhu AS, et al. Poor resident-attending intraoperative communication may compromise patient safety. J Surg Res. 2011;171(2):386-394.
-
Angoff NR, Duncan L, Roxas N, Hansen H. Power day: addressing the use and abuse of power in medical training [published online ahead of print March 15, 2016]. J Bioeth Inq. doi:10.1007/s11673-016-9714-4.
- Cassell EJ. Consent or obedience? Power and authority in medicine. N Engl J Med. 2005;352(4):328-330.
- Wright SM, Wolfe L, Stewart R, et al. Ethical concerns related to grateful patient philanthropy: the physician’s perspective. J Gen Intern Med. 2013;28(5):645-651.
-
Prokopetz JJ, Lehmann LS. Physicians as fundraisers: medical philanthropy and the doctor-patient relationship. PLoS Med. 2014;11(2):e1001600. http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1001600. Accessed April 29, 2016.
-
Ogunyemi B. Understanding the crucial role of resident doctors. HuffPost. February 8, 2016. http://www.huffingtonpost.ca/boluwaji-ogunyemi/resident-doctor-medicine_b_9260534.html. Accessed June 7, 2016.
- Smith MS, Shesser RF. The emergency care of the VIP patient. N Engl J Med. 1988;319(21):1421-1423.
- Walter JK. Practical and ethical implications of inpatient preferential treatment. Psychiatr Ann. 2012;42(1):30-32.