Abstract
Death certificates and autopsy reports contain personal identifying information and clinical information protected under the Health Insurance Portability and Accountability Act (HIPAA) of 1996. These documents are used, for example, by the families of the deceased for settling estates, bereavement and closure, and genetic counseling of relatives. Insurance companies, public health and law enforcement officials, and the legal community also have legitimate claims to this information. Critical ethical questions have not yet been settled about whether and when this information should be public and under which circumstances making this kind of information public incurs benefits, harms, or both. Additional considerations include which organizations—the media, academic institutions, or government agencies, for example—are best suited to interpret these questions and respond to them.
The Death of Prince
When superstar musician Prince died earlier this year, fans and media alike clamored for the results of his autopsy. Speculation swirled around the circumstances of his death and whether the medical examiner (ME) would release additional, detailed information. Like many states, Minnesota, where Prince both lived and died, restricts access to autopsy reports. So MEs are only allowed to release cause and manner of death and minimal identifying information [1]. After weeks of waiting for toxicology tests, Prince’s cause of death was leaked to the media by a law enforcement official, prompting the ME to release a one-page form identifying the official cause of death as an accidental overdose of fentanyl [2].
Media Interest in Autopsies and the Roles of Pathologists
When other stars, such as Michael Jackson and Whitney Houston, have died, the published autopsy results were quite detailed and painted a picture that allowed independent conclusions about their causes of death to be developed by both the media and fans [3, 4].
The issues of privacy, the role of government, transparency, and the so-called “public’s right to know” (asserted by the media for decades) have complicated the release of autopsy reports to the public. States have taken differing stances on whether and when to release autopsy reports, which gives rise to conflicting priorities among family members, public health and public safety officials, insurance companies, and other stakeholders. These issues have been the subject of ethical, legal, and clinical debate for many decades. As self-appointed “watchdogs” of the public interest, the media considers autopsy reports to be important sources of information. Yet federal law under the Health Insurance Portability and Accountability Act(HIPAA) of 1996 [5], with some exceptions, protects all individually identifiable health information—referred to as protected health information(PHI)—including information that “relates to the past, present, or future physical or mental health or condition of any individual [and] the provision of health care to any individual” that “is created or received by a health care provider, health plan, employer, or health care clearinghouse” [6].
Legally, ethically, and clinically relevant, however, is that MEs and coroners are not “covered entities” under HIPAA. To be clear, all MEs are forensic pathologists in appointed positions, while coroners are elected officials. State-to-state variations abound: sixteen states do not have laws requiring coroners to have specific training requirements, and four states require them to be physicians though not necessarily pathologists [7].
HIPAA, Professional Ethics, PHI, and the Public Domain
MEs and coroners are exempt from HIPAA when gathering information while executing their statutory responsibility to determine a cause of death, but a number of ethical questions remain about the extent of HIPAA’s authority to MEs’ and coroners’ practices. Should exemption from HIPAA extend to MEs and coroners when releasing information to the public? Was this exemption intended by the legislature to apply to MEs and coroners for the purpose of investigation only? Does this exemption mean that what would, in other circumstances, be considered PHI and thus not be releasable to the public, is somehow justifiably releasable to the public? If so, why?
In some states, an autopsy report is public record and a death certificate is restricted (e.g., Maryland [8]). In other states, the reverse is true (e.g., Virginia [9]): an autopsy report is restricted and a death certificate is not. So, effectively, in cases in which the deceased person is a public figure, a public record autopsy report (or death certificate, depending on the state) can become a “back door” to revealing restricted information, including PHI, in a death certificate (or autopsy report, depending on the state).
Conflict between promoting the ethical value of transparency by accelerating access to a public figure’s PHI and the right of that public figure to privacy, especially of PHI, is a significant dilemma that Prince’s case illustrates. Some persuaded by the so-called “public’s right to know” might argue that access to deceased patients’ (including public figures’) PHI should be exempt from HIPAA. Others might argue more generally that, since an autopsy is conducted after death, it should not be considered part of any patient’s clinical record. Others might argue, however, that an autopsy report contains clinical information that is PHI, regardless of the person’s renown or infamy, and thus should be—from legal, ethical, and clinical perspectives—regarded as private and protected as such by professionals.
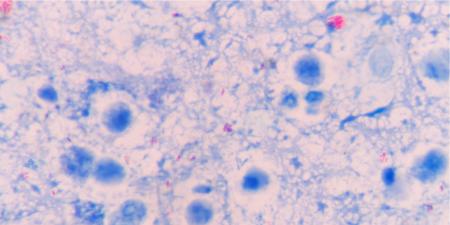
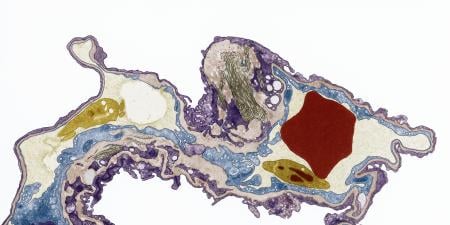
The National Association of Medical Examiners, for example, states that “the performance of forensic autopsy is the practice of medicine” [10]. This suggests that an autopsy report is probably regarded by most MEs as an important part of a person’s health record and perhaps as PHI. Like other health care professionals, pathologists are legally and ethically obliged to keep PHI confidential. Why should this professional obligation change when a pathologist is determining the cause of a person’s—any person’s—death?
More Unresolved Ethical Questions
It’s no wonder, then, that the demand for Prince’s full autopsy report has sparked numerous ethical questions about how state-by-state regulations and laws concerning autopsies should be interpreted. For example, in some states (e.g., Kentucky [11]), if a death is determined to be a coroner’s case, an ME or coroner has the authority to order an autopsy without obtaining consent from the deceased person’s survivors and to release information about the cause and manner of that person’s death to the public. Is this ethically appropriate, particularly considering the legal, ethical, and professional standards that typically apply to patients’ rights to have their PHI protected? Which protections should be afforded to the deceased and to a deceased person’s loved ones? How much value should be attributed to survivors’ distress? When, if ever, should a person’s status as a public figure matter for how we treat their PHI? What constitutes just access for the media, for example, to any person’s PHI? What constitutes appropriate scope of a so-called “right” to know, on the part of the public?
These questions will continue to be debated in the media and, most likely, in legislative bodies, for years to come.
References
-
Minn Stat chap sec 13.83. https://www.revisor.mn.gov/statutes/?id=13&view=chapter#stat.13.83. Accessed June 20, 2016.
-
Puente M. Prince died of “fentanyl toxicity,” an overdose of a painkiller. Record Searchlight. June 2, 2016. http://www.redding.com/news/381666051.xhtml. Accessed June 20, 2016.
-
Michael Jackson’s autopsy. Los Angeles Times. September 22, 2011. http://documents.latimes.com/michael-jackson-autopsy/. Accessed June 20, 2016.
-
Whitney Houston: final coroner’s report. Los Angeles Times. April 4, 2012. http://documents.latimes.com/whitney-houston-coroners-report-final/. Accessed June 20, 2016.
-
Health Insurance Portability and Accountability Act of 1996, Pub Law No. 104-191, 110 Stat 1936. https://www.gpo.gov/fdsys/pkg/PLAW-104publ191/html/PLAW-104publ191.htm. Accessed June 20, 2016.
-
HIPAA “protected health information”: what does PHI include? https://www.hipaa.com/hipaa-protected-health-information-what-does-phi-include/. Accessed June 21, 2016.
-
Centers for Disease Control and Prevention. Coroner training requirements. http://www.cdc.gov/phlp/publications/coroner/training.html. Updated January 1, 2015. Accessed June 22, 2016.
-
Maryland Department of Health and Mental Hygiene Office of Chief Medical Examiner. Frequently asked questions. http://dhmh.maryland.gov/ocme/Pages/faqs.aspx#cert. Accessed June 22, 2016.
-
Virginia Department of Health. Family and friends—frequently asked questions. https://www.vdh.virginia.gov/MedExam/FriendsFamilyFAQ.htm. Updated December 15, 2015. Accessed June 22, 2016.
-
Peterson GF, Clark SC. Forensic autopsy performance standards. National Association of Medical Examiners; October 16, 2006:4. https://www.mtf.org/pdf/name_standards_2006.pdf. Accessed June 20, 2016.
-
Kentucky Medical Examiner. Information for families. http://justice.ky.gov/Documents/Medical%20Examiners/KentuckyMedicalExaminerBrochure.pdf. Accessed June 22, 2016.