Abstract
Faith-based organizations serve as effective sites for community-based health promotion, but there is a lack of research on this work in ethnic minority-serving religious institutions such as mosques, temples, and gurdwaras. This article will share best practices, challenges, and special considerations in engaging these sites through two projects: Racial and Ethnic Approaches to Community Health for Asian Americans and Muslim Americans Reaching for Health and Building Alliances. We also discuss the Consolidated Framework for Implementation Research and how we used this framework in the two projects to facilitate implementation of health promotion initiatives within ethnic minority-serving religious institutions. To successfully implement such initiatives within these sites, efforts should leverage trusted internal and external relationships through iterative engagement, include adaptable interventions, and address sustainability from the outset.
Faith-Based Community Health
Faith-based organizations (FBOs) serve as effective sites for community-based health promotion activities, especially among underserved groups, given their roles as community centers.1-5 However, most research has focused on African-American and Latino community churches1,4; a limited number of studies have engaged other ethnic minority-serving religious institutions in the US, including mosques, temples, and gurudwaras.6-9 Results of the few studies that have conducted health promotion activities within these sites7,10-12 suggest that these sites are “prime opportunities”7for this work.
This paper will share best practices, challenges, and special considerations in engaging these religious settings in the US in health promotion programs and research through our experiences with two projects: Racial and Ethnic Approaches to Community Health for Asian Americans (REACH FAR) and Muslim Americans Reaching for Health and Building Alliances (MARHABA). Both projects were funded by the Centers for Disease Control and Prevention (CDC) and involved multiple community partners and sites (see table 1). Project foci were guided by the grant and funder priorities and specific disparities faced by the target communities. The REACH FAR project uses a community-engaged approach to implement and disseminate culturally adapted evidence-based policy, systems, and environmental strategies to improve hypertension prevention and management for Asian Americans (ie, Asian Indians, Bangladeshis, Filipinos, and Koreans) in New York City and New Jersey. The MARHABA project evaluates the effectiveness of a culturally adapted lay health worker (LHW) intervention designed to increase breast and cervical cancer screening among Muslim women using a randomized controlled design.
| Funding source | Partners and People |
|---|---|
|
REACH FAR |
|
| CDC (2014-2018) | 4 CBO partners: Korean Community Services of Metropolitan New York, Inc. (serving the Korean community in New York City); UNITED SIKHS (serving the Sikh community across the US); Diabetes Research, Education, and Action for Minorities (DREAM) Coalition (serving the Bangladeshi community in New York City); and Kalusugan Coalition (serving the Filipino community in New York City)
12 FBOs: 3 Asian Indian gurdwaras, 3 Bangladeshi mosques (including 1 senior center co-located in a mosque setting), 3 Korean churches, and 3 Filipino churches 9 KOT Consultants: Individuals identified by CBO partners to train volunteers on the KOT program in faith-based settings. Consultants were contracted and trained by the New York City Department of Health and Mental Hygiene on KOT program implementation 96 KOT volunteers: FBO volunteers and leaders identified in each setting to deliver the blood pressure screening program on a monthly basis to congregants |
|
MARHABA |
|
| CDC (2012-2014, 2015-2018) | 14 mosques and community centers: eg, Baitul Mamur Masjid, Al-Iman Masjid, Brooklyn Islamic Center, Jamaica Muslim Center, India Home, Turning Point
8 LHWs with networks and contacts in 5 New York City boroughs and South Asian, Southeast Asian, African American, African immigrant, and Middle Eastern Muslim communities |
| Abbreviations: CBO, community-based organization; CDC, Centers for Disease Control and Prevention; KOT, Keep on Track; FBOs, faith-based organizations; LHWs, lay health worker; MARHABA, Muslim Americans Reaching for Health and Building Alliances; REACH FAR, Racial and Ethnic Approaches to Community Health for Asian Americans. | |
Case Studies
REACH FAR. Building on a substantial collaborative history,11-17 the REACH FAR project is guided by a multisector coalition consisting of a lead academic agency (NYU School of Medicine); 4 community-based organizations (CBOs) representing the Asian-Indian, Bangladeshi, Filipino, and Korean communities; and New York and New Jersey state and local health departments.7 Aided by technical assistance, training, and resources from NYU School of Medicine, coalition partners leveraged their roots in the community to engage 12 FBO sites, including 6 churches in the Filipino and Korean communities, 3 gurdwaras (Sikh houses of worship) in the Asian-Indian community, and 3 mosques in the Bangladeshi community. Given the high burden of heart disease among Asian Americans18 and the lack of culturally tailored hypertension management programs for this population, the project implemented a multilevel, evidence-based health promotion and hypertension control program that addressed organizational change (increasing access to healthy foods and beverages at communal meals) and individual behavior change (improving cardiovascular health through the implementation of blood pressure [BP] screening programs).7
Specifically, organizational nutritional policies were implemented to improve access to heart-healthy food and beverages during communal meals in each of the 12 FBO settings. At each site, we conducted a baseline survey with congregants to assess availability of healthy foods and beverages during communal meals prior to policy implementation. Leadership was engaged to discuss opportunities for introducing healthy meal options, and a social marketing campaign was developed and implemented at each site to promote organizational policy change. The project enhanced and promoted systematic linkages to culturally and linguistically tailored community-based resources by implementing the Keep on Track (KOT) program—a volunteer-led BP monitoring program sponsored by the New York City Department of Health and Mental Hygiene—at FBO settings. At each site, trained consultants offered a train-the-trainer program to the FBO. Volunteers then held monthly BP screenings for congregants, and congregants who participated in the program received a free screening, culturally tailored health coaching, and referral to care if needed. FBO volunteers tracked and monitored congregant BP readings at each event. In a period of 36 months, REACH FAR activities reached 6 876 congregants across the 12 sites.
MARHABA. The MARHABA project is guided by a coalition of a lead academic agency (NYU School of Medicine), primary care practice clinicians, mosques, and CBOs.19 The project grew out of research suggesting that Muslim women in the US have lower rates of breast and cervical cancer screening compared to the general population.20 To address this disparity, the project implemented a culturally adapted LHW intervention designed to increase breast and cervical cancer screening among Muslim women in New York City. LHWs were identified leaders in the community and represented a variety of racial and ethnic backgrounds. Using their social networks and mosque affiliation, LHWs recruited Muslim women who were not up to date on their breast and cervical cancer screening to enroll in the intervention. Participants were randomized into a less intensive or more intensive intervention arm. Women in both groups received a 1-hour educational seminar delivered by an LHW and culturally and religiously adapted health education materials. Women in the more intensive intervention arm received additional follow-up from an LHW to schedule and obtain needed screenings. The study, started in December 2016 and currently ongoing, has linked 7 LHWs with 186 Muslim women across New York City, providing tailored health education and referral to screening, with a goal of reaching 370 women by September 2018.
A Framework for Successful Engagement and Implementation of Health-Promotion Initiatives in Religious Minority-Serving FBOs
Implementation science frameworks provide important domains and constructs for identifying barriers to addressing gaps in the translation of evidence into policies and programs, particularly policies and programs in minority-serving FBOs that might be otherwise left out of larger population health efforts. The Consolidated Framework for Implementation Research (CFIR)21 identifies key constructs in 5 domains that influence the implementation and dissemination process and that are relevant to working in minority-serving FBOs in particular. These domains comprise intervention characteristics (characteristics of the intervention itself), outer setting(factors external to the organization), inner setting (characteristics of the organization implementing the intervention), individual characteristics(characteristics of the persons involved in implementation), and process(the processes of implementation). The CFIR framework was an integral aspect of project development for REACH FAR and MARHABA; the 5 domains guided project planning, implementation, and sustainability.
Intervention characteristics. Two key factors related to intervention characteristics led to successful project implementation. First, we culturally adapted the intervention to increase its relevance and acceptability for our FBOs. For instance, within Sikh gurdwaras, we incorporated the concept of seva, or service to the community without personal benefit, into promotion of healthy food to serve during langar, or shared communal meals offered to gurdwara participants. Specifically, the concept of seva was incorporated in messaging on healthy food programming and in working with gurdwara leadership to facilitate initiation of the project. This cultural adaptation helped to enhance the relevance and resonance of healthy food promotion strategies for congregation members and leaders. In the MARHABA project, we integrated ideas of collectivism, commitment to God, and the importance of maintaining individual health for the greater family health into education materials. While the adapted nature of our intervention was crucial to implementation success, a challenge related to this approach is the ability to replicate activities across different sites, as the intervention often had to be adapted at multiple levels, including ethnicity, site, and language.
Outer setting. The CFIR framework assumes that the outer setting of environments where program or polices are implemented will influence the implementation process. In our studies, we found that FBOs that had a history of working with the project’s CBO partners were more likely to agree to project implementation because of the trust and shared history they had with the CBOs. In addition to leveraging formal partnerships with CBOs, leveraging external FBO networks was crucial to facilitate project success. For example, in the MARHABA study, we were able to leverage LHWs’ strong ties within both their congregation and their external social networks to rapidly recruit participants. Finally, we were able to facilitate FBO access to other external organizations and resources through our efforts. For instance, as part of the REACH FAR project, FBOs were incorporated in the New York City Department of Health and Mental Hygiene’s BP screening program network and connected with other health department initiatives, thus expanding the reach of citywide efforts for underserved populations. The outer setting of FBO settings engaged in our projects, however, also created barriers to implementation, particularly with regard to navigating the political and social context of the community. For example, mosques that were part of REACH FAR and MARHABA were often faced with competing challenges and priorities, as the New York City Muslim community has increasingly been a target of negative media attention and discriminatory practices in the last decade.22-24
Inner setting. We employed 3 strategies relevant to the inner setting domain to help us successfully implement our programs. First, we leveraged existing organizational infrastructure. All of the FBO sites we worked with had some type of volunteer committee structure, although the formality of structures varied across settings. For implementation of the KOT program, which is designed to be a volunteer-led screening program, we built upon existing structures within each FBO setting in the REACH FAR project and trained volunteers who were already active in FBO activities. Another factor that drove successful implementation was adaptation of the intervention to the organizational capacity of each site. For example, in working with FBO sites in the REACH FAR project to implement nutritional policy changes that would increase congregants’ access to healthy foods, we accounted for a variety of site structures—including sites with a kitchen that served their own food and those without a kitchen that received food from an outside source—in the policy language. Finally, we enhanced the internal capacity of each site by offering organizational incentives such as BP monitors and education materials. One specific challenge we encountered relevant to FBOs’ inner setting was variations in leadership structures; each site had its own leadership structure, such as volunteer committee structures at gurdwaras or imams and board structures at mosques. For this reason, gaining approval for project initiation at each FBO site varied substantially, as did the frequency and method of engagement.
Characteristics of individuals. Taking into account the characteristics and types of individuals implementing REACH FAR and MARHABA interventions was critical to success. For KOT volunteers in REACH FAR and LHWs in MARHABA, we recruited and trained individuals who had existing trusted relationships with congregation members, which enhanced program success. We also found it was important to engage opinion leaders in the implementation process and champions at each site to initiate and sustain the project. A challenge faced in implementation was the need to account for gender balance in certain FBO settings. For instance, mosques often separate faith-based activities in their sites by gender. As such, we had to ensure that we trained sufficient numbers of male and female volunteers for programs like KOT. Similarly, there were variations in sociodemographic factors such as access to care and English proficiency across sites. To overcome this challenge, it was crucial for us to engage multilingual volunteers and FBO leaders in REACH FAR and multilingual LHWs in MARHABA.
Process. We employed a number of process-related strategies to facilitate project implementation. For example, we utilized a combination of social marketing, congregant-level education, and organizational-level training to ensure project activities were mutually reinforcing in both MARHABA and REACH FAR. Site engagement also concurrently focused on various FBO representatives (eg, leadership, congregants, meal prep staff), and partnerships were formalized by codeveloping memorandums of understanding with each site. Finally, we also allowed for reflection and evaluation in the process by providing and soliciting feedback about the projects throughout the implementation process. Specifically, we disseminated brief reports on the impact of the activities to congregation and leadership, held community forums to update FBO sites on progress, and created structured opportunity to engage FBO leadership in the implementation process. Two related challenges relevant to the process were site leadership time constraints and our dependency on these leaders to implement programs. For instance, in order to implement projects at the gurdwaras, we needed approval from gurdwara committee members, who were often volunteers and only available on weekends. As such, decision making and the process of obtaining feedback on project implementation were often delayed.
Best Practices
Using the CFIR domains to guide project implementation, we have distilled a number of best practices for partnering with ethnic minority-serving FBOs on health promotion and prevention.
Leveraging trusted internal and external relationships through iterative engagement. We worked with community partners to identify FBOs for health promotion activities based on their shared histories. A history of collaboration between CBOs and FBOs enhanced the likelihood that sites would be amenable to implementing health promotion activities (eg, increasing healthier food and beverage options at communal meals) or providing access to such activities for congregation members (eg, allowing LHWs to host educational sessions and link women with screening services).
In addition to engaging external partners, engaging faith leaders, who are highly respected and serve as community gatekeepers, was critical. To this end, we developed guidelines to enhance faith leadership engagement. For example, a series of faith leader engagement meetings was conducted prior to implementation of health promotion activities at each site. Once faith leaders agreed to participate in projects, memorandums of understanding were jointly developed and reviewed by coalition partners and faith leaders. In addition to working with faith leadership, we worked closely with community members with informal leadership roles at the site. For instance, to ensure effective mechanisms for increasing access to healthy food at communal meals, the REACH FAR project engaged volunteers and people in charge of food procurement, preparation, and serving at FBO sites with kitchens as well as people in charge of purchasing food from outside vendors at sites without kitchens. Similarly, in order to ensure mosque participation in MARHABA, concurrently seeking approval from the imam as well as buy-in from female leaders at the mosque was important to project success.
Adaptation of intervention. Another best practice allows for the adaptation of protocols for health promotion program activities to address cultural and religious norms, the context of religious service and events, and FBO organizational structures. For example, REACH FAR BP screenings were adapted to accommodate Muslim women’s modesty concerns by creating a separate station for female congregants in mosques. Similarly, MARHABA breast and cervical cancer educational materials were adapted to address sociocultural considerations in obtaining screenings by including imagery of Muslim women. For instance, all clinicians in the materials are female and all female patients are shown with their head covered (see figure 1).
Figure. MARHABA Educational Materials

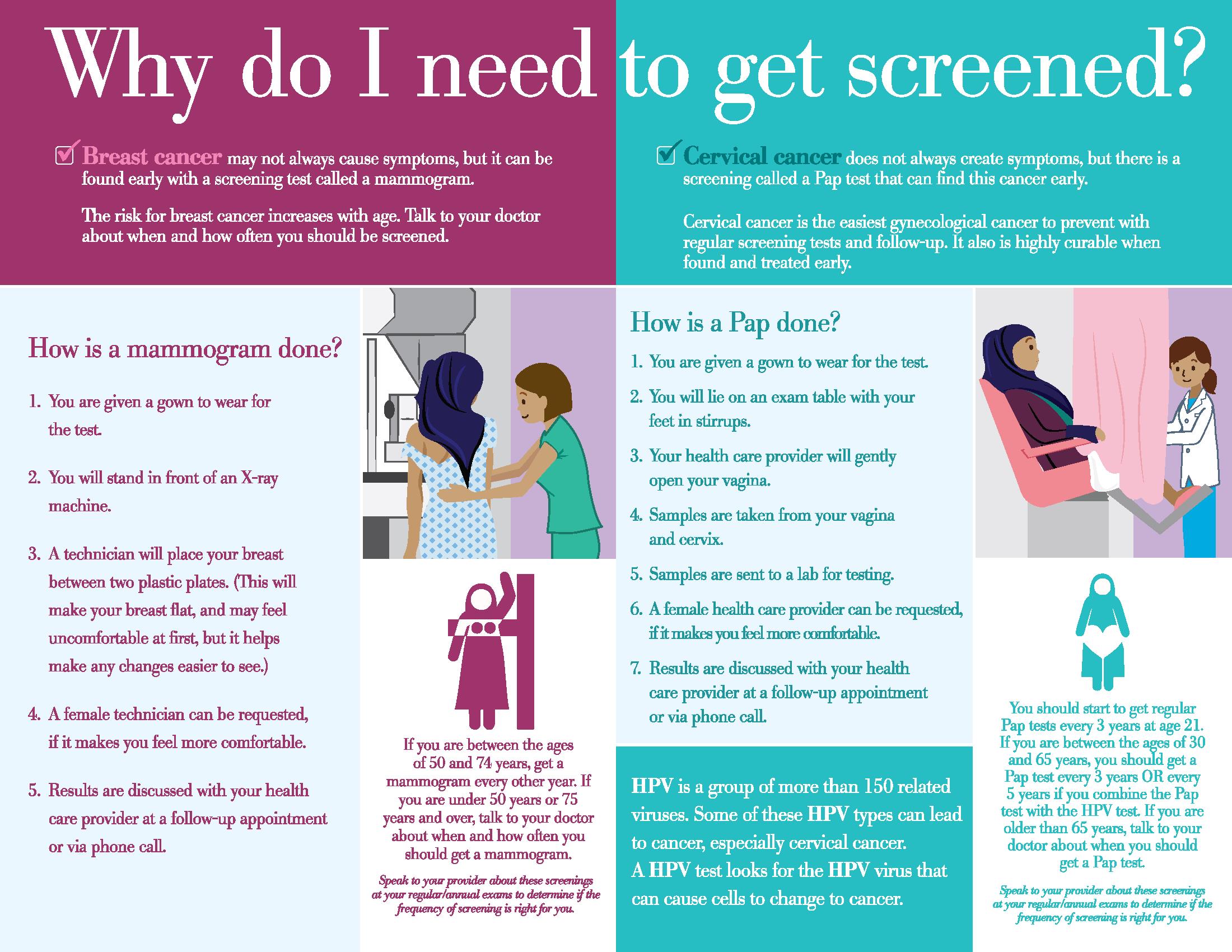
© Copyright Nadia Islam. Reproduced with permission of Nadia Islam.
To enhance project success, a variety of mutually reinforcing education activities and social marketing strategies were implemented at the sites. For instance, to implement REACH FAR activities at Korean churches, we first held a workshop on hypertension awareness and then held a healthy eating food sampling event at which congregants sampled low-sodium healthy recipes of traditional foods such as kimchi. In addition, staff displayed posters encouraging healthy eating at all events and provided nutrition education to congregants and kitchen staff.
Addressing sustainability from the outset. The organizational capacity of many minority-serving FBOs is at a nascent stage, although they serve large congregations. For example, leadership structures, though formalized, often shift in rapid cycles and might not be supported through salary or other means. Thus, the implementation of health promotion strategies should build organizational capacity. We accomplished this goal by tapping into natural leaders within each FBO (eg, individuals who led prayers groups or health screening events) and providing standardized and systemized training opportunities. Furthermore, we engaged these leaders in developing a protocol for health promotion programs that were realistic and sustainable within each FBO context. For instance, to increase access to healthy food and beverages at communal meals for the REACH FAR project, we offered a range of choices so that sites could choose the strategy that was the most feasible and relevant to their site and congregation. We also linked FBO settings and leaders to citywide resources and agencies that are otherwise disengaged from these settings to ensure continuance of the project. For example, REACH FAR sites were formalized into the local city health agency’s BP screening program network, which situated these sites for other opportunities and resources available through government agencies.
References
- Baskin ML, Resnicow K, Campbell MK. Conducting health interventions in black churches: a model for building effective partnerships. Ethn Dis. 2001;11(4):823-833.
-
Bond J, Wilson J, Eccles M, et al. Protocol for north of England and Scotland study of tonsillectomy and adeno-tonsillectomy in children (NESSTAC). A pragmatic randomised controlled trial comparing surgical intervention with conventional medical treatment in children with recurrent sore throats. BMC Ear Nose Throat Disord. 2006;6:13. doi:10.1186/1472-6815-6-13.
- Bopp M, Fallon EA. Health and wellness programming in faith-based organizations: a description of a nationwide sample. Health Promot Pract. 2013;14(1):122-131.
- Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28213-234.
- Peterson J, Atwood JR, Yates B. Key elements for church-based health promotion programs: outcome-based literature review. Public Health Nurs. 2002;19(6):401-411.
- Killawi A, Heisler M, Hamid H, Padela AI. Using CBPR for health research in American Muslim mosque communities. Prog Community Health Partnersh. 2015;9(1):65-74.
- Kwon SC, Patel S, Choy C, et al. Implementing health promotion activities using community-engaged approaches in Asian American faith-based organizations in New York City and New Jersey. Transl Behav Med. 2017;7(3):444-466.
- Nadimpalli SB, Van Devanter N, Kavathe R, Islam N. Developing and conducting a dissertation study through the community-based participatory research approach. Pedagogy Health Promot. 2016;2(2):94-100.
- Vu M, Muhammad H, Peek ME, Padela AI. Muslim women’s perspectives on designing mosque-based women’s health interventions—an exploratory qualitative study. Women Health. 2018;58(3):334-346.
- Banerjee AT, Landry M, Zawi M, et al. A pilot examination of a mosque-based physical activity intervention for South Asian Muslim women in Ontario, Canada. J Immigr Minor Health. 2017;19(2):349-357.
- Islam NS, Zanowiak JM, Wyatt LC, et al. Diabetes prevention in the New York City Sikh Asian Indian community: a pilot study. Int J Environ Res Public Health. 2014;11(5):5462-5486.
- Northridge ME, Kavathe R, Zanowiak J, Wyatt L, Singh H, Islam N. Implementation and dissemination of the Sikh American Families Oral Health Promotion Program. Transl Behav Med. 2017;7(3):435-443.
- Islam NS, Tandon D, Mukherji R, et al. Understanding barriers to and facilitators of diabetes control and prevention in the New York City Bangladeshi community: a mixed-methods approach. Am J Public Health. 2012;102(3):486-490.
- Islam NS, Wyatt LC, Patel SD, et al. Evaluation of a community health worker pilot intervention to improve diabetes management in Bangladeshi immigrants with type 2 diabetes in New York City. Diabetes Educ. 2013;39(4):478-493.
- Islam NS, Zanowiak JM, Wyatt LC, et al. A randomized-controlled, pilot intervention on diabetes prevention and healthy lifestyles in the New York City Korean community. J Community Health. 2013;38(6):1030-1041.
- Trinh-Shevrin C, Islam NS, Nadkarni SK, Park R, Kwon SC. Defining an integrative approach for health promotion and disease prevention: a population health equity framework. J Health Care Poor Underserved. 2015;26(2 suppl):146-163.
- Trinh-Shevrin C, Islam NS, Tandon SD, Abesamis N, Hoe-Asjoe H, Rey MJ. Using community-based participatory research as a guiding framework for health disparities research centers. Prog Community Health Partnersh. 2007;1(2):195-205.
- Jose PO, Frank AT, Kapphahn KI, et al. Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol. 2014;64(23):2486-2494.
-
Islam N, Patel S, Brooks-Griffin Q, et al. Understanding barriers and facilitators to breast and cervical cancer screening among Muslim women in New York City: perspectives from key informants. SM J Community Med. 2017;3(1):1022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5889113/. Accessed May 28, 2018.
- Salman KF. Health beliefs and practices related to cancer screening among Arab Muslim women in an urban community. Health Care Women Int. 2012;33(1):45-74.
-
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi:10.1186/1748-5908-4-50.
- Levin J, Idler EL. Islamophobia and the public health implications of religious hatred. Am J Public Health. 2018;108(6):718-719.
-
Pew Research Center. US Muslims Concerned about Their Place in Society, but Continue to Believe in the American Dream: Findings from Pew Research Center’s 2017 Survey of US Muslims.http://www.pewforum.org/2017/07/26/findings-from-pew-research-centers-2017-survey-of-us-muslims/2017. Published July 26, 2017. Accessed May 28, 2018.
- Samari G, Alcala HE, Sharif MZ. Islamophobia, health, and public health: a systematic literature review. Am J Public Health. 2018;108(6):e1-e9.