Abstract
This medical narrative highlights ways in which comics reflect the author’s experience as a primary care physician striving to offer sensitive care to people who have experienced sexual violence.
Comics in the Clinic
A few years ago, I started the PurpLE (Purpose: Listen and Engage) Clinic. Nested within a federally qualified health center network in New York City, the PurpLE Clinic provides longitudinal care for survivors of sexual violence and human rights-related abuses. The patients I work with have experienced human trafficking, domestic violence, sexual assault, and political violence. They come from the United States and abroad, are of all genders, are sometimes undocumented and uninsured, and face stressful social circumstances including homelessness and food insecurity. And all of them have experienced trauma.
As the sole physician at the PurpLE Clinic, my lens on “routine” primary care was necessarily, incrementally, adjusted and refocused to accommodate the breadth of violence and socioeconomic and medical circumstances impacting patients’ health. It became increasingly detached from the medicine that I had been taught and tested on in my training. Straightforward tasks such as: “use motivational interviewing to counsel on smoking cessation” would result in disclosures of “I smoke cigarettes to deal with the stress of my family being taken hostage back home. I’m not ready to quit,” which translates into the sterile electronic medical record verbiage of “tobacco cessation: precontemplative.” These unanticipated answers to routine questions became my new normal.
So I began creating cartoons to depict exactly this: a new normal. The opportunity to draw and share lessons learned, to advocate for underrepresented viewpoints, and to put forth clinical scenarios I struggle with ties me back to the clinical world of medicine that at times abandons me to algorithms and guidelines that are stubbornly inapplicable to the clinical scenarios I encounter.
Trauma-Informed Care Informed by Comics
Example 1. In the early days of the PurpLE clinic, a therapist contacted me to refer her client, Ms. X, for care. “I think it’s important for you to know that Ms. X is one of the most extreme cases of sex trafficking I have ever encountered,” she prepared me. It had taken two years of working together before Ms. X felt comfortable addressing the extensive traumas in her life with her therapist—multiple broken bones often misdiagnosed as fibromyalgia, psychological torture, and sexual violence. I had primed our staff that she would be arriving and would need particularly sensitive care. Anxiously looking at my schedule, I stepped into the waiting room to introduce myself when I saw that she had checked in. But I couldn’t find her. I peeked into each of the triage stations; our nurse was taking the vitals of a woman laughing with her child, and in the adjoining cubicle the medical assistant was offering an HIV test to an elderly man. But where was my patient? I grew concerned—was she in the bathroom? Had she left because she was too nervous? Running through a differential of possibilities for where she could be, I returned to the clinic room, and found the patient sitting there, waiting for me. And she was still laughing with her child. My misstep became clear as the encounter evolved. Ms. X continued smiling as we reviewed her medical history, but when her child stepped outside of the room her smile vanished, as she grasped the moment of privacy to share the symptoms of her mental and physical pain, her exhaustion manifesting as tears.
So why had I missed Ms. X in the triage area? I realized that I was trained to look for trauma, but I didn’t know how to look for resilience. I had assumed that Ms. X’s laughter precluded a history of pain. But she wore her smiles for her child. With each clinic, new functions of smiles emerged: a mask for shame, a vehicle for conveying disbelief of past experiences, a reflex when recounting happier times, and so on. Disconnecting smiling from assumed happiness relieved the cognitive dissonance I would experience after watching my non-English speaking patients smile while talking to an interpreter, only to hear back translations of graphic abuse perpetrated by traffickers or violent partners.
With the hope of being more in tune with the issues patients communicate to me, I have attempted to create a new normal, by training myself to stop assuming smiles are “one size fits all.” And to help others bypass my mistakes, I created this ever-evolving diagnostic chart for a smile.
Figure 1. The Smile Spectrum

In some medical scenarios, cultural norms not only lead us to misinterpret smiles but also teach us to expect smiles, which is equally problematic.
Example 2. The following scenario is not infrequent in the hallways of our safety net clinic.
Figure 2. Positive Test
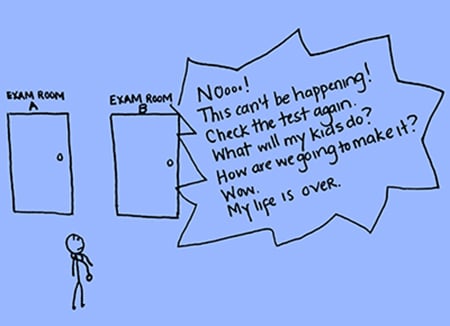
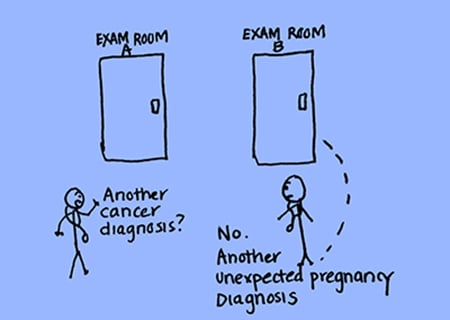
I was taught early in my family medicine training to unlearn the habit of saying “congratulations” when meeting a new patient who had a positive pregnancy test. As not all pregnancies are planned or desired, understanding the context of a pregnancy is essential in creating and preserving a patient-clinician partnership, especially when working with those experiencing abusive relationships.
This was indeed my experience with Ms. A. She was a new patient on my schedule, and all I knew was that “wants pregnancy test” was listed as the reason for her visit. So when I told her the test was positive, she smiled in relief—“Thank God! I was worried I was pregnant.” When I clarified the results with her, she screamed. It took me a few moments before I understood what had just occurred. “Positive” meant “positive news” for this mother of three with a six-month-old infant. Positive news meant not having an unplanned pregnancy following a recent sexual assault by her ex-husband. Positive news meant leaving the clinic with the same challenging circumstances she faced coming in, and nothing more. But instead, she found herself at a physician’s office, inconsolably blaming herself for becoming pregnant from a rape.
To counter a culture saturated with pregnancy test commercials equating happiness with a plus sign on a stick, I draw comics like this one to depict the complex, emotionally challenging scenarios that are also part of routine clinical care, with the hope of expanding our perceptions of “normal.”
Example 3. Even when pain and discomfort are anticipated during a clinic visit, they can present in unexpected ways. In our medical training, we are taught how to help patients feel more comfortable during gynecologic exams:
- “Encourage deep breaths.”
- “Use a smaller speculum.”
- “Add more lube.”
While these are helpful tips, I have found one area of discomfort during these exams that I did not receive guidance on managing: patient apologies.
Figure 3. “I’m Sorry, Doctor”
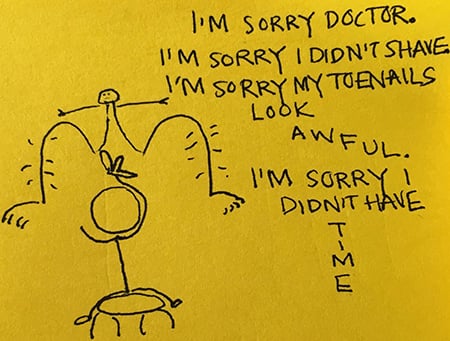
Unmanicured toenails or legs and pubic areas with hair commonly trigger a preemptive, “I’m sorry, Doctor,” from patients as soon as I reach for the speculum. These sentiments have been challenging for me to process—particularly when working with sexual trauma survivors who already express concerns that their appearance was a reason for their rape. When people share with me, “Now I try to dress in baggy clothes so people won’t harass me,” “I’ve stopped wearing make-up,” and “I gained weight because I didn’t want anything to do with my body anymore,” I do my best to listen, understand, and offer reassurance when appropriate.
But these revelations have also made me sensitive to the way that pelvic exams re-engage this complex relationship of physical appearance, violence, and shame. Women apologizing for their natural body hair and nails—essentially apologizing for being themselves—has caught me off guard and without a “gold standard” response to fill the void during these invasive exams. I find myself wishing I could refer to a clinical trial that studied the risks and benefits of responding to these apologies by saying nothing at all, reassuring the patient with an instructive “Please don’t apologize,” or, even better, trialing an affirming or empowering response. Until I come across that study, however, sharing these situations with friends and colleagues through comics helps spark conversation. And, to my surprise, common responses have included: “Yes! I always apologize to my doctor but I don’t know why” or “I never know how to respond either.” Such responses normalize the insecurity of both patient and physician in these scenarios as our profession seeks to find a best communication practice.
Reflections
Providing longitudinal care for people who have experienced sexual violence has changed my perception of normal medical practice. It has heightened my awareness of the versatility of facial expressions, the sensitivity of language, and the subtle ways in which culture, trauma, and health collide. Comics have become my vehicle for describing these flashpoints of learning: the moments inspired by a single influential patient encounter or the moments when repeated patterns finally come to consciousness. Depicting and sharing these moments through simple drawings protects the fragile strings that connect me to my patients and my profession.



