Case
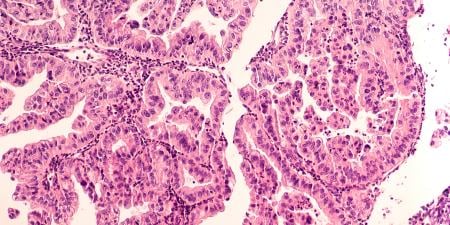
Mrs. Durham was diagnosed with an invasive epithelial ovarian cancer and, in conjunction with conversations about her treatment, was offered genetic testing for the BRCA1 and BRCA2 mutations. It was revealed that she carried a harmful BRCA1 mutation that is known to increase the lifetime risk of breast and ovarian cancer significantly. Once the results came back, her oncologist brought up the option of a prophylactic mastectomy and advised her to inform her living relatives of the results of the test.
Mrs. Durham’s primary care physician, Dr. Bartlett, expected she would do so, too. At her first appointment after the diagnosis, Dr. Bartlett asked Mrs. Durham how she was holding up and how her sister, Mrs. Weir—her only living family member and also one of Dr. Bartlett’s patients—had taken the news.
“Oh. Well, I haven’t told her.”
“Are you going to?” asked Dr. Bartlett.
Mrs. Durham responded, “You know we haven’t spoken in quite some time, and I can’t imagine making this the topic of our first conversation.”
“Yes, I know…but I think this is important information that may affect her health.”
Mrs. Durham sighed. “We’re estranged, for one thing, and for another, I want to keep my cancer private. I don’t want people knowing I’m sick and pitying me.”
Dr. Bartlett felt pulled in two directions—his obligation to respect Mrs. Durham’s wishes and protect her privacy conflicted with his obligation to promote Mrs. Weir’s health. BRCA1 mutations are not “reportable” illnesses like HIV and tuberculosis, so he was not compelled by law to break Mrs. Durham’s confidentiality. Dr. Bartlett considered how he might be able to encourage Mrs. Durham’s sister to be tested for the BRCA mutations while preserving Mrs. Durham’s confidentiality.
Commentary
In our case, Dr. Bartlett appears to have a professional obligation to keep Mrs. Durham’s private medical information confidential. He also appears to have an obligation to prevent harm to Mrs. Durham’s sister, Mrs. Weir, who is also his patient. Because her sister has the BRCA1 mutation, there is an increased likelihood of Mrs. Weir’s also carrying it, and, if she does, there is increased risk of harm from breast and ovarian cancer that could be reduced through prophylactic operations and aggressive screening. Therefore, Dr. Bartlett appears to have an obligation to counsel Mrs. Weir about her possible increased risk of cancer, about diagnostic testing that could verify whether she actually has this increased risk, and, if she does have the mutation and the concomitant increased risk of cancer that comes with it, about the therapeutic options available to her to decrease this risk.
On the face of it, it seems that Dr. Bartlett is confronted with an ethical dilemma. A true ethical dilemma involves competing moral obligations that cannot both be fulfilled and may take the following form: Person A has a moral obligation to do act X and act Y, but cannot do both X and Y simultaneously. In our case it seems that Dr. Bartlett must either protect Mrs. Durham’s confidentiality or break this confidence to try to decrease the risk of a bad outcome for her sister.
Whether one considers ethical dilemmas real depends on what ethical theory one accepts. Some ethical theories are structurally monistic, that is, they assert that any moral choice can, in theory, be adjudicated by one overarching moral rule and that what appears to be a dilemma is not. Act consequentialism is a theory that functions in this way [1]: the right action in any given case is that act which, among the possible acts an agent could pursue, would bring about the best balance of good over bad consequences—however one defines good or bad consequences.
Most approaches to moral decision making in modern bioethics, however, are not monistic. Rather, it is common in modern bioethics to assume a pluralistic framework—one in which multiple, competing moral claims do not simply reduce to an overarching moral claim [2, 3]. Unlike in monistic systems, in some pluralistic systems, moral dilemmas can arise [4].
In pluralistic systems, there are at least three different ways of thinking about conflicts between moral claims. First, one can take an optimistic view and hold that as long as one fulfills at least one of the competing moral obligations, one has acted rightly. So, as long as Dr. Bartlett either keeps Mrs. Durham’s information confidential or breaks confidentiality for the good reason of counseling her sister regarding her possible increased risk of cancer, he has done what is right. Alternatively, one can take a pessimistic view and hold that as long as one has failed to fulfill one of the competing moral obligations, one has acted wrongly. This would present a true ethical dilemma; regardless of whether Dr. Bartlett keeps Mrs. Durham’s medical information confidential or breaks confidentiality in order to counsel her sister, he has acted wrongly. However, there is a third way to think about conflicts between competing moral claims that does not assume each moral consideration to be an actual moral obligation.
In this third approach, individual moral considerations, each of which is considered to have some degree of moral force when viewed in isolation, are called prima facie moral obligations [5]. The job of the moral agent is to balance the competing prima facie moral obligations and come up with an all-things-considered (ATC) judgment about what to do in a given case. Prima facie obligations can be thought of as wrong-making or right-making properties. For example, the act “Dr. Bartlett divulges Mrs. Durham’s confidential information” can fall under different act descriptions. It can be described as an act of “breaking confidentiality,” and it can also be described as an act of “preventing harm.” Thus the same act has two moral properties—the wrong-making property of violating a prima facie obligation to maintain patient confidentiality and the right-making property of fulfilling a prima facie obligation to prevent harm.
The ATC judgment is an intuitive act of moral reasoning in which we consider all of the right- and wrong-making properties of the act and then judge whether the act is actually wrong, morally required, or permissible. It is this judgment that is ultimately action guiding, and it is these properties (i.e., wrongness or obligatoriness) that ultimately provide warrant for moral attitudes such as blame and praise. On this view, prima facie obligations are not actual obligations and, therefore, cannot lead to a true ethical dilemma. That is, taken individually, they do not necessarily obligate us. They are ways of describing the right- and wrong-making properties of acts that then must be weighed against one another to determine whether the act is actually morally required or prohibited. We may use the term obligation in prima facie obligations because if there is only one morally relevant description of an act, then the prima facie obligation exemplified by that act description would determine the rightness or wrongness of the act, which would then actually obligate us.
For our case, I will adopt this third approach, and our task will be to see which of the possible actions available to us is the right thing to do, given our prima facie obligation to keep Mrs. Durham’s private medical information confidential and our prima facie obligation to counsel Mrs. Weir in order to prevent possible harm.
Analysis of This Case
There are at least four different actions that Dr. Bartlett could take. First, he could simply not counsel Mrs. Weir regarding her possible increased risk of cancer. Second, he could break confidentiality, tell Mrs. Weir that Mrs. Durham tested positive for the BRCA1 mutation, counsel her regarding her own risk of carrying the mutation, and recommend getting tested. Third, he could try to convince Mrs. Durham to tell her sister about her positive BRCA1 test or, at least, to give him permission to do so. Finally, Dr. Bartlett could simply advise Mrs. Weir that he believes that she is at risk for the BRCA1 mutation and should get tested for it. If she asks why, then he could inform her that, while he is not at liberty to disclose all of the details of whyhe believes she is at increased risk, he has come to that conclusion and would like for her to trust that he is acting in her best interest.
I will argue against the first two approaches and for a combination of the last two approaches. The main ethical consideration that supports counseling Mrs. Weir to get tested is that physicians have a prima facieobligation to try to prevent disease from harming their patients. By not counseling Mrs. Weir about her possible increased risk of the BRCA1 mutation, Dr. Bartlett would be depriving her of information she needs to make a decision about tests and procedures that might help reduce her risk of cancer. However, if Dr. Bartlett simply told Mrs. Weir that Mrs. Durham had cancer and tested positive for the BRCA1 mutation, then he would be violating the competing prima facie obligation to keep Mrs. Durham’s medical information confidential.
Certainly, if Mrs. Durham told her sister herself or consented to allowing Dr. Bartlett to share this information with her sister, that would allow Dr. Bartlett to act in a way that did not violate patient confidentiality and would likewise allow him to fulfill his prima facie obligation to try to prevent harm to Mrs. Weir. It would be morally acceptable for Dr. Bartlett to have an open and honest discussion with Mrs. Durham about why he would want to share this information with her sister, offer a moral argument for why this would be appropriate, and make a direct recommendation such as, “I think you should allow me to share this information with your sister because it may help her make decisions that could decrease her risk of getting cancer.”
Let’s assume that, for whatever reason, Mrs. Durham again refuses. Whatever one may think about the moral propriety of her action, Dr. Bartlett would still have a prima facie moral obligation to keep her information confidential. One could argue that, since the obligation is only prima facie, it should be overridden by the prima facie obligation to try to prevent harm—especially if Mrs. Durham cannot articulate any good reasons for keeping the information confidential. However, in this case, I think that another option is available to Dr. Bartlett that would allow him to keep Mrs. Durham’s information confidential and prevent harm to Mrs. Weir. He could meet with Mrs. Weir and simply recommend that she get tested for the BRCA1 mutation. I could imagine the conversation going as follows:
Dr. Bartlett: Mrs. Weir, I wanted to bring you in today to discuss something with you. I have recently come to believe that you may be at increased risk of breast and ovarian cancer due to possibly possessing a genetic mutation. I would like to get you tested, because if you have this mutation there may be some things we can do to decrease your risk. The test involves obtaining a blood sample.
Mrs. Weir: Dr. Bartlett, why do you think I might have this mutation?
Dr. Bartlett: I am not at liberty to give you all the details of how I have come to believe that you might have this mutation, but I do think it is in your best interest if we had you tested. As your doctor I am asking you to trust me.
Trust is a ubiquitous part of the patient-physician relationship. And, while respect for patient autonomy is an extremely important ethical consideration that plays a fundamental role in the patient-physician relationship, respect for patient autonomy does not eliminate the need for patients to trust physicians, and it does not eliminate the need for physicians to be worthy of that trust. Sometimes trust is needed because the patient may not be able to understand or have enough time to process the information to make a decision without relying heavily on the physician’s recommendation. In this case, trust is needed because the physician is trying to avoid violating a prima facie obligation to one patient while also trying to meet his prima facieobligation to prevent harm to another patient.
At this point, one might object. What if Mrs. Weir surmises that her sister has the mutation and that this is why Dr. Bartlett wants to have her tested? Suppose Mrs. Weir asks Mrs. Durham if she has the mutation? I think that both are possible outcomes, but even if Mrs. Weir does come to the conclusion that her sister has the mutation, Dr. Bartlett has not violated Mrs. Durham’s confidentiality. He has not told Mrs. Weir anything about her sister’s condition. He has only used that information to help another one of his patients. And while I think a case can be made that Dr. Bartlett should not directly divulge or negligently expose Mrs. Durham’s personal health information to a third party, it is much harder to make the case that Dr. Bartlett should not use the information he has obtained to prevent a possible harm to a third party merely because doing so may increase the chances of that third party correctly surmising something about Mrs. Durham’s health condition.
Suppose, for example, a college student contracts meningitis in a dorm and doesn’t want anyone to know that she has it. Would the college student’s desire to keep her health information private also preclude someone’s sending letters to her dormmates about their need to get prophylaxis, because they might be able to deduce who was originally infected? I don’t think so. The point here is that when one patient’s confidential medical information can be used to prevent a serious harm to a third party, the prima facie right to confidentiality must be balanced against the prima facieobligation that the physician has to prevent serious harm to that third party. And while patients have a strong prima facie right to expect that physicians will not directly disclose or negligently expose their health information, the claim to a right that physicians do everything possible to prevent others from surmising on their own some detail about a patient’s health information is a far weaker claim. Suppose, for example, one patient sees another come to see an oncologist while in the waiting room and surmises that this person is being evaluated or treated for cancer. Are physicians obliged to prevent such occurrences? This seems to demand too much.
When divulging confidential information to prevent harm to a third party, I believe physicians should be guided by two principles. First, the harm should be both likely and significant [6]. The prima facie right to a physician’s confidentiality is strong—the patient-physician relationship depends on it—and it takes a strong counterclaim to override it. Second, the physician should divulge only the information necessary for the third party to avoid the possible harm. Divulging other information would break confidentiality for no good reason. In our case, the potential harm is great and the amount of information that needs to be divulged can be minimized to the point that there is no direct disclosure of any of Mrs. Durham’s confidential information.
In conclusion, Dr. Bartlett should talk to Mrs. Durham about why he believes it is important that her sister be tested and ask her to either tell her sister or allow him to discuss the positive BRCA1 test results with her sister. If Mrs. Durham refuses, Dr. Bartlett should reassure Mrs. Durham that he will not reveal to her sister that she has been diagnosed with ovarian cancer or with the BRCA1 mutation. He should then meet with Mrs. Weir, counsel her to get tested, and if she inquires why, inform her that he is not at liberty to say but would like for her to trust that he is trying to act in her best interest. This course of action would avoid violating Dr. Bartlett’s prima facie obligation to keep Mrs. Durham’s diagnosis confidential and fulfill his prima facieobligation to help prevent harm to Mrs. Weir.
References
-
For one famous version of act consequentialism, see Mill JS. Utilitarianism. Sher G, ed. Indianapolis, IN: Hackett Publishing Company; 1979.
-
Brody B. Life and Death Decision Making. New York, NY: Oxford University Press; 1988.
-
Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 6th ed. New York, NY: Oxford University Press; 2008.
-
For a useful summary of moral dilemmas, see McConnell T. Moral dilemmas. In: Zalta EN, ed. Stanford Encyclopedia of Philosophy. Revised June 30, 2014. http://plato.stanford.edu/archives/fall2014/entries/moral-dilemmas/. Accessed June 14, 2015.
-
For an example of this type of approach, see Ross WD. The Right and the Good. Indianapolis, IN: Hackett Publishing Company; 1988.
-
For a classic court case that has influenced thinking about breaking confidentiality to prevent harm to third parties, see Tarasoff v. Regents of the University of California. In: Beauchamp TL, Walters L, Kahn JP, Mastroianni AC, eds. Contemporary Issues in Bioethics. 7th ed. Belmont, CA: Thomson-Wadsworth; 2007:140-148.