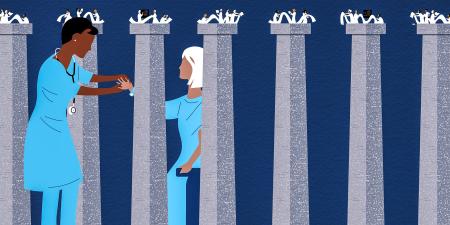
Whether oppressive structures are legal, financial, or educational, victims of systemic injustice have almost always been those with minoritized identities. Health care—despite clinicians’ presumed fiduciary obligations extending to patients and the public via the social contract—is not exempt from these flaws. Racism, policy- and practice-based assaults on reproductive rights, gun violence, disinformation, transphobia, mass incarceration, and climate change are features of contemporary medicine. To believe that biomedicine can remain above abuses of power and privilege is to be complicit in perpetuation of oppression in the US health sector.
The discourse of inequity in health care has been gaining momentum within health professions curricula over the past few years. Although well-intentioned, many of these curricula fail to build knowledge among learners about structural causes that have historically—and still currently—produce and reproduce inequity.1 Moreover, many of these teachings reinforce harmful stereotypes, fail to uproot bias, and fail to address how structural forces limit the autonomy of our most vulnerable patients and communities.1 Arbitrary “race corrections” to estimated glomerular filtration rates,2 poor access to obstetric care in rural areas and among women of color,3 and inferior health outcomes in historically redlined areas4 serve as few of the many examples of how a biomedical worldview of illness promotes racial essentialism while ignoring underlying institutional mechanisms that reify deeply historically entrenched patterns of oppression5,6—oppression that draws its legitimacy from decades of its unopposed existence.
Brazilian educational theorist Paulo Freire advocated critical pedagogy as a means of empowering people to effect societal change via critical consciousness (ie, awareness and questioning) of power and privilege.7 Incorporating such a pedagogy within health professions education (HPE) would require moving from the more traditional and checklist-driven competency approach to one that encourages deeper engagement with the structural determinants and social patterns of disease. By incorporating Freire’s pedagogy, faculty in HPE can empower learners to challenge the notions of biomedical essentialism that perpetuate injustices within health care. Critical pedagogies can equip learners to contextualize scientific phenomena within the contemporary sociopolitical realities of our times.
As editors of this theme issue on critical pedagogy, our goal is for this issue to serve as a tool kit for faculty who may find Freire’s principles too challenging and perhaps even too disruptive to incorporate in their existing curricula. The contributors to this issue apply diverse disciplinary lenses—including medical education, sociology, anthropology, educational psychology, and health policy—and represent the wider HPE community. Each piece highlights an important issue for health professions educators—curricular content, assessment strategies, educational scholarship, faculty development, virtual spaces, standardized patients, and more. In particular, the contributors examine how contemporary curricula promote racial essentialism, exacerbate inequity, and fail to appropriately problematize overly simplistic views of race in health and health care. In this issue, contributors contextualize the need for learners to engage with social determinants of health and provide key pedagogical ideas that can help faculty and scholars center criticality in their teaching, research, and scholarship.
References
- Tsai J, Crawford-Roberts A. A call for critical race theory in medical education. Acad Med. 2017;92(8):1072-1073.
- Richmond SP 2nd, Grubbs V. How abolition of race-based medicine is necessary to American health justice. AMA J Ethics. 2022;24(3):E226-E232.
-
Pandey P. A year after Dobbs: people with low incomes and communities of color disproportionately harmed. Center for Law and Social Policy blog. June 23, 2023. Accessed September 26, 2023. https://www.clasp.org/blog/a-year-after-dobbs-people-with-low-incomes-and-communities-of-color-disproportionately-harmed/
-
Lee EK, Donley G, Ciesielski TH, et al. Health outcomes in redlined versus non-redlined neighborhoods: a systematic review and meta-analysis. Soc Sci Med. 2022;294:114696.
- Cleveland Manchanda E, Sivashanker K, Kinglake S, Laflamme E, Saini V, Maybank A. Training to build antiracist, equitable health care systems. AMA J Ethics. 2023;25(1):E37-E47.
-
Tsai J, Lindo E, Bridges K. Seeing the window, finding the spider: applying critical race theory to medical education to make up where biomedical models and social determinants of health curricula fall short. Front Public Health. 2021;9:653643.
-
Freire P. Pedagogy of Hope: Reliving Pedagogy of the Oppressed. Barr RR, trans. Bloomsbury; 2021.