Abstract
This first-person narrative illuminates how the author—a nurse, artist, and dancer—uses the arts and movement to help patients and clinicians process personal loss individually and collectively in the hospital setting. Through the arts, play, movement, and performance, the author raises awareness of and offers artistic practices to combat burnout, secondary traumatic stress, and moral injury. The author acknowledges that the stories of her patients have, in many ways, become her stories, and the reverse is true as well. These shared experiences remind us of the incredible impact that nurses have on patients—and patients, on nurses—every single day. Lastly, the author questions her understanding of resiliency and shares the ways the arts have helped her redefine its meaning.
Nurse as Patient
I have been a nurse for more than 19 years, and this was the first time I was a patient with a life-threatening experience in the hospital setting. I found myself alone, crying and waiting for a nurse to see me so I could get help. I knew this was one of those moments in life that I would never forget, a moment that would be with me and would change my life forever. I remember being admitted to the hospital with a tubal pregnancy and being transferred to a room when my fallopian tube burst. I remember my room being full of people, and though I was passed out, I could still hear everything that was being said. I remember my nurse grabbing my hand and telling me I was going to be okay, and I remember thanking her in my mind for remembering me because I was so scared, and I couldn’t speak.
After my experience as a patient, I was reminded of the incredible honor and gift it is to be a nurse, to care so intimately for patients who are scared, and to stand witness for and support others during some of life’s most difficult moments. As I reflected on the importance of creating this care with my patients so that they feel seen, heard, and truly cared for, I realized that the systems we work within do not readily allow for these connections to take place. Burnout, lack of support, secondary traumatic stress, moral injury, and many other factors in the nursing field contribute to inhibiting the experience of joy that can be found in a relationship as we care for another human being. In response, I founded The Clinic, an immersive theater company that creates artistic and play-based workshops and performances that take place in the hospital setting for clinicians, patients, and the general public to raise awareness of, reflect upon, and challenge inertia about burnout, secondary traumatic stress, and moral injury.
The Clinic
In October 2018, The Clinic premiered First, Do No Harm, an immersive theater performance open to clinicians and the general public that took place inside an active hospital. Through movement, art, music, and performance, First Do No Harm explored topics of grief, loss, compassion fatigue, and burnout from the perspective of nurses and patients’ family members. Guests, including clinicians and members of the general public, were taken through the hospital to different locations, where they witnessed firsthand through performance vignettes what nurses and family members go through on a daily basis. This performance helped clinicians give voice to the grief they were experiencing and contributed to destigmatizing and calling attention to the importance of clinicians prioritizing their mental and emotional well-being. It also offered members of the general public empathy-fostering understanding of the complex work clinicians perform in their profession.
I wonder now if the meaning of resiliency is to soften—to soften enough to feel and to find soft spaces of support to land.
Through the arts and play, The Clinic is shifting cultures, behaviors, and beliefs. Collectively, workshop participants get curious, move their bodies, share stories, and partner with artists, empowering them to reimagine new and healthy ways of being and thriving in the health care profession. The arts and artists are crucial for this exchange and for healing and disrupting old—and creating new—pathways forward for themselves and patients. When clinicians are seen, heard, and cared for, I believe patients will experience this caring as well.
Witnessing and Experiencing Grief Alongside Patients
I remember when I was working in the emergency room as the triage nurse. I had just returned from rooming a patient when a woman, crying, was wheeled into the triage bay. She was bleeding profusely, and she started screaming that she had lost her baby. As I wheeled her back into the emergency room, I saw a trail of blood behind us. When we arrived at her room, she was shaking, crying, and screaming. Her screams sounded like howls coming from the depth of her being. I hugged her as another nurse arrived to take over. As I walked back to the triage bay, tears formed in my eyes, as I could still feel the grief of this woman and hear her screaming for her child. In preparation to care for my next patient, I swallowed my tears. “You cannot cry.” I said to myself, “You must be strong, Tara.”
Only 2 days later, I see a trail of blood. I am losing my own baby, a baby I had just found out about earlier that morning. I remember this woman and how she held me as she cried and howled for her baby. I thought of how brave she was, and I chose in that moment not to swallow my tears but to allow myself to feel. This time I cried, screamed, and howled for her loss and for mine. I thanked her for teaching me that there’s power and strength in feeling our own emotions and that healing can come from allowing our tears to fall, as they play an important part in our experiencing sadness and the depths of our grief.
Singing in the Suffering
I remember when I heard her heart stop. It was 5:30 am and I was lying next to her in bed; all night I have been listening to her breath go in and out as the pauses between each breath got longer and longer until the next breath never came. I placed my ear to her heart and listened, but I heard nothing. This unconditional pulse of love that had been beating my whole life—the unconditional love that had been guiding me, nurturing me, caring for me—had suddenly stopped. I gathered my brother and sisters, and we held my mother and sang her favorite song, together holding hands as she left her body.
After the death of my mother, I felt as if I could not bounce back, I could no longer be resilient, I was tapped out, I was done. I could not be strong any longer, and the flow of my tears began and did not stop for the next 3 years as I earned my master’s degree in dance. Looking back, I wonder: Is this what resiliency really is? Up to this point, my definition of resiliency was to be strong—to bounce back quicker, harder, and stronger and be unchanged by my circumstances. I wonder now if the meaning of resiliency is to soften—to soften enough to feel and to find soft spaces of support to land. Softening also allows us a moment to slow down and reflect upon how self-care provides us an opportunity to see more clearly the injustices around us, which enables us to challenge harmful structures—including racism and other forms of discrimination—more effectively than someone who is burned out. It is in the softening, the plié, or the bending of our knees, that we are gathering the strength and support for ourselves to continue to grow.
COVID Stories and Resiliency Moments
Alongside our own stories, our patients’ stories can leave a lasting effect on us and, in some cases, even become part of our own story. In The Clinic, we create safe spaces where we can share these stories with one another and soften together, acknowledging the collective grief we carry in health care, and where we can create a mutual understanding that we are not alone in our suffering.
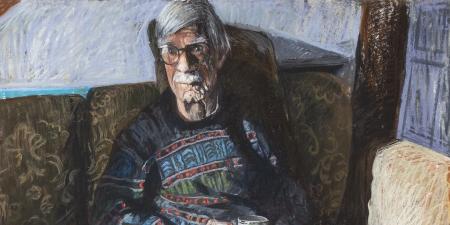
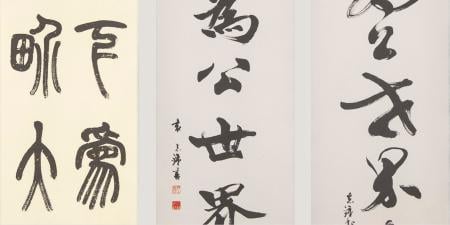
As COVID has ravaged an already-burned out profession, I have been honored to collectively create space for and access to the arts for health care professionals through our workshops, COVID Stories and Resiliency Moments. COVID Stories began during the pandemic and is a writing and movement series that offers time and space for nurses to journal and share their experiences during the COVID pandemic, both in person and virtually, through reading and responding to movement prompts with other nurses. Resiliency Moments is a virtual workshop that pairs health care professionals with musicians, dancers, and visual artists in one-on-one artistic experiences, offering health care professionals time to engage with artists through artistic prompts and offerings. Some participants receive a song that was created just for them, in the moment, based on personal preferences; others spend time in play and revisit memories of safe and calming spaces. In some cases, a visual art piece is created and mailed to the participant after the moment is over.
Listening to Ourselves
Together, as we navigate the unknown continuation of COVID, grief, burnout, and fatigue, I urge everyone to put their ears to their hearts and listen to their own pulse, their own beat, and their own longings—to take a moment to connect to others through the arts, movement, and play. Once we are in connection with what we need in order to be cared for and take the necessary steps to care for ourselves, I wonder: What would happen when we put our ears to the hearts of one another, hold one another’s hand, and collectively care for one another? I believe our hearts are urging us not to bounce back quickly from all we have experienced but to soften, to cry our tears, to listen, to slow down, to dance, to sing, to paint, to reflect, to grieve and, when ready, to use our soft landing, bend our knees, and wholeheartedly embrace the next leap that transpires.