Abstract
This commentary on a case suggests why health care organizations have responsibilities to serve food to their patients, guests, and employees that is ethically, nutritionally, culturally, and religiously appropriate. This article also investigates how inclusive, equitable, sustainable food services are key dimensions of health care organizations’ civic and stewardship responsibilities to individuals and communities.
Case
NN is hospitalized due to pneumonia and eats only plant-based foods. Vegan food options are few, and NN’s nutrition has been limited to sides of vegetables, plain toast, fruit juices, and fruit salads for a few days. NN has requested more nutritionally dense foods that are easy to prepare (ie, quinoa, oatmeal, whole vegetables, whole fruits, nuts).
The organization’s dietetics administrator has apologized and explained that their food offerings are limited by their suppliers. An order has been placed for some of the items NN requested yesterday, but the supplier has reiterated that demand for meat and dairy alternatives is just too low to warrant their regular availability and delivery without the organization’s food supply costs increasing.
NN does not have anyone at the time who could bring her prepared, or even raw, plant-based foods from outside the hospital. NN’s caloric intake has been substantially reduced, despite high caloric demands of illness recovery; NN is losing weight, feels hungry, and is worried. NN asks, “I’ve requested simple items that are easy to prepare. I’d even eat some items raw. Why is this organization not able to meet my basic health nutritional needs?”
Members of NN’s clinical team wonder how to respond.
Commentary
For all hospitalized patients, proper nutrition is needed to mount an effective immune response, heal wounds, build and maintain strength, and cope with acute illness, although nutrition needs vary based on one’s acute as well as chronic health needs. The types of food required within a culture for optimal nutrition and acceptance are influenced by personal religious, moral, and other beliefs. Serving patients food that is nutritionally, culturally, religiously, and morally appropriate and acceptable to them is a critical component of providing effective, inclusive, and equitable health care services. This is a key component of patient-centered care, wherein the recipient of health care is seen as a person within their own context and the delivery of care honors dignity and autonomy during the care process.
Malnutrition—including undernutrition, overweight or obesity, and imbalances in various specific nutrients—results in increased complications, greater morbidity and mortality, longer hospital stays, higher treatment costs, more frequent readmissions, and a substantial economic burden.1,2 Conversely, treating disease-related malnutrition during a hospital stay significantly improves outcomes.3 Hospitals have ethical obligations to prevent disease and promote public health in addition to financial incentives to prevent readmissions. Indeed, prevention and health promotion in an era of epidemic chronic disease are principal obligations of most hospitals’ work. Hospitals cannot fulfill their mission to prevent disease and promote health without paying attention to individualized nutrition as well as the broader impacts of their purchasing and serving food to patients, staff, and visitors. To meet these ethical and nutritional requirements and fulfill their missions, hospitals must acknowledge individual, cultural, economic, and community and global factors.
Helping Patients Choose
A coordinated multidisciplinary approach is needed to improve nutrition care for better patient outcomes in the short- and long-term and to systemically embed culturally sensitive and individualized care into routine clinical practice. Just as clinicians have a professional obligation to guide patients to enact and practice healthy lifestyle behaviors, so the hospitals in which they work are ethically obligated to promote and facilitate healthy dietary choices by offering nutritionally balanced foods that meet the dietary needs of the diverse patients they serve.
Providing food preparers, staff, and clinicians with education and tools to offer individualized nutrition and medically appropriate—as well as culturally sensitive, desirable, delicious, and health-promoting—food options for a variety of populations is a key part of supporting patients in achieving better outcomes. For example, catering and meal service staff can facilitate patient meal selection at the bedside in accessible ways by using easy-to-understand individualized “e-menus” listing a variety of medically appropriate, healthy, and diverse food options that clearly describe the ingredients and relevant nutritional facts. Electronic bedside meal ordering systems had greater effects on patient dietary intake and satisfaction and on waste and cost reduction than traditional menus.4 Patient-centered food service, such as more informative and interactive meal-ordering systems, can be offered when medically appropriate to optimize a patient’s nutrition options.5 Engaging professional, creative, knowledgeable chefs and nutrition professionals who can guide the adjustment of recipes and educate food preparers about healthy ways to adapt food preparation by cooking from scratch with whole food-focused ingredients and healthy food preparation techniques (eg, baking instead of deep frying) would allow hospitals to provide more desirable, palatable, and familiar foods using healthier cooking methods, thereby satisfying patients’ health requirements in an enjoyable and comforting way.6
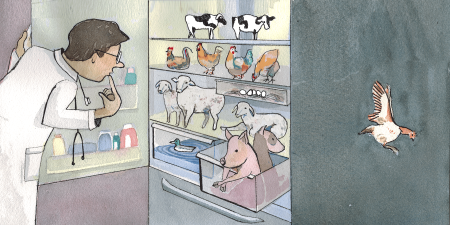
Heath organizations have ethical obligations to promote public health sourcing high-quality food.
In sum, patients’ food choices can be individualized to best meet their health and nutritional needs while respecting their autonomy by taking a team-based approach that integrates input from the patient, physicians, nutrition and culinary professionals, and other relevant providers during the acute stay, discharge process, and follow-up care.5 This collaborative and educational approach would ensure that patients have proper nutrition to aid acute recovery as well as follow-up nutrition care in the community to enhance long-term healing, management of chronic disease, and prevention of readmission.7 A patient-centered culinary medicine approach teaches patients healthy food preparation methods that support consumption of desirable, health-promoting foods while considering the social, cultural, economic, and emotional meanings that patients attach to food.8
Special Diets
Plant-based. A balanced healthy diet that emphasizes plant-based foods, such as fresh fruits and vegetables, whole grains, legumes, nuts, and seeds, can reduce the risk of many chronic conditions, including hypertension, heart disease, stroke, and some cancers,9 while aligning with the ethical preferences of many Americans who identify as vegetarian or vegan.10 Hospitals that increase access to healthy foods, including plant-based foods, have seen positive results, including “improved patient satisfaction, enhanced nutrition quality, and improved community relations.”11
Not all plant-based diets are equal in terms of reduced disease risks, however. Fresh, organic, minimally processed, and sustainably grown food offers many potential health, environmental, and ethical benefits. Foods grown under free-range conditions and grown and prepared with fewer pesticides, no artificial colors or preservatives, and no routine use of hormones and antibiotics offer health benefits for farm workers, animals, the environment, and consumers.12 Moreover, organic regenerative farming maintains biodiversity and healthy soil that is more resistant to the impacts of climate change while reducing greenhouse gas emissions, chemical runoff into water supplies, and the risk of pathogen contamination.12 Organically grown produce also has lower concentrations of pesticides and heavy metals and may have greater concentrations of essential nutrients, such as antioxidants and some vitamins and minerals.12 Therefore, hospitals have an ethical obligation to promote public health by sourcing the highest-quality food—including organic, ethically produced, and minimally processed food options—whenever possible.12
Other diets. Patient-centered care should also accommodate conditions—such as celiac disease, diabetes, allergies, lactose intolerance, pancreatic insufficiency, cardiovascular disease, kidney and liver issues, and other health conditions—that affect patients’ nutritional needs. Studies suggest that many inpatient settings are not meeting the nutrient needs of patients who require therapeutic diets, including those with food allergies.13 Food allergies and cross-contamination of foods like gluten for patients with celiac disease can also result in significant adverse health outcomes, such as anaphylaxis and acute worsening of disease.14 While some hospitals use systems like wristbands to convey significant food allergies,15 many people who contribute to ordering, preparing, and delivering food are not trained to—and fail to—communicate about food allergies and specialized dietary needs, leading to patients’ accidental allergen exposure.14 Technological tools that help alert team members to allergies at each stage of the food provision process, as well as training and clear communication, can help keep patients safe and better ensure adequate nutrition choices to keep patients healthy.15 Integrating a patient-centered approach as an organizational philosophy, as opposed to a task-focused model wherein the patient is a passive recipient of health care, is a key component of providing ethical and effective care and facilitating more effective communication,16 both of which are relevant to the provision of safe and appropriate nutrition. Furthermore, hospital food services are a tangible point of outreach to the community and significantly impact the public’s assessment of healthy nutrition.17
Cultural Considerations
Equitable, quality health care must be offered without discrimination regardless of a patient’s religion, culture, or ethnicity.18 Serving food that is unacceptable for health requirements or for moral, cultural, or religious reasons can exacerbate the discomfort of illness or hospitalization. The provision of equal care to all patients therefore requires that hospitals adjust the types and preparation of foods offered to patients in a manner that is sensitive to moral, health, cultural, and religious context.19
Food and dietary practices are often a key part of one’s cultural identity; taste and palates are trained and influenced by cultural, moral, and religious factors.19,20 Providing culturally sensitive health care, including serving food that is acceptable according to an individual’s cultural and religious mores, is important for establishing trust between patients and health care professionals, for respecting individual autonomy,19 and for helping patients feel they are respected and treated with dignity. Patients’ distrust of the preparation and type of food served can lead to additional distress, worry, and insufficient nutritional intake that may subsequently contribute to poorer outcomes and patient satisfaction.19 Therefore, collecting information about food habits and religious, cultural, or moral taboos from each individual should be standard upon nonemergency admission, and culturally inclusive menus should be offered that provide food options that align with patients’ cultural, religious, and moral preferences.
Economic Argument
Public and private institutions, including hospitals, spend billions of dollars each year on food.21 Although an institution must remain fiscally solvent to fulfill its mission in the long term, its business practices should not come into conflict with its broader mission to promote health. Hospitals must balance the logistical and economic constraints associated with feeding large numbers of people every day by respecting conventional supply chain norms of efficiency, standardization, and affordability while ensuring environmental stewardship and social equity.22 While plant-based food options may be perceived as more expensive, studies have shown that a meal plan focused on simple shelf-stable, plant-based options with olive oil can be significantly less expensive than a meal plan focusing on MyPlate guidelines that include lean animal protein, dairy, and canola oil,23 with a vegetarian diet potentially resulting in approximately $580 per year in savings.23,24 Importantly, one hospital system found that the cost of vegetarian meals was roughly half that of meat-based meals.25
Paying attention to proper nutrition more generally is fiscally responsible. There are tremendous costs, financially and ethically, in ignoring the provision of healthy, delicious, and individualized food and in failing to prevent chronic disease. Malnutrition in hospitalized patients results in poorer outcomes, slower recovery, a greater chance of readmission, and a substantial economic burden.1,2 For example, the cost of acute care for a malnourished patient is approximately $2000 more than for a well-nourished patient.26 In terms of chronic disease prevention, a 1% reduction in dietary-related health risks—such as elevated weight, blood pressure, glucose, and cholesterol levels—would save $83 to $103 per person per year in medical costs.27
Local and Global Impacts
In addition to having significant purchasing power, institutional food services use many natural and human resources and generate substantial waste, making them key players in the larger food system. Health care institutions have an ethical obligation to use their role and money to promote health and resilience in their communities and to mitigate larger inequities by embracing their responsibility to address social, economic, and physical determinants of health.28 Sustainable hospital food options thus must consider health and environmental impacts on a local and global level.
One emerging solution for hospitals to balance economics, supply chain impacts, environmental stewardship, and social equity in an ethical manner is the development of hospital gardens and farms. For example, St Luke’s University Health Network has partnered with a local nonprofit, Rodale Institute, to develop a farm on acreage surrounding one of its health campuses that yields thousands of pounds of produce each year that is served at all 10 of its hospitals.29 Similarly, Boston Medical Center produces as much as 3 tons of produce annually on a 2658 sq ft modular rooftop growing space to serve 1800 meals daily,30 support an on-site teaching kitchen, and donate free vegetables to patients with low incomes in the community.31
Health care institutions can also use their purchasing power to support their local communities. Working with local vendors to purchase ingredients that align with different ethnic and cultural traditions provides economic support to the community while procuring more culturally inclusive meals for the communities served and employed by the institution.
Conclusion
Hospitals and the food they provide have immense impact, and therefore hospitals have immense responsibilities. Hospitals should remain cognizant of how their food offerings affect patients, employees, their mission, and the planet. A global shift in dietary habits towards plant-based diets has both health and sustainability benefits. Providing appropriate and health-promoting dietary options is beneficial to patient health, necessary to respect patient dignity and provide person-centered care, and a way for hospitals to exercise institutional power in service of ecological sustainability.
References
- Agarwal E, Ferguson M, Banks M, et al. Malnutrition and poor food intake are associated with prolonged hospital stay, frequent readmissions, and greater in-hospital mortality: results from the Nutrition Care Day Survey 2010. Clin Nutr. 2013;32(5):737-745.
- Curtis LJ, Bernier P, Jeejeebhoy K, et al. Costs of hospital malnutrition. Clin Nutr. 2017;36(5):1391-1396.
- Sriram K, Sulo S, VanDerBosch G, et al. A comprehensive nutrition-focused quality improvement program reduces 30-day readmissions and length of stay in hospitalized patients. J Parenter Enteral Nutr. 2017;41(3):384-391.
- MacKenzie-Shalders K, Maunder K, So D, Norris R, McCray S. Impact of electronic bedside meal ordering systems on dietary intake, patient satisfaction, plate waste and costs: a systematic literature review. Nutr Diet. 2020;77(1):103-111.
-
Osman NS, Mor NM, Sharif MSM, Hamid SBA, Rahamat S. Hospital food service strategies to improve food intakes among inpatients: a systematic review. Nutrients. 2021;13(10):3649.
-
Held LE. Chefs serve hospital food that’s better for patients, employees—and the planet. Food Tank. Accessed September 18, 2022. https://foodtank.com/news/2018/08/nutritious-sustainable-hospital-food/
-
Everett W, Badaracco C, McCauley S. From hospital to home: why nutrition counts. Health Affairs Forefront. January 24, 2020. Accessed February 12, 2022. https://www.healthaffairs.org/do/10.1377/forefront.20200117.329745
- Irl B, Evert A, Fleming A, et al. Culinary medicine: advancing a framework for healthier eating to improve chronic disease management and prevention. Clin Ther. 2019;41(10):2184-2198.
- Slavin JL, Lloyd B. Health benefits of fruits and vegetables. Adv Nutr. 2012;3(4):506-516.
-
Reinhaert RJ. Snapshot: few Americans vegetarian or vegan. Gallup. August 1, 2018. Accessed February 14, 2022. https://news.gallup.com/poll/238328/snapshot-few-americans-vegetarian-vegan.aspx
- Potter-Dunlop JA, Tse AM. Dietary issues inpatients face with being vegetarian: an integrative review. Holist Nurs Pract. 2012;26(1):30-37.
- Barański M, Srednicka-Tober D, Volakakis N, et al. Higher antioxidant and lower cadmium concentrations and lower incidence of pesticide residues in organically grown crops: a systematic literature review and meta-analyses. Br J Nutr. 2014;112(5):794-811.
-
Rattray M, Desbrow B, Roberts S. Comparing nutritional requirements, provision and intakes among patients prescribed therapeutic diets in hospital: an observational study. Nutrition. 2017;39-40:50-56.
-
Harari R, Toren O, Tal Y, Ben-Porat T. Food allergy safety: a descriptive report of changing policy in a single large medical center. Isr J Health Policy Res. 2021;10(1):32.
-
Gagné C. Food allergies and hospitals: lack of training and reliable systems. Allergic Living. September 19, 2018. Accessed September 16, 2022. https://www.allergicliving.com/2018/09/19/food-allergies-and-hospitals-a-lack-of-training-and-reliable-systems/
-
Tomaselli G, Buttigieg SC, Rosano A, Cassar M, Grima G. Person-centered care from a relational ethics perspective for the delivery of high quality and safe healthcare: a scoping review. Front Public Health. 2020;8:44.
- Sahud HB, Binns HJ, Meadow WL, Tanz RR. Marketing fast food: impact of fast food restaurants in children’s hospitals. Pediatrics. 2006;118(6):2290-2297.
-
Office of the United Nations High Commissioner for Human Rights. The right to health. World Health Organization; 2008. Accessed February 14, 2022. https://www.ohchr.org/sites/default/files/Documents/Publications/Factsheet31.pdf
- Alpers LM. Hospital food: when nurses’ and ethnic minority patients’ understanding of Islamic dietary needs differ. Nurs Open. 2019;6(4):1455-1463.
-
Helman CG. Culture, Health and Illness. 5th ed. Hodder Arnold; 2007.
-
MarketsandMarkets. US healthcare/hospital food services market worth $22.8 billion by 2026. Cision PR Newswire. March 30, 2022. Accessed November 8, 2022. https://www.prnewswire.com/news-releases/us-healthcare-hospital-food-services-market-worth-22-8-billion-by-2026--exclusive-report-by-marketsandmarkets-301513863.html
-
Klein K. Values-based food procurement in hospitals: the role of health care group purchasing organizations. Agric Human Values. 2015;32:635-648.
- Flynn M, Schiff A. Economical healthy diets (2012): including lean animal protein costs more than using extra virgin olive oil. J Hunger Environ Nutr. 2015;10(4):467-482.
-
Green H. Mediterranean diet most affordable when shopping online. Healio. May 29, 2018. Accessed November 30, 2022. https://www.healio.com/news/endocrinology/20180529/vegetarian-diet-most-affordable-when-shopping-online
- Storz MA. Should plant-based hospital meals be the law? An American experience. Hosp Pract. 1995;48(5):241-243.
- Curtis LJ, Bernier P, Jeejeebhoy K, et al. Costs of hospital malnutrition. Clin Nutr. 2017;36(5):1391-1396.
- Henke RM, Carls GS, Short ME, et al. The relationship between health risks and health and productivity costs among employees at Pepsi Bottling Group. J Occup Environ Med. 2010;52(5):519-527.
- Willett W, Rockström J, Loken B, et al. Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet. 2019;393(10170):447-492.
-
St Luke’s Rodale Institute organic farm. Rodale Institute. Accessed February 18, 2022. https://rodaleinstitute.org/about/facilities-and-campuses/st-lukes-rodale-institute-organic-farm/
-
Vega Moreno A. Food access and education take root in hospital farms. HealthCity. August 27, 2019. Accessed November 8, 2022. https://healthcity.bmc.org/population-health/food-access-and-education-take-root-hospital-farms
-
Rooftop farm. Boston Medical Center. Accessed February 18, 2022. https://www.bmc.org/nourishing-our-community/rooftop-farm