Abstract
The AMA Code of Medical Ethics offers guidance on ethical issues pertaining to risks involving patient discharge, which provides an example of how the Code might pertain to issues in risk management. This article presents one example case regarding patient discharge and how the Code might be applied in such a scenario to help guide physicians in ethically discharging a patient while also managing associated risks.
Introduction
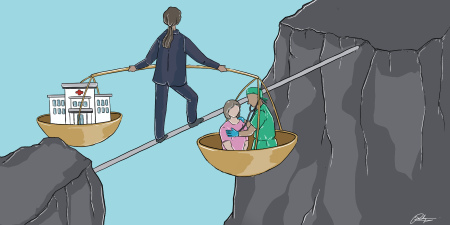
Risk management in health care “comprises the clinical and administrative systems, processes, and reports employed to detect, monitor, assess, mitigate, and prevent risks.”1 Health care risk management functions to both reactively and proactively “safeguard patient safety” while also helping to protect health care organizations’ value.1 The American Medical Association (AMA) Code of Medical Ethics does not speak specifically to the ethics of risk management; however, when the facts of a medical case involving risk management are considered, certain opinions of the Code become relevant and can provide guidance. One such example is a risk management case regarding patient discharge from a hospital. Here, the Code can guide physicians on how to address ethical issues that might arise when they plan a patient’s discharge. For example, discharge of patients with cognitive or physical disabilities often requires physicians to weigh ethical issues (eg, respect for patient autonomy, beneficence, nonmaleficence) against potential legal risks to the institution and to themselves.
Managing Risk During Discharge Planning
Case and Commentary 2 of this theme issue considers a 32-year-old man hospitalized with complications of end-stage multiple sclerosis who develops severe respiratory distress while in the intensive care unit. The patient repeatedly resists intubation through his body language, but his electronic health record (EHR) contains no advance directive. The pulmonologist believes the respiratory crisis is temporary and that remission is likely. She determines that the patient lacks decision-making capacity at this time and consults his parents. After obtaining their agreement, the medical team intubates the patient and begins mechanical ventilation. After 80 days, the patient’s condition stabilizes enough for him to be weaned from the ventilator. Soon afterward, the patient covers his tracheostomy tube and states, “I don’t want any more machines and I don’t want any more treatment. I want to go home, and I want to be by myself.”
The patient’s mother and sister agree to add orders to the EHR to limit future life-sustaining treatment. However, the patient’s father insists on implementing all resuscitative measures if his condition worsens again. The pulmonologist explains that the son “has decision-making capacity now, and he understands the risks of going home, so it’s reasonable for us to explore discharge planning at this time.” However, the father becomes angry and threatens to sue the physician and the hospital if something happens to his son. The care team consults the hospital’s risk manager, who advises that “[e]ven with full assessment of his home environment, his deteriorating condition makes anywhere he’s alone unsafe. Allowing him to exercise his right to self-determination is just too risky for us in this case.” The risk manager recommends that the patient be discharged to a skilled nursing facility. Members of the medical team wonder what to do next.
Relevant Code Opinions
There are several Code opinions that offer relevant guidance in this case. First, and most directly relevant, is Opinion 1.1.8, “Physician Responsibilities for Safe Patient Discharge,” which states: “Physicians’ primary ethical obligation to promote the well-being of individual patients encompasses an obligation to collaborate in a discharge plan that is safe for the patient” and “physicians should resist any discharge requests that are likely to compromise a patient’s safety.”2 In order to carry out this obligation to safely discharge, Opinion 1.1.8 states that physicians should:
(1) Determine that the patient is medically stable and ready for discharge from the treating facility; and
(2) Collaborate with those health care professionals and others who can facilitate a patient discharge to establish that a plan is in place for medically needed care that considers the patient’s particular needs and preferences.2
Applied to the case, the Code makes clear that the physician has a duty to ensure the patient’s safety when discharging and, in this case, that duty might require a plan that involves a safer option than home discharge—such as discharge to a skilled nursing facility—even though this option might be contrary to, and in tension with, the patient’s current wishes.
The physician has a duty to ensure the patient’s safety when discharging.
Also relevant are Code opinions regarding ascertaining and respecting a patient’s needs and preferences. Opinion 1.1.3, “Patient Rights,” states that “[a] patient who has decision-making capacity might accept or refuse any recommended medical intervention.”3 And Opinion 2.1.2, “Decisions for Adult Patients Who Lack Capacity,” advises that “[r]espect for patient autonomy is central to professional ethics and physicians should involve patients in health care decisions commensurate with the patient’s decision-making capacity” and that “[p]hysicians should engage patients whose capacity is impaired in decisions involving their own care to the greatest extent possible, including when the patient has previously designated a surrogate to make decisions on his or her behalf.”4 Applied to the case example, both opinions are key in that the patient had, at different points, capacity and a lack of capacity, and in both instances it is ethically important to understand and respect the desires of the patient—expressed either directly by the patient when he has capacity or by the patient’s surrogate when he lacks capacity—when making any medical decisions, such as about patient discharge.
Also relevant to patient autonomy regarding decisions about discharge is the Code’s discussion of ethically and emotionally challenging decisions regarding advance care planning. Opinion 5.1, “Advance Care Planning,” explains:
Planning in advance for decisions about care in the event of a life-threatening illness or injury gives individuals the opportunity to reflect on and express the values they want to have govern their care, to articulate the factors that are important to them for quality of life, and to make clear any preferences they have with respect to specific interventions.5
Opinion 5.1 makes clear that physicians should understand that “patients and families approach decision making in many different ways, informed by culture, faith traditions, and life experience, and should be sensitive to each patient’s individual situations and preferences when broaching discussion of planning for care at the end of life.”5 Advance care planning is acutely relevant to the case example, as the patient is at the end of life and planning the governance of his future care—including where and how he is discharged from the hospital—when it is critically important to uphold the patient’s autonomy and self-determination; thoughtful planning must reflect the patient’s goals. The Code recommends that physicians “encourage all patients” to consider “their values and perspectives on quality of life and articulate what goals they would have for care if they faced a life-threatening illness.”5 In the current case, such a dialogue with the patient about his goals and values would help him better ascertain whether discharge to a skilled nursing facility truly reflects his values, thus upholding his autonomy.
Lastly, the Code’s guidance on life-sustaining treatments has relevance for scenarios, as in the case example, in which patients resist discharge to a skilled nursing facility. Opinion 5.3, “Withholding or Withdrawing Life-Sustaining Treatment” reminds physicians that “a patient who has decision-making capacity appropriate to the decision at hand has the right to decline any medical intervention or ask that an intervention be stopped, even when that decision is expected to lead to his or her death and regardless of whether or not the individual is terminally ill,” and that “[p]hysicians should elicit patient goals of care and preferences regarding life-sustaining interventions early in the course of care, including the patient’s surrogate in that discussion whenever possible.”6 In the case example, the patient, when he regains capacity, decides to decline life-sustaining treatment. If, after the physician has elicited the patient’s goals and values and explained how nursing care might meet some of those goals, the patient still resists discharge to a skilled nursing facility, then the patient’s decision to decline life-sustaining treatment must be ethically respected, although it is in tension with the wishes of his father and increases the safety risks involved with hospital discharge. The physician must find a balance—possibly with the help of an ethics committee—that at some level respects the patient’s right to refuse life-sustaining treatment while also managing his discharge at an acceptable level of risk.
Conclusion
While the Code does not speak to risk management specifically, it certainly offers guidance regarding management of risk in the course of clinical care. In particular, the case example of patient discharge demonstrates the relevance of the Code to ethical issues of patient safety, patient autonomy (whether the patient has decision-making capacity), advance care planning, and the withholding or withdrawing of life-sustaining treatment. When physicians and hospital risk managers make decisions about discharging a patient, they must account not only for the risk assessment regarding discharge but also the ethical issues at hand. Tensions and disagreements—as in the case, where the patient wants to go home rather than to a skilled nursing facility—might be inevitable. If disagreement persists over the risks and benefits of a particular treatment or discharge plan, physicians should consult the hospital ethics committee and other institutional resources,2,4 which might be able to offer additional perspectives relevant to patient-centered care. This input could help support physicians in making ethically justifiable decisions regarding discharge that lower the risks of patient harm to acceptable levels.
References
-
What is risk management in healthcare? NEJM Catalyst. April 25, 2018. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0197. Accessed April 13, 2020.
-
American Medical Association. Opinion 1.1.8 Physician responsibilities for safe patient discharge. Code of Medical Ethics. https://www.ama-assn.org/delivering-care/ethics/physician-responsibilities-safe-patient-discharge. Accessed February 10, 2020.
-
American Medical Association. Opinion 1.1.3 Patient rights. Code of Medical Ethics. https://www.ama-assn.org/delivering-care/ethics/patient-rights. Accessed February 11, 2020.
-
American Medical Association. Opinion 2.1.2 Decisions for adult patients who lack capacity. Code of Medical Ethics. https://www.ama-assn.org/delivering-care/ethics/decisions-adult-patients-who-lack-capacity. Accessed February 10, 2020.
-
American Medical Association. Opinion 5.1 Advance care planning. Code of Medical Ethics. https://www.ama-assn.org/delivering-care/ethics/advance-care-planning. Accessed February 10, 2020.
-
American Medical Association. Opinion 5.3 Withholding or withdrawing life-sustaining treatment. Code of Medical Ethics. https://www.ama-assn.org/delivering-care/ethics/withholding-or-withdrawing-life-sustaining-treatment. Accessed February 10, 2020.