Abstract
This commentary examines the appropriateness of a clinician’s deceiving a patient who will not discuss lifesaving therapy through the lens of solidarity, a key professional ethical value. Clinicians’ awareness of social determinants of many patients’ increased vulnerability to HIV infection is needed to promote equitable HIV intervention outcomes at both individual and community levels.
Case
M is a 56-year-old Black man with human immunodeficiency virus (HIV) who is hospitalized with failure to thrive and dyspnea. Prior to hospitalization, M did not have an infectious disease or a primary care physician, and he was not taking antiretroviral therapy (ART). In the past 20 years, when physicians have tried to speak to M about his HIV diagnosis and benefits of ART, he has said, “I don’t have HIV,” or “I don’t talk about that.”
M has a CD4+ count of 3 cells/μL. He is diagnosed with Pneumocystis jirovecii pneumonia, norovirus diarrhea, and acquired immune deficiency syndrome (AIDS) wasting syndrome. During hospitalization, his relationships with clinicians worsen; if a clinician mentions HIV, M breaks eye contact, becomes silent, and interacts minimally.
An infectious disease specialist, Dr D, visits M to talk about his pneumonia. M consents to antibiotics to treat this infection and appears interested in strengthening his immune system “in other ways,” as Dr D suggests. Dr D continues to use M’s positive response as an opportunity to motivate M to take ART and is tempted to give M ART without saying it is HIV treatment. She is worried about deceiving M, taking unfair advantage of his lower health literacy, and upsetting him if he discovers that “immunity booster pills” are actually ART. Since low engagement with health care and worse health outcomes are prevalent in some communities of color and sometimes accompanied by misinformation about HIV, Dr D is encouraged by M’s engagement. She considers whether it might be best to get him to take ART, even unknowingly, to save his life.
Commentary
HIV disproportionately afflicts marginalized populations, but not through intrinsic biological susceptibility. Homophobia, drug use criminalization, inequitable access to HIV testing and treatment, and racism in sexual network formation contribute to HIV disparities.1,2 Clinician awareness of these and other social determinants of vulnerability to HIV infection is key to promoting equity in HIV outcomes. Combined with empathy, awareness of these factors can motivate education and testing in high-risk populations and focus funding and program development efforts in vulnerable communities.
Clinician Awareness
Awareness of patients’ social vulnerability to HIV infection can enable clinicians to have good conversations with individual patients about reducing their risk of infection.3 A clinician who knows that HIV infection prevalence is higher in populations with specific sexual behaviors, for example, can take a more complete sexual history of a specific patient, which can better position that clinician to help that patient reduce their risk of HIV infection or transmission. But awareness of a patient’s social vulnerability to HIV infection can also fuel discrimination and stigma.4 Men who have sex with men, people who inject drugs, and other groups with higher-than-average HIV infection risk are among those who experience discrimination from clinicians, which might affect HIV medication adherence or utilization of HIV primary care.4,5,6 Even well-meaning clinicians who would never intentionally discriminate might assume that demographics are the most important determinant of an individual patient’s risk. Clinicians who are aware that HIV infection prevalence is higher in patients from a given sociodemographic group might mistakenly infer, for example, more than they should about a specific patient’s mindset, behaviors, or risk profile on the basis of such demographics. If patients respond to this kind of error in reasoning by feeling stigmatized, they are likely to feel alienated from family and friends, employers, community leaders, and clinicians from whom they could seek help.7
Trust is central to therapeutic alliance and thus to the success of therapies like ART.
Clinicians also need to cultivate awareness that patients can respond to HIV stigma with reluctance to discussing either their risk behaviors or their infection status,8 perhaps out of fear of loss of employment, loss of insurance, suffering abuse, or being ostracized. Others respond to HIV stigma by internalizing it and might come to believe that they do not deserve care.9 Even patients who have unrestricted access to health care could, for instance, stop seeking health care if they expect a clinician to treat them poorly.10,11 In response to social or internalized stigma, people with HIV tend to develop coping mechanisms, including denial, which can exacerbate how they feel psychologically and physically. Indeed, HIV diagnosis has been associated with poorer self-reported health outcomes as well as lower engagement in care, including treatment refusal, in patients with HIV.12,13,14,15
Trust and Therapeutic Alliance
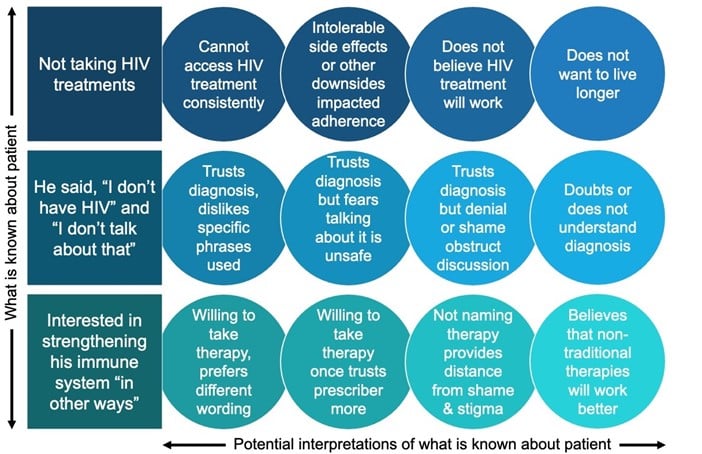
In the case, Dr D knows only 3 things with certainty about M and ART: M is not taking ART; M has been reluctant to discuss HIV infection, at least in certain ways; and M is open to “immunity booster pills,” whatever that might mean to him. It would be easy for Dr D to assume that M’s behaviors stem from low health literacy or mistrust. They might be. Dr D should not make this assumption, however. Instead, Dr D should gently explore an array of potential interpretations of these facts in a nonjudgmental conversation with M (see Figure). Approaching this conversation with respect and openness is more likely to build therapeutic alliance and yield a wider array of actionable hypotheses for Dr D than making unfounded assumptions about what motivates M’s behavior.
Figure. Potential Interpretations of Patient Statements Regarding Treatment for HIV Infection
Trust is central to therapeutic alliance and thus to the success of therapies like ART. Black and Latino patients in particular have suffered a legacy of institutional racism, unequal access to health care, and mistreatment at the hands of clinicians that long antedates the HIV epidemic, and perceived discrimination is related to mistrust in physicians.6,16 HIV-related stigma and clumsy clinician assumptions can simply confirm patients’ preexisting mistrust and thus lead to their further ostracism from high-quality care.
Avoiding stereotyping is key to establishing trust, particularly when clinicians and patients come from different demographic and socioeconomic backgrounds. On first meeting M, Dr D is seeing M as a person with AIDS and as a Black man. M is likely having similar perceptions of Dr D based on her speech, her dress, and the ways she reacts to him. In time, hopefully these first impressions will fall away and each will see the other as unique individuals, but this rarely happens during a first encounter. It takes time for clinicians to build trust with patients through listening, being open to questions, avoiding judgmental communications, and sharing both information and decision making with patients.17,18 A wise clinician balances a personal, individualized connection with the patient in front of her with awareness of complex dynamics, such as those discussed above.
Lying
Dr D fears for M’s life. It would be tempting to attempt to initiate ART and other potentially lifesaving therapies rapidly and by any means necessary. The temptation is understandable: M’s low CD4+ count and AIDS-defining illnesses do suggest his life expectancy might be measured in months.19 Temptations that arise from positive motivations, like the desire to save a life, can be the most difficult to resist. Dr D should, however, resist the temptation to lie. M is not likely to die today or this week. A lie today is not likely to save his life tomorrow and, in fact, it could have just the opposite effect. Even though a drug is prescribed through subterfuge, M is very likely to discover he is taking ART at some point. If this discovery makes M feel violated, M is unlikely to see Dr D again and may well be less likely to seek clinical care in the future. M’s adherence to ART will surely falter if he feels it was initiated under false pretenses. Deceit itself could thus be lethal, converting a misguided attempt at beneficence into an act of maleficence. Dr D should ensure that good, lifesaving intentions do not overshadow commitment to honest, transparent interactions with M. Deception is generally ethically and legally prohibited for the reasons above and because it expresses disrespect for patients’ dignity and autonomy. Hiding the nature of treatment from patients could prevent them from receiving care they want. Regardless of whether deception is regarded as legal in the face of HIV denial, most clinicians tend to understand deception as so unprofessional as to make its legality irrelevant.
Although outright deception thus runs afoul of more than one foundational value in bioethics, Dr D is not obligated to use a single set of words to describe ART, particularly if M might not understand or feel comfortable with her original word choice. Dr D is welcome to explore M’s level of health literacy and his vocabulary preferences and to probe gently to find a shared vocabulary for the medications she hopes will save his life. Perhaps M understands that Dr D wants to prescribe ART and is signaling with his reference to “other ways” of boosting his immune system that he is open to it. On the other hand, he may truly desire to avoid ART and be beset by a false belief that there is some other treatment that can prolong his life in a similar fashion.
Honesty
To identify patient knowledge gaps or attitudes that obstruct ART acceptance, Dr D can ask exploratory questions.
- What are M’s goals of care (eg, is longer life his goal)?
- Are there aspects of his health or HIV that M is willing to discuss?
- Are there words that M is comfortable using to address these topics?
- What does M understand about ART?
- Does M believe ART will prolong life?
- What does M mean by “other ways” of strengthening his immune system?
After probing M’s wishes, understanding, and preferences—and, in the process, building trust and a better sense of M’s needs—Dr D will be better positioned to offer ART adherence support via evidence-based interventions, including cognitive behavior therapy, education about the health benefits of ART adherence, treatment supporters, directly observed therapy, and dose reminders.20 Throughout these conversations, Dr D should always be clear that the treatment she is offering is treatment for HIV.
It is appropriate for concerned clinicians to want to initiate an urgently needed intervention, such as ART for M. This impulse, however, should never overshadow one’s obligation to be honest or distract from focus on therapeutic alliance and trust. With the same avidity with which she seeks ways to prescribe lifesaving ART for M, Dr D should find ways to build trust with M. Dr D should spend unstructured time getting to know M. In so doing, she can demonstrate that she is a good listener who has his best interests at heart. She should seek to understand what makes life worth living for M and what M fears most, and she should work with M on a course of care that fits with his goals and fears. This process will take time. In time, the development of trust and solidarity and continued offers of ART will give M the best chance to regain his health, to feel supported, and to live to see the day he thanks Dr D for saving his life, with respect.
References
- De Jesus M, Williams DR. The Care and Prevention in the United States Demonstration Project: a call for more focus on the social determinants of HIV/AIDS. Public Health Rep. 2018;133(2)(suppl):28S-33S.
- Birkett M, Neray B, Janulis P, Phillips G II, Mustanski B. Intersectional identities and HIV: race and ethnicity drive patterns of sexual mixing. AIDS Behav. 2019;23(6):1452-1459.
- Naar-King S, Parsons JT, Johnson AM. Motivational interviewing targeting risk reduction for people with HIV: a systematic review. Curr HIV/AIDS Rep. 2012;9(4):335-343.
- Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991-1999. Am J Public Health. 2002;92(3):371-377.
- Beyrer C, Malinowska-Sempruch K, Kamarulzaman A, Strathdee SA. 12 myths about HIV/AIDS and people who use drugs. Lancet. 2010;376(9737):208-211.
- Brincks AM, Shiu-Yee K, Metsch LR, et al. Physician mistrust, medical system mistrust, and perceived discrimination: associations with HIV care engagement and viral load. AIDS Behav. 2019;23(10):2859-2869.
- Logie C, Gadalla TM. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care. 2009;21(6):742-753.
- Bird JDP, Eversman M, Voisin DR. “You just can’t trust everybody”: the impact of sexual risk, partner type and perceived partner trustworthiness on HIV-status disclosure decisions among HIV-positive Black gay and bisexual men. Cult Health Sex. 2017;19(8):829-843.
-
Baugher AR, Beer L, Fagan JL, et al; Medical Monitoring Project. Prevalence of internalized HIV-related stigma among HIV-infected adults in care, United States, 2011-2013. AIDS Behav. 2017;21(9):2600-2608.
- Steward WT, Herek GM, Ramakrishna J, et al. HIV-related stigma: adapting a theoretical framework for use in India. Soc Sci Med. 2008;67(8):1225-1235.
- Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64(9):1823-1831.
- Kamen C, Taniguchi S, Student A, et al. The impact of denial on health-related quality of life in patients with HIV. Qual Life Res. 2012;21(8):1327-1336.
-
Horter S, Thabede Z, Dlamini V, et al. “Life is so easy on ART, once you accept it”: acceptance, denial and linkage to HIV care in Shiselweni, Swaziland. Soc Sci Med. 2017;176:52-59.
- Kelly-Hanku A, Kawage T, Vallely A, Mek A, Mathers B. Sex, violence and HIV on the inside: cultures of violence, denial, gender inequality and homophobia negatively influence the health outcomes of those in closed settings. Cult Health Sex. 2015;17(8):990-1003.
- Kalichman SC, Eaton L, Cherry C. “There is no proof that HIV causes AIDS”: AIDS denialism beliefs among people living with HIV/AIDS. J Behav Med. 2010;33(6):432-440.
- Schuster MA, Collins R, Cunningham WE, et al. Perceived discrimination in clinical care in a nationally representative sample of HIV-infected adults receiving health care. J Gen Intern Med. 2005;20(9):807-813.
-
Dang BN, Westbrook RA, Njue SM, Giordano TP. Building trust and rapport early in the new doctor-patient relationship: a longitudinal qualitative study. BMC Med Educ. 2017;17(1):32.
- Ridd M, Shaw A, Lewis G, Salisbury C. The patient-doctor relationship: a synthesis of the qualitative literature on patients’ perspectives. Br J Gen Pract. 2009;59(561):e116-e133.
-
Egger M, May M, Chêne G, et al; ART Cohort Collaboration. Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: a collaborative analysis of prospective studies. Lancet. 2002;360(9327):119-129.
- Chaiyachati KH, Ogbuoji O, Price M, Suthar AB, Negussie EK, Bärnighausen T. Interventions to improve adherence to antiretroviral therapy: a rapid systematic review. AIDS. 2014;28(suppl 2):S187-S204.