Abstract
Genital reconstructive surgeries (GRS) are available for a variety of indications and populations, including transgender and gender diverse (TGD) individuals and those with intersex traits/differences in sex development (I/dsd). Despite the common outcomes of GRS for TGD and I/dsd individuals, decision making about this surgical care differs between these populations and across the lifespan. Sociocultural perspectives on sexuality and gender dominate the ethics of GRS, and reform is needed within clinical ethics to center the autonomy of TGD and I/dsd individuals in informed consent processes. Such changes are necessary to ensure justice in health care for all sex and gender diverse individuals across the lifespan.
Introduction
For transgender and gender diverse (TGD) individuals and for those with intersex traits/differences in sex development (I/dsd)—an umbrella term used to describe a constellation of congenital variations in sex traits—genital reconstructive surgeries (GRS) have analogous aesthetic and functional outcomes that contribute to sexual, gender, and reproductive health.1,2 Candidacy for GRS among sex and gender diverse populations has historically varied based on age. GRS for TGD populations is primarily accessible to adults, usually those who have reached the legal age of majority.1 In contrast, individuals with I/dsd are often considered for GRS in infancy and childhood.3 The ethics of decision making about GRS in these respective populations has evolved in parallel with clinical norms, such that considerations of beneficence and nonmaleficence in GRS—which are steeped in dominant societal notions of sexuality and gender—supersede considerations of respect for autonomy and justice.
After describing sociocultural norms of sexuality and gender, we examine historical and contemporary ethics of decision making about GRS that are influenced by these norms. Based on our collective history and extensive discussions with clinicians, community members, and advocates, we assert that GRS across the lifespan is ethically sound when the autonomy of sex and gender diverse individuals is centered in decision making and when these individuals are active participants in informed consent processes. We also identify and problematize divergent approaches to informed consent that do not consistently empower sex and gender diverse individuals as decision makers—either in adulthood or in adolescence, a period in the lifespan when both TGD individuals and those with I/dsd may seek GRS.
Influence of Sociocultural Norms on GRS
Sociocultural norms about sexuality and gender in the United States inform “standard” expectations for GRS procedures and associated surgical goals and outcomes. For example, people with 46 XX chromosomes who have virilizing congenital adrenal hyperplasia (CAH) are routinely considered for clitoral recession procedures because they have female sex organs (ovaries, uterus, and vagina) and gender identity (often reared from birth as female). Clinicians are less likely to expect that these patients will want metoidioplasty and urethral lengthening to create a more prominent phallus. It is assumed in these cases that societal norms and individual preferences will favor external genitalia typical of an endosex female (whose sexual traits are aligned with what is expected of “female” sexed bodies). We use the term endosex and explicitly name the majority category to avoid the implicit othering of minority individuals that occurs when framing minority status as being in opposition to “normal.”
Notably, there is some evidence that girls with virilizing CAH are more likely to identify as non-cisgender than girls without CAH and that some 46,XX CAH children may do well when raised male.4 As such, the threshold for parental consent for GRS to “correct” I/dsd variations—typically, for clitoroplasty in a child with CAH—is lower than the threshold for parental consent for GRS to affirm gender identity—eg, for metoidioplasty in an adolescent with CAH—because the former aligns with normative societal expectations, while the latter does not. As a result of such norms, TGD individuals across the lifespan also encounter clinicians who are hesitant or reticent to perform GRS when projected surgical outcomes do not aesthetically or functionally align with binary endosex standards. For example, vaginal sparing phalloplasty is a “nonstandard” GRS procedure that creates a phallus and preserves a functional vagina.
Historical and Medical Context for GRS
I/dsd populations. It is estimated that individuals with I/dsd compose up to 2% of the global population.5 GRS in individuals with I/dsd is medically indicated to treat or normalize genital aesthetic and functional variance.2 For example, urogenital sinus mobilization separates urethral and vaginal openings to achieve average, endosex female anatomical genital appearance and to promote future sexual and reproductive capacity, including tampon insertion, penile-vaginal intercourse with effective insemination, and the capacity for vaginal delivery.6 Originating in the 1930s, GRS for individuals with I/dsd made possible the alteration of infants’ genitals in order to align their gross anatomy and functionality with that of endosex individuals’ genitalia.7 Throughout the history of GRS for individuals with I/dsd, medical and ethics academies have endorsed—and clinicians have consistently upheld—guardians as the most appropriate decision makers regarding their children’s sexual, gender, and reproductive health.7 Prevailing ethical norms and legal standards continue to empower guardians to decide for or against infant or childhood GRS for individuals with I/dsd.
Since the 1990s, some individuals with I/dsd have shared lived experiences of early GRS as negatively affecting their sexual function and reproductive potential.8 These stakeholders have also voiced concerns about genital anatomical modifications in infancy or early childhood that could conflict with an individual’s future gender identity and embodiment goals.8 Their advocacy has invoked the principle of respect for autonomy and the right to an open future—the right of the child to self-determination, including the ability, upon achieving maturity, to make decisions about gender identity, sexual anatomy, and sexual and reproductive function—as guideposts of ethical decision making about GRS. Accordingly, clinicians and guardians in contemporary US health care settings have been called upon to postpone GRS until individuals with I/dsd can participate in informed consent processes.9 However, GRS in infancy and early childhood remains the standard of care for I/dsd populations at most US medical institutions.2
TGD populations. While global prevalence estimates are difficult to establish, TGD individuals compose around 0.6% of the US population, although the percentage is higher among adolescents (1.4%).10 Up to two-thirds of members of the TGD population in the United States may, during their lifetime, desire GRS to treat or relieve gender incongruence or dysphoria—distress arising from a mismatch between their gender and their sense of their physical, psychological, and emotional self.11 In its nascence, GRS for TGD individuals encompassed procedures common to GRS for individuals with I/dsd but the procedures were performed only on adults. Initial surgeries modified postpubertal genital anatomy according to aesthetic standards of endosex individuals of the “opposite” sex, and therefore surgical outcomes achieved select aspects of genital functionality per standards of heterosexuality.12 Despite differing medical indications, GRS in TGD and I/dsd populations shared similar periprocedural complications and postprocedural sequelae related to fertility and sexual function.1,3
Historically, TGD individuals received nominal direction from clinicians regarding medical interventions of relevance to their sexual, gender, and reproductive health and thus sought GRS at their own discretion.13,14 In contrast to candidacy for GRS for individuals with I/dsd, eligibility for GRS for TGD individuals was often contingent on presurgical psychological evaluations intended to assess TGD individuals’ readiness for GRS and to protect clinicians from ethical and legal scrutiny. This legacy reverberates in contemporary insurance and institutional requirements for GRS for TGD individuals in the United States.1,12,15 Notably, GRS is not widely accessible to TGD individuals in the United States before the legal age of majority, even with guardians’ consent.16 This age-related criterion for GRS reflects the international gold standard for TGD medical care set by the World Professional Association of Transgender Health (WPATH), which specified, until its most recent guidance update in 2022,17 that GRS should not be undertaken until the age of majority in any given country and, unlike with chest surgeries, WPATH did not provide alternate eligibility criteria for adolescents.1
Inconsistencies in Decision Making
Informed consent manifests the ethical principle of respect for an individual’s autonomy in decision making about medical care; upholds personal values of self-determination, sovereignty, authenticity, and best interest; and realizes intentional, collective, and relational decision making among individuals and other stakeholders.18 While clinicians are habitual stakeholders, guardians become stakeholders when individuals do not meet legal and clinical standards of competence and capacity. Importantly, in childhood and adolescence, guardians are stakeholders with legal authority to make decisions for the child,19,20 which is relevant to the ways in which decision making about GRS occurs for individuals with I/dsd.
I/dsd populations. Because GRS for individuals with I/dsd is most often performed in infancy and early childhood when the future preferences of individuals with I/dsd are unknowable, the locus of informed consent is the guardian. At this life stage, an individual with I/dsd’s assent is unobtainable. Neither legal competence nor decision-making capacity are present. As such, guardians rely upon their own values, those of clinicians, and the perceived values of society writ large to make a decision about GRS that they believe is in the best interest of the individual with I/dsd. In the context of clinical counseling, these stakeholders may be influenced by assumptions not associated with high-quality scientific evidence—specifically, the assumption that children with endosex genitalia will have better psychosocial outcomes than children with intersex genitalia in maturity.7 In addition, decisions about surgery may reflect culturally determined assumptions, including that a child with I/dsd will mature as heterosexual and desire aesthetically and functionally normative genitalia. Acceptance of a right to an open future prioritizes the as-yet-unknown values of an individual with I/dsd during childhood and can guide the guardian’s determination of the individual’s best interest regarding early GRS.19
TGD populations. In contrast to individuals with I/dsd, TGD individuals are central to decision making about GRS. Legal competence, as primarily defined by attainment of the legal age of majority, is ethically requisite. Consequently, informed consent for GRS most often occurs during adulthood, and the individual’s preferences and conception of quality of life are considered essential but insufficient for informed consent. Many clinicians and Global North societies view age as a proxy for psychological and cognitive maturity and dispute TGD adolescents’ ability to conceptualize their preferences about GRS.1,20,21 As such, societal obligation to the welfare of children is often considered to preclude GRS for TGD adolescents, even if they seek to assent and consent is given by their guardian(s). Importantly, many TGD adolescents have a strong sense of self-determination, authenticity, and their own best interest, although these values are rarely given substantive consideration or factored into professional guidelines concerning decision making about GRS for TGD adolescents.20
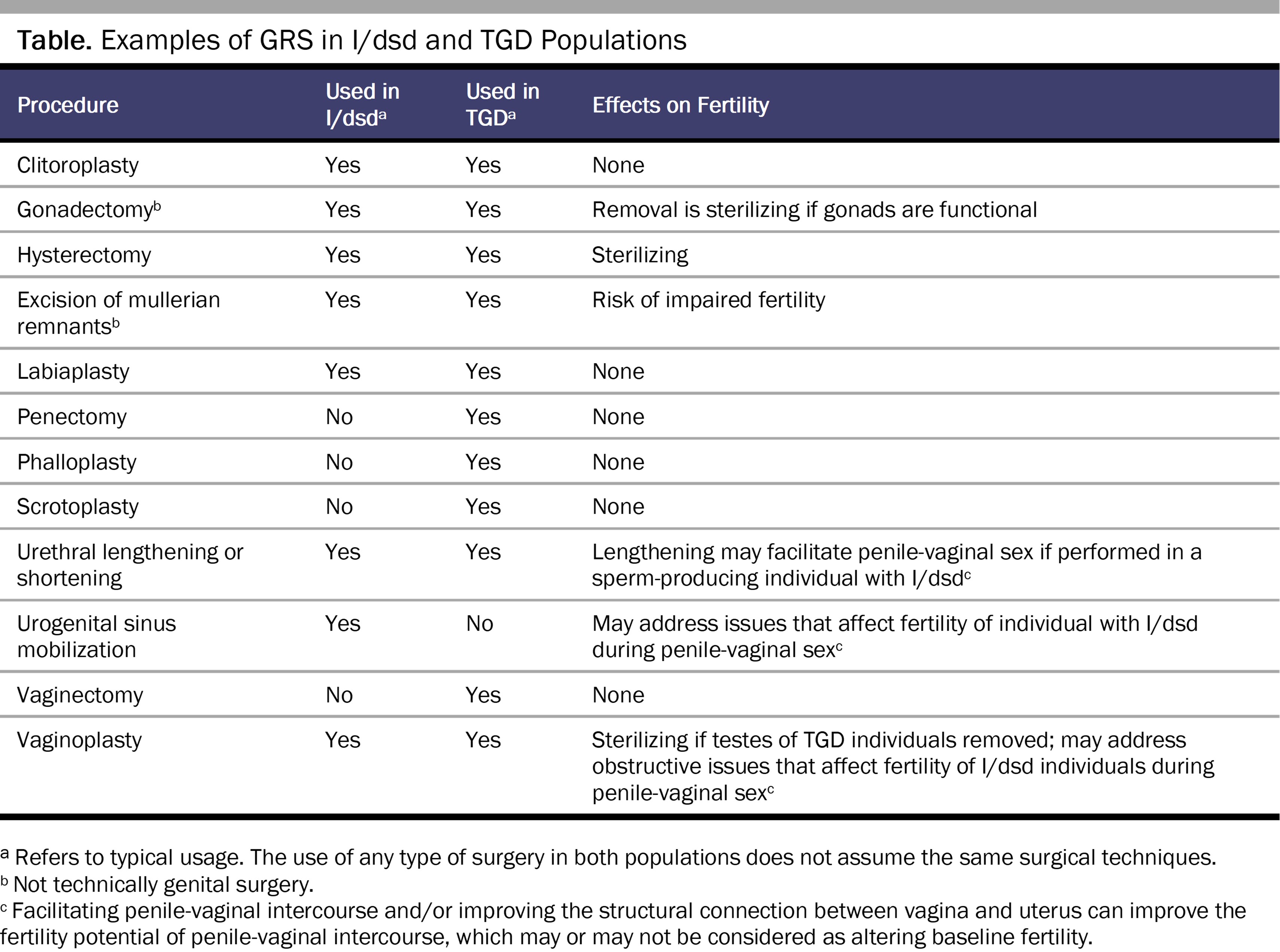
Despite the growing acceptance of gender diversity in Global North societies, ethical standards for decision making about GRS continue to incorporate the assumption that TGD individuals’ original genitalia are “normal” and “healthy” and to posit regret as a significant risk of surgery.17 Psychological evaluations are often required to corroborate an individual’s preferences and decision-making capacity, an insurance- and clinician-driven criterion that TGD and medical advocates identify as excessively restrictive and medically unnecessary.21 Desired genital alterations in GRS are diverse (see Table), and individuals whose preferences do not align with binary endosex norms can also experience regret if they do not undergo GRS.22
As of February 2023, 28 US state governments have introduced or passed legislation banning GRS and other gender-affirming care for TGD minors, even with guardian consent.23 In some states, this legislation subjects to criminal liability any clinicians who provide GRS or guardians who consent to such care for TGD adolescents.23,24 While eliminating the rights of guardians of TGD adolescents to consent to GRS actively desired and sought by their minor offspring, these mandates often incorporate explicit GRS exemptions for guardians of I/dsd infants and children and tacit permission for gender-affirming care among cisgender adolescents, such as breast augmentation or gynecomastia repair, with guardian consent.25 Such laws and policies reify an “ethics of normativity” in decision making about GRS. They also empower state governments as an implicit stakeholder, one with autonomy disproportionate to that entrusted to individuals, clinicians, and guardians and that tends to enforce sexual and gender uniformity as defined by dominant Global North societies.7 An ethics of normativity undermines respect for autonomy and defines beneficence and nonmaleficence solely in terms of the expectations of these societies. This reality precludes ethically sound informed consent for GRS in adolescence.
Working With I/dsd and TGD Populations
We recommend reform of clinical ethics to prioritize the autonomy of TGD adolescents and those with I/dsd irrespective of dominant sociocultural expectations regarding GRS. We propose the following key considerations to guide decision making and practice:
- GRS must be considered within an ethical context that understands sex and gender diversity to be normal, not pathological, states. Within such a decision-making framework, clinicians and other stakeholders champion the autonomy of TGD youth and those with I/dsd by emphasizing their self-determination, sovereignty, authenticity, and best interest. Ethically sound informed consent for GRS—especially concerning the rights of guardians to consent to these procedures for children and adolescents—warrants that the individuals who would be undergoing the procedure be considered active stakeholders and that their rights be given precedence when appropriate, based on their decisional capacity.
- The right to an open future must be prioritized in decision making about GRS for children and adolescents. Reproductive and sexual health are universal human rights.26 Decisions about fertility and sexuality are to be driven, to the extent possible, by the individuals that they most directly affect. Furthermore, all GRS must explicitly direct their primary benefit to the individual, as opposed to the guardian, the clinician, or other stakeholders.
- Assessment of adolescents’ decisional capacity using best practices is imperative to decision making about GRS for adolescents.27
Health care justice for TGD individuals and those with I/dsd requires explicit acknowledgment of dominant societal expectations so that they may be intentionally factored into decision making. Within this evolved ethics of GRS, justice is promoted by centering respect for the individual’s autonomy in decision making, seeing beneficence and nonmaleficence as principles that must derive from the locus of individual autonomy, and prioritizing the present and future rights of the individual over those of other implicit and explicit stakeholders.
References
- Coleman E, Bockting W, Botzer M, et al. Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, version 7. Int J Transgend. 2012;13(4):165-232.
- Lee PA, Nordenström A, Houk CP, et al. Global disorders of sex development update since 2006: perceptions, approach and care. Horm Res Paediatr. 2016;85(3):158-180.
- Lee PA, Houk CP, Ahmed SF, Hughes IA. Consensus statement on management of intersex disorders. Pediatrics. 2006;118(2):e488-e500.
- Pasterski V, Zucker KJ, Hindmarsh PC, et al. Increased cross-gender identification independent of gender role behavior in girls with congenital adrenal hyperplasia: results from a standardized assessment of 4- to 11-year-old children. Arch Sex Behav. 2015;44(5):1363-1375.
- Blackless M, Charuvastra A, Derryck A, Fausto‐Sterling A, Lauzanne K, Lee E. How sexually dimorphic are we? Review and synthesis. Am J Hum Biol. 2000;12(2):151-166.
- Jesus VM, Buriti F, Lessa R, Toralles MB, Oliveira LB, Barroso U. Total urogenital sinus mobilization for ambiguous genitalia. J Pediatr Surg. 2018;53(4):808-812.
-
Reis E. Bodies in Doubt: An American History of Intersex. Johns Hopkins University Press; 2012.
-
Karkazis K. Fixing Sex: Intersex, Medical Authority, and Lived Experience. Duke University Press; 2008.
- Sandberg DE, Vilain E. Decision making in differences of sex development/intersex care in the USA: bridging advocacy and family-centred care. Lancet Diabetes Endocrinol. 2022;10(6):381-383.
-
Herman JL, Flores AR, O’Neill KK. How Many Adults and Youth Identify as Transgender in the United States? UCLA School of Law; 2022. Accessed July 24, 2022. https://williamsinstitute.law.ucla.edu/publications/trans-adults-united-states/
-
James SE, Herman JL, Keisling M, Mottet L, Anafi M. The Report of the 2015 US Transgender Survey. National Center for Transgender Equality; 2016. Accessed April 18, 2023. https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf
-
Stryker S. Transgender History: The Roots of Today's Revolution. Seal Press; 2008.
- Willis P, Dobbs C, Evans E, Raithby M, Bishop JA. Reluctant educators and self-advocates: older trans adults’ experiences of health-care services and practitioners in seeking gender-affirming services. Health Expect. 2020;23(5):1231-1240.
-
Dawson R, Leong T. Not up for debate: LGBTQ people need and deserve tailored sexual and reproductive health care. Guttmacher Institute. November 16, 2020. Accessed July 24, 2022. https://www.guttmacher.org/article/2020/11/not-debate-lgbtq-people-need-and-deserve-tailored-sexual-and-reproductive-health
- Almazan AN, Benson TA, Boskey ER, Ganor O. Associations between transgender exclusion prohibitions and insurance coverage of gender-affirming surgery. LGBT Health. 2020;7(5):254-263.
- Milrod C, Karasic DH. Age is just a number: WPATH-affiliated surgeons’ experiences and attitudes toward vaginoplasty in transgender females under 18 years of age in the United States. J Sex Med. 2017;14(4):624-634.
- Coleman E, Radix AE, Bouman WP, et al. Standards of Care for the Health of Transgender and Gender Diverse People, version 8. Int J Transgend Health. 2022;23(suppl 1):S1-S259.
- Wendler D. Promoting the values for surrogate decision-making. JAMA. 2022;328(3):243-244.
- Bangalore Krishna K, Kogan BA, Mazur T, Hoebeke P, Bogaert G, Lee PA. Individualized care for patients with intersex (differences of sex development): part 4/5. Considering the ifs, whens, and whats regarding sexual-reproductive system surgery. J Pediatr Urol. 2021;17(3):338-345.
- Kimberly L, McBride Folkers K, Karrington B, Wernick J, Busa S, Salas-Humara C. Navigating evolving ethical questions in decision making for gender-affirming medical care for adolescents. J Clin Ethics. 2021;32(4):307-321.
- Cavanaugh T, Hopwood R, Lambert C. Informed consent in the medical care of transgender and gender-nonconforming patients. AMA J Ethics. 2016;18(11):1147-1155.
-
Hopwood RA. Supporting the transgender individual in deciding their pathway. In: Kauth MR, Shipherd JC, eds. Adult Transgender Care: An Interdisciplinary Approach for Training Mental Health Professionals. Routledge; 2018:61-77.
-
Goodwin GE. Utah just banned gender-affirming healthcare for transgender kids. These 21 other states are considering similar bills in 2023. Insider. February 1, 2023. Accessed February 23, 2023. https://www.insider.com/states-considering-bills-ban-gender-affirming-healthcare-transgender-youth-2023-1
-
Dawson L, Kates J. Youth access to gender-affirming care: the federal and state policy landscape. Kaiser Family Foundation. June 1, 2022. Accessed February 23, 2023. https://www.kff.org/other/issue-brief/youth-access-to-gender-affirming-care-the-federal-and-state-policy-landscape/
-
Outlawing trans youth: state legislatures and the battle over gender-affirming healthcare for minors. Harv Law Rev. 2021;134(6):2163-2185. Accessed February 23, 2023. https://harvardlawreview.org/wp-content/uploads/2021/04/134-Harv.-L.-Rev.-2163.pdf
-
Human Reproduction Programme. Sexual Health, Human Rights and the Law. World Health Organization; 2015. Accessed February 23, 2023. https://apps.who.int/iris/bitstream/handle/10665/175556/9789241564984_eng.pdf
- Baltag V, Takeuchi Y, Guthold R, Ambresin AE. Assessing and supporting adolescents’ capacity for autonomous decision-making in health-care settings: new guidance from the World Health Organization. J Adolesc Health. 2022;71(1):10-13.



