Abstract
Understanding the decline in the autopsy rate can be furthered through analysis of Foucault’s idea of the medical gaze and the ancient Greek idea of theoria. The medical gaze has shifted over time from the surface of the body to the inner organs to the cellular and subcellular levels. Physicians and loved ones of the deceased person are not likely to “gaze” at the same levels. Patients’ loved ones might not theorize as physicians do; they have different interests, which suggest the need for more attention to informed consent for autopsies. Responding to this need should take priority over efforts to increase the autopsy rate, and it can also be seen as an opportunity to improve autopsy and autopsy consent practices.
Introduction
The decline of the autopsy rate since 1972 is well documented [1]. Reasons offered include the 1971 decision of the Joint Commission on Accreditation of Hospitals (now the Joint Commission) to eliminate autopsy requirements for hospital accreditation, the high cost of autopsies, the cumbersome process required to obtain consent, and the belief that autopsies have lost their value because of advances in diagnostic testing [2].
Studies of autopsy results provide data that support the continuing importance of the autopsy, despite its decline. One study of autopsy results from 1960, 1970, and 1980 found that in all three decades, roughly 10 percent of autopsies revealed a previously undetected major diagnosis that, if known, might have led to a change in therapy that could have prolonged survival [3]. Another study comparing results of autopsies from a university hospital and a community hospital during 1984-1985 showed similar results and also discovered other “unexpected findings” that, had they been diagnosed premortem, probably would not have improved survival [4]. These findings suggest that the early ’80s marked an important shift: improved diagnostics rendered autopsies less necessary and less likely to reveal critical findings, which, if diagnosed earlier, could have made a difference for morbidity or mortality. A 2003 meta-analysis of 45 studies conducted over a period of 40 years showed statistically significant decreases over time in major diagnostic errors, although a major diagnosis remained clinically undetected in at least 8.4 percent of cases. The authors concluded that ongoing use of autopsy is warranted [5], but the evidence of a decrease in major diagnostic errors or an increase in the acuity of diagnostic technology suggests a less urgent need for autopsy than in the past.
Except in forensic cases, pathologists need permission from loved ones of the deceased person to do autopsies. But informed consent processes of discussing risks and benefits can be difficult for a deceased patient’s loved ones, who tend to “see” autopsies in a different light than pathologists. Reluctance to grant permission might be another reason for the decline in the autopsy rate. What can an understanding of habits of perception tell us about all this?
The Clinical Gaze
To understand just how differently pathologists and loved ones of the deceased person tend to view an autopsy, we first examine three aspects of the pathologist’s trained perception.
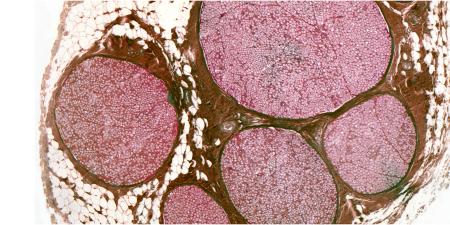
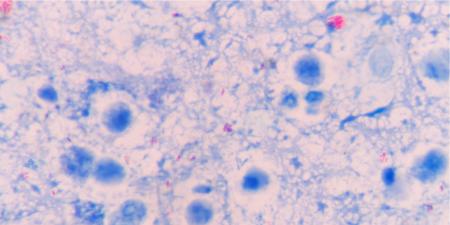
The “anatomo-clinical gaze.” Michel Foucault argued that in the late eighteenth century, with the “birth of the clinic,” the perceptual “gaze” of physicians shifted from the body’s surface to the inner organs, the space of pathological anatomy. Diseases, previously understood by classification of clinically observable symptoms and signs, were now seen as lesions in the depths of tissues. Understanding disease requires that we “open up a few corpses” [6]. Today, technology enables the gaze to focus on smaller histological, cytological, and molecular elements of organs. Through various forms of imaging and tests for pathology at the molecular level, bodies no longer need to be opened up to enable a gaze below the surface. Has technology rendered the methods of Virchow and Rokitansky, the pioneers of pathological anatomy, obsolete?
The technological gaze. Some have gone so far as to suggest that technology has fundamentally altered our perception of disease; Hofmann speaks of the “technological gaze,” perception mediated by technological means, in “The Technological Invention of Disease” [7]. That is, technology mediates between the perceiver and the perceived, allowing clinicians to observe representations of morbid anatomy during life. Pompilio and Viera argue that this new paradigm obviates the need for autopsies to correlate symptoms with pathological anatomy; instead, one need only check lab results and images, since these are what define disease [8]. Furthermore, this thinking is already reflected in the idea that “living anatomy” and medical imaging can replace the use of cadavers in anatomy teaching [9, 10]. It could be that a technological gaze is beginning to replace what Foucault called the “anatomo-clinical gaze,” which relied on opening a few corpses.
The theorizing gaze. The ancient Greeks’ theoria is the root of our word “theory.” Theoria was originally related to being a spectator. It meant the activity of looking at or considering, and it also referred to the spectacle that is viewed [11]. The common Latin translation, contemplatio, gives us the English “contemplation,” which carries quite lofty connotations for us and might lead us to miss the nuances buried in the Greek theoria. “Gazing upon” perhaps more aptly conveys the idea that theoria involves some depth. If we bring this notion of theoria as gaze to Foucault’s notion of the medical gaze, we see that the theorizing gaze not only looks more deeply into the body, but also contemplates more deeply what the body reveals.
In Book 10 of his Nicomachean Ethics, Aristotle calls a life of theoria the best, most fulfilling kind of human life [12], although he never fully explains exactly what he means by theoria. Philosopher David Roochnik argues that while some interpreters attribute to Aristotle an “exalted” conception of theoria—something akin to contemplating necessary truth—a more complex “mundane” conception seems correct when theoria is understood in the context of the whole of Aristotle’s writings [13]. Aristotle distinguishes between theoria (theorizing), praxis (rationally choosing a practical course of action), and poiesis (producing something). Praxis and poiesis are practical and involve objects that are shaped by human beings, but the object of theoria is truth itself. While the exalted conception of theoria draws a clear line between theorizing and the other two practical conceptions, Roochnik views Aristotle as linking these, as all purposeful human actions and productions involve an element of theorizing [13]. Purposeful and productive action is not merely instinctual, but involves depth of thought that seeks truth. This is a particularly apt understanding of the work of a pathologist, who delves into a patient’s body seeking not only knowledge of the disease of that particular person for practical, patient-centered reasons, but also knowledge of the truth about disease in general.
Although clinicians can have practical concerns such as explaining a death to a deceased person’s loved ones and improving care, they also have a theorizing gaze, as they are concerned with treating more than just this one patient and, like pathologists, want a better understanding of disease processes. When physicians request permission for an autopsy, they are seeking knowledge about various aspects of disease. The deceased patient’s loved ones, however, might have different practical, emotional, ethical, or spiritual concerns, such as expediting the return of the body to prepare for a wake. Their gaze can be affected by overwhelming emotions of grief and even fear, and the information to be gleaned from autopsy might hold relatively little importance for them.
A Patient’s Loved One’s Gaze
The objectifying technological gaze has undoubtedly rendered some families of deceased patients ambivalent about the need to “open up” and look deeply into a particular corpse. But their primary gaze likely remains at the surface, with fresh, raw images of the suffering of a loved one. Some may be altruistic about offering the body for educational purposes, but emotional resistance leads many to not even want to think about such a thing.
Those who have a technological gaze might see dead bodies, now lacking the essence of the person, as nothing more than nonfunctioning biological material. The medical gaze thus can focus on mechanical failure of organs, even if physicians recognize further practical purposes of autopsy such as diagnostic quality control and increasing knowledge that might benefit others. It is far more likely, however, that bereaved family members see the deceased patient’s body as a morally significant representation of the person. Memories of a person are based on memories associated with the body. Hence, loved ones of the deceased person can perceive the body as “at once dead and alive” [14] and focus on finding deeper meaning in that person’s death. The thought of cutting into the body and removing organs might be abhorrent to them—something that can easily escape the gaze of the pathologist going about everyday work. This dissonance alone cannot explain the decrease in autopsy rates; these feelings of abhorrence and resistance to thinking about death are nothing new. Such considerations, however, do suggest the importance of consent for, and robust discussion of the risks and benefits of, an autopsy.
Improving Informed Consent as a Means of Improving and Increasing Autopsies
What is needed is to de-emphasize getting permission for autopsies in order to enable the theorizing gaze, which can lead to knowing more about disease, and instead to emphasize getting informed consent. This recommendation might seem counterintuitive, but a frank discussion of the different gazes that are operative could lead to more carefully considered autopsies. Autopsy consent forms often lack information that would be helpful for both physicians and families in making educated decisions about autopsies. A national survey of autopsy consent practices found that over half of chief residents reported deficiencies in their knowledge of autopsy procedures [15]. If chief residents do not fully comprehend all the elements of an autopsy, they cannot explain them; it is hard to see how families could then give informed consent. What is needed is transparency in a conversation between physician and family and a robust discussion of risks and benefits [16]. Matters such as how the procedure is carried out, the retention of organs for teaching purposes, and the possibility of limited autopsies or postmortem use of imaging technology are examples of topics that should be discussed if consent is to be considered informed. Explicit discussion of all these matters manifests the respect due the body during autopsy.
Conclusion
Clinicians, pathologists, and families of a deceased person might gaze on the autopsy differently: families of the deceased might still see a person with whom they have had a significant relationship while clinicians and pathologists might have a more penetrating, objectifying, and theorizing gaze. Appreciating this difference in perception of value might help us to fulfill the ethical requirements of informed consent processes and the important roles autopsies can play in motivating our shared understandings of a person’s death. To be clear, the focus should not be primarily on increasing the number of autopsies performed, but rather on fostering cooperation between inquiring physicians and grieving families in order to uphold the value of seeking knowledge and to express respect for the deceased person’s body. In performing the autopsy, the pathologist, too, needs to direct a penetrating gaze in both of these directions.
References
-
Hoyert DL. The changing profile of autopsied deaths in the United States, 1972-2007. NCHS Data Brief. 2011;(67):1-8. http://www.cdc.gov/nchs/data/databriefs/db67.pdf. Accessed May 10, 2016.
-
Hoyert D. The autopsy, medicine, and mortality statistics. Vital Health Stat. 2001;3(32):1-42. http://www.cdc.gov/nchs/data/series/sr_03/sr03_032.pdf. Accessed April 29, 2016.
- Goldman L, Sayson R, Robbins S, Cohn LH, Bettmann M, Weisberg M. The value of the autopsy in three medical eras. N Engl J Med. 1983;308(17):1000-1005.
- Landefeld CS, Chren MM, Myers A, Geller R, Robbins S, Goldman L. Diagnostic yield of the autopsy in a university hospital and a community hospital. N Engl J Med. 1988;318(19):1249-1254.
- Shojania KG, Burton EC, McDonald KM, Goldman L. Changes in rates of autopsy-detected diagnostic errors over time: a systematic review. JAMA. 2003;289(21):2849-2856.
-
Foucault M. The Birth of the Clinic: An Archaeology of Medical Perception. Sheridan Smith AM, trans. New York, NY: Vintage Books; 1975:chap 8.
- Hofmann B. The technological invention of disease. Med Humanit. 2001;27(1):10-19.
- Pompilio CE, Vieira JE. The technological invention of disease and the decline of autopsies. Sao Paulo Med J. 2008;126(2):71-72.
- McLachlan JC. New path for teaching anatomy: living anatomy and medical imaging vs. dissection. Anat Rec B New Anat. 2004;281(1):4-5.
- McLachlan JC, Patten D. Anatomy teaching: ghosts of the past, present and future. Med Educ. 2006;40(3):243-253.
-
Liddell HG, Scott R, Jones HS. A Greek-English Lexicon: Revised Supplement. 9th ed. Oxford, UK: Clarendon Press; 1996.
-
Aristotle. Nicomachean Ethics. 2nd ed. Irwin T, trans. Indianapolis, IN: Hackett Publishing; 2000:10(7-8).
-
Roochnik D. What is theoria? Nicomachean Ethics book 10.7-8. Class Philol. 2009;104(1):69-82.
https://www.journals.uchicago.edu/doi/abs/10.1086/603572?journalCode=cp
-
Drayton J. Bodies-in-life/bodies-in-death: social work, coronial autopsies and the bonds of identity. Br J Soc Work. 2013;43(2):268.
- Rosenbaum GE, Burns J, Johnson J, Mitchell C, Robinson M, Truog RD. Autopsy consent practice at US teaching hospitals: results of a national survey. Arch Intern Med. 2000;160(3):374-380.
- Brody H. Transparency: informed consent in primary care. Hastings Cent Rep. 1989;19(5):5-9.