Abstract
Physicians, pharmacists, and other health professionals play an important role in addressing social determinants of health and health disparities. Pharmacists have been addressing social determinants of health for years in all populations that experience health disparities by working as vital members of their communities and interacting on a regular basis with patients. The case presented in this article highlights social determinants’ roles in health outcomes and how pharmacists contribute to improving them. In collaboration, pharmacists and physicians can help reduce costs and optimize health outcomes.
Case
AJ is an uninsured 85-year-old man with limited English-language proficiency who has a long-standing history of type 2 diabetes, hypertension, obesity, and nonadherence to medications. AJ is a patient at a federally qualified health center (FQHC), and he has been referred by his physician to the pharmacist (ML) to assist him in managing his chronic medical conditions. ML practices in the FQHC clinic as part of an interprofessional team that consists of physicians, nurse practitioners, physician assistants, medical assistants, and dietitians. ML works under a collaborative practice agreement (CPA) with the physician, which allows her an expanded scope of practice to initiate, modify, and discontinue medication therapy under the terms of the agreement.1 During AJ’s visit, ML reviews his chart in the FQHC’s electronic health record (EHR). ML notices that AJ’s most recent A1C—a measure of a patient’s average blood sugar levels over 3 months—is 11%, indicating that AJ’s current medications are either not being taken or, if being taken, are not controlling his diabetes. ML also notices that AJ has more than one angiotensin-converting-enzyme (ACE) inhibitor prescription. Duplicate use of ACE inhibitors occurs in about 5% of elderly patients and often suggests poor communication among clinicians managing a patient’s prescriptions.2 AJ also informs ML that he had been underdosing his insulin to try to make his supply last longer and admits that he has not kept his recommended dental appointment because he has been saving money for food and bus fare. He inquires how much his new prescriptions will cost.
Commentary
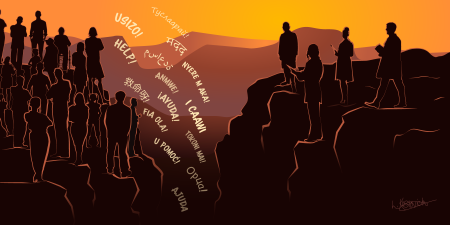
The patient in this case is experiencing several classic health effects of social determinants of health (SDOH), or the conditions in which people are born, develop, live, work, and age that can significantly affect health (see Figure 1).3 In particular, AJ has food insecurity, limited access to health care services, limited health literacy, a language barrier, and a lack of social support—all of which are routinely seen by pharmacists.
Figure 1. Social Determinants of Health

Adapted from US Department of Health and Human Services.4
Pharmacists encounter scenarios like AJ’s on a regular basis and are equipped with the knowledge and skills to assist in addressing these barriers. Although pharmacists are typically associated with community pharmacies, many pharmacists work in physician offices, clinics, hospitals, long-term care, and other settings (see Table).
| Academia | ||||||
Community-based practice
|
||||||
Health system pharmacy
|
||||||
| Long-term care facility | ||||||
| Managed care organization | ||||||
| Pharmacy benefit management organization | ||||||
| Nuclear pharmacy | ||||||
| Government/federal pharmacy | ||||||
| Pharmacy law/regulatory affairs/public policy | ||||||
| Contract research organization | ||||||
Management
|
||||||
| Medical communication/drug information centers | ||||||
Pharmaceutical industry
|
||||||
|
||||||
In this case scenario, AJ’s physician discussed the patient’s case with ML prior to the scheduled appointment and requested that ML assist with managing his chronic conditions and optimizing his medications. Although AJ was paired with ML, a bilingual pharmacist, to facilitate communication, build trust, and manage his chronic conditions, presumably other tools, such as translation line services, were available for other team members to utilize if needed. ML comprehensively evaluated AJ’s medications for his conditions, identified areas for education, developed a care plan, and, under the established CPA, discontinued the duplicate ACE inhibitor.
Pharmacists’ Roles on a Care Team
Since AJ is uninsured, ML should direct AJ to a patient navigator to assess whether he is eligible for health insurance or a patient assistance program or qualifies for a sliding-scale fee based on his income. Because they care for uninsured and low-income patients, FQHCs are eligible for 340B pricing, which allows them to obtain medications at a significantly reduced price while passing on those discounted prices to patients. By assessing AJ’s income, the patient navigator could help him qualify for more affordable medications.
Additionally, ML could assist with social support. For example, ML could facilitate connecting AJ with community health advisors who could provide him with resources for obtaining groceries and meals for free or at a discounted price. ML could also inform AJ of the FQHC’s free transportation services and how to arrange transportation for his medical and dental appointments with the help of the medical assistant.
ML could then have a brief conversation with the physician to discuss a behavioral health services referral to help AJ manage his stress. All interventions performed at this visit by the different team members, including ML, would be documented in the EHR to facilitate continuity of care and monitor patient outcomes. Imagine that at his 3-month follow-up, AJ’s A1C level decreased to 9.7% (the goal being less than 9%6) as a result of appropriate medication use, significant lifestyle changes, and access to care.
Pharmacists’ involvement in clinical preventive services, chronic disease state management, and transitions of care is vital to the elimination of health disparities.
This case demonstrates the benefits of leveraging various health care professionals to address SDOH. Understanding and tackling patients’ barriers to care beyond the clinical aspects can have a significant impact on their overall health outcomes. The health care practitioners in this case integrated SDOH assessment into clinical care and leveraged the expertise of various health care practitioners and community resources to overcome AJ’s barriers to accessing care.
Addressing Health Disparities Collaboratively
The United States invests more in its health care system than many other countries, yet disparities in health care persist, leading to unnecessary morbidity and mortality across numerous communities.7,8,9 Such disparities in health outcomes among segments of the population—categorized by race or ethnicity, sexual identity, age, disability, socioeconomic status, or geographic location, for example—are exacerbated by SDOH, resulting in lack of equity in health care.10,11 Several programs have developed goals and toolkits to achieve health equity, eliminate disparities, and improve the health of all Americans.12,13,14,15 Pharmacists have been addressing SDOH for years in all populations that experience health disparities, working as vital members of their communities by interacting daily with patients in the community—not only in specialty and community pharmacies, but also in integrated health delivery networks, managed care and community-based settings, health care clinics and physician offices, and hospitals.16,17
Pharmacists, who have earned a doctor of pharmacy degree (PharmD), identify and address health care needs by consistently applying the steps of the Pharmacists’ Patient Care Process (see Figure 2).18 This care process is not limited to clinical services, as it includes consideration of patient lifestyle, preferences, beliefs, functional goals, and socioeconomic factors. In addition, patients’ health and functional status, risk factors, health data, cultural background, health literacy, and access to medications are assessed in order to develop a patient-centered care plan. Pharmacists consistently apply this process regardless of their practice setting or specialty.
Figure 2. Pharmacists’ Patient Care Process

Reproduced with permission of the Joint Commission of Pharmacy Practitioners.18
Pharmacists’ scope of practice can be expanded in 48 states and the District of Columbia through CPAs with physicians that enhance patients’ access to coordinated care.1 CPAs vary by state, but common functions physicians delegate to pharmacists include initiating, modifying, or discontinuing drug therapy and ordering, interpreting, and monitoring laboratory tests. A US Public Health Service report to the US Surgeon General provides evidential support for comprehensive pharmacists’ patient care services.19 Through their medication and health expertise, pharmacists can provide chronic condition management, comprehensive medication management, and medication reconciliation and assessment; help with medication cost reduction; assist in formulary navigation; and facilitate home medication delivery and visits, among many other services.20,21,22,23,24,25
Health and wellness promotion areas in which pharmacists work with underserved populations include participating in wellness screening programs, promoting self-care, conducting tobacco cessation interventions, providing preconception care services, and administering vaccines.26,27,28,29 These initiatives improve the lives of community members, including in medically underserved areas, and help address major health disparities. American Public Health Association policy recognized the role of pharmacists in public health in 2006.30
Health Disparities Through a Pharmacist’s Eyes
Health professionals are at the forefront of bridging health disparities and can have a direct role in achieving this goal by integrating assessments of SDOH with interventions in clinical practice, all while providing clinical preventive services that address tobacco and substance use disorder, nutrition, physical activity, and obesity and optimize mental, oral, and sexual health.9,31 In its STEPS Forward initiative, the American Medical Association supports regarding pharmacists as integral members of the health care team due to their expertise in pharmacotherapy and their accessibility.32 Pharmacists, 55% of whom work in a community-based setting,33 are ideally positioned to address gaps in care by collaborating with other members of the health care team. For example, a community health center in Minnesota found that, after integrating a pharmacist into the clinic team, the percentage of patients, both English speaking and non-English speaking, who achieved the desired drug therapy outcomes improved by 24%.34 In addition, pharmacists can assist physicians with chronic disease management. Chronic diseases, such as diabetes, hypertension, dyslipidemia, and obesity, affect 60% of Americans, account for 37% of office-based physician visits, and continue to be on the rise.35,36 Minorities and underserved communities are disproportionally affected by these chronic diseases, one potential explanation being the association between these diseases and disparities in nutrition, access to walkable communities, and tobacco marketing.37,38 In a year-long study of patients with diabetes, 56.3% of African Americans who received medication therapy management services from a pharmacist significantly improved their diabetes compared to 22.7% in the control group.21 Pharmacists involved in transitions of care can also help patients safely transition after a hospitalization and avoid inpatient readmissions or emergency department visits within 30 days of discharge by managing medications and educating patients.39 Therefore, pharmacists’ involvement in clinical preventive services, chronic disease state management, and transitions of care is vital to the elimination of health disparities.
With the growing shift from fee-for-service models to value-based models, pharmacists can work hand-in-hand with other health care clinicians to meet health outcomes and cost metrics.40 Many required measures in value-based programs, such as the measures of the National Committee for Quality Assurance, the Healthcare Effectiveness Data and Information Set, and the Pharmacy Quality Alliance, involve optimal use of medications. For example, a large trial focused on the collaboration between physicians and pharmacists in managing blood pressure showed that individuals assigned to a team that included a pharmacist were more likely to have a meaningful reduction in blood pressure.20 A study published in 2019 reinforced these results by showing that pharmacists, in partnership with community barbers and local physicians, were able to improve blood pressure in 94% of the African-American men who visited barbershops and were seen by a pharmacist compared to 29% of those who visited barbershops and were encouraged to follow up with clinicians but did not see a pharmacist.41 By working together, pharmacists and physicians can help optimize health outcomes for vulnerable patients in communities.
Conclusion
Tackling health disparities requires a team-based, multidisciplinary approach. The case illustrated in this article, as well as the evidence provided, emphasizes the role of pharmacists in areas such as chronic disease management and prevention, medication management, health and wellness, and patient advocacy. Although pharmacists, physicians, and other clinicians could address health disparities separately, it is through a collaborative effort that the health care system will become more efficient in addressing health disparities and meeting the goals set by the federal government to improve the health of all Americans.
References
-
US Department of Health and Human Services. Advancing team-based care through collaborative practice agreements: a resource and implementation guide for adding pharmacists to the care team. Centers for Disease Control and Prevention; 2017. Accessed June 30, 2020. https://www.cdc.gov/dhdsp/pubs/docs/CPA-Team-Based-Care.pdf
- Rajska-Neumann A, Wieczorowska-Tobis K, Schulz M, Breborowicz A, Grzeskowiak E, Oreopoulos DG. Duplicate use of angiotesin-converting enzyme (ACE) inhibitors in a community-dwelling elderly population in Poland. Arch Gerontol Geriatr. 2007;44(suppl 1):295-301.
-
NCHHSTP social determinants of health. Centers for Disease Control and Prevention. Reviewed December 19, 2019. Accessed June 30, 2020. https://www.cdc.gov/nchhstp/socialdeterminants/index.html
-
Disparities. Healthy People, Office of Disease Prevention and Health Promotion, US Department of Health and Human Services. Accessed September 15, 2020. https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities
-
Career option profiles. American Pharmacists Association. Accessed August 20, 2020. https://www.pharmacist.com/career-option-profiles
-
Diabetes and health centers. Health Resources and Services Administration. Accessed August 23, 2020. https://bphc.hrsa.gov/qualityimprovement/clinicalquality/diabetes.html
-
Schneider EC, Sarnak DO, Squires D, Shah A. Mirror, mirror 2017: international comparison reflects flaws and opportunities for better US health care. Commonwealth Fund; July 2017. Accessed December 9, 2020. https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_fund_report_2017_jul_schneider_mirror_mirror_2017.pdf
-
Maloney LR, Thompson KK, Vanderpool HK. ASHP’s role in eliminating health disparities. Am J Health Syst Pharm. 2005;62(18):1871.
-
Baciu A, Negussie Y, Geller A, et al, eds; National Academies of Sciences, Engineering, and Medicine. The state of health disparities in the United States. In: Communities in Action: Pathways to Health Equity. National Academies Press; 2017:chap 2.
-
Truman BI, Smith KC, Roy K, et al; Centers for Disease Control and Prevention. Rationale for regular reporting on health disparities and inequalities—United States. MMWR Suppl. 2011;60(1):3-10.
-
Carter-Pokras O, Baquet C. What is a “health disparity”? Public Health Rep. 2002;117(5):426-434.
-
Disparities. US Department of Health and Human Services. Accessed June 30, 2020. https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities
-
Reducing disparities in health care. American Medical Association. Accessed August 23, 2020. https://www.ama-assn.org/delivering-care/patient-support-advocacy/reducing-disparities-health-care
-
Attaining health equity. Centers for Disease Control and Prevention. Accessed August 23, 2020. https://www.cdc.gov/nccdphp/dch/programs/healthycommunitiesprogram/overview/healthequity.htm
-
About SDOH in healthcare. Agency for Healthcare Research and Quality. Accessed August 23, 2020. https://www.ahrq.gov/sdoh/about.html
-
Nessel J. 2020 trends in pharmacy care: value-based pharmacy and social determinants of health. Pharmacy Times. January 22, 2020. Accessed December 9, 2020. https://www.pharmacytimes.com/news/2020-trends-in-pharmacy-care-value-based-pharmacy-and-social-determinants-of-health
-
Chiara A. The expanding role of pharmacists: a positive shift for health care. Commonwealth Medicine blog. March 26, 2019. Accessed October 27, 2020. https://commed.umassmed.edu/blog/2019/03/26/expanding-role-pharmacists-positive-shift-health-care
-
Joint Commission of Pharmacy Practitioners. Pharmacists’ patient care process. May 29, 2014. Accessed June 30, 2020. https://jcpp.net/wp-content/uploads/2016/03/PatientCareProcess-with-supporting-organizations.pdf
-
Pharmacist Professional Advisory Committee. Improving patient and health system outcomes through advanced pharmacy practice: a report to the US Surgeon General, 2011. Commissioned Corps of the US Public Health Service. Revised September 27, 2019. Accessed August 23, 2020. https://dcp.psc.gov/osg/pharmacy/sc_comms_sg_report.aspx
- Carter BL, Coffey CS, Ardery G, et al. Cluster-randomized trial of a physician/pharmacist collaborative model to improve blood pressure control. Circ Cardiovasc Qual Outcomes. 2015;8(3):235-243.
- Jameson JP, Baty PJ. Pharmacist collaborative management of poorly controlled diabetes mellitus: a randomized controlled trial. Am J Manag Care. 2010;16(4):250-255.
- Isetts BJ, Brummel AR, de Oliviera DR, Moen DW. Managing drug-related morbidity and mortality in a patient-centered medical home. Med Care. 2012;50(11):997-1001.
-
Santschi V, Chiolero A, Colosimo AL, et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc. 2014;3(2):e000718.
- Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and hospital mortality rates. Pharmacotherapy. 2007;27(4):482-493.
- Arnold ME, Buys L, Fullas F. Impact of pharmacist intervention in conjunction with outpatient physician follow-up visits after hospital discharge on readmission rate. Am J Health Syst Pharm. 2015;72(11)(suppl 1):S36-S42.
- Alhossan A, Kennedy A, Leal S. Outcomes of annual wellness visits provided by pharmacists in an accountable care organization associated with a federally qualified health center. Am J Health Syst Pharm. 2016;73(4):225-228.
- Dent LA, Harris KJ, Noonan CW. Randomized trial assessing the effectiveness of a pharmacist-delivered program for smoking cessation. Ann Pharmacother. 2009;43(2):194-201.
- Saba M, Diep J, Saini B, Dhippayom T. Meta-analysis of the effectiveness of smoking cessation interventions in community pharmacy. J Clin Pharm Ther. 2014;39(3):240-247.
- Bartch SM, Taitel MS, DePasse JV, et al. Epidemiologic and economic impact of pharmacies as vaccination location during an influenza epidemic. Vaccine. 2018;34(46):7054-7063.
-
The role of the pharmacist in public health. Policy No. 200614. American Public Health Association. November 8, 2006. Accessed June 30, 2020. https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2014/07/07/13/05/the-role-of-the-pharmacist-in-public-health
-
Green GR, Nze C. Language-based inequity in health care: Who is the “poor historian”? AMA J Ethics. 2017;19(3):263-271.
-
Choe HM, Standiford CJ, Brown MT. Embedding pharmacists into the practice. American Medical Association STEPS Forward. Accessed April 19, 2020. https://edhub.ama-assn.org/steps-forward/module/2702554
-
Occupational Outlook Handbook: pharmacists. US Bureau of Labor Statistics. Revised September 4, 2019. Accessed October 26, 2020. https://www.bls.gov/ooh/healthcare/pharmacists.htm#tab-3
- Westberg SM, Sorensen TD. Pharmacy-related health disparities experienced by non-English-speaking patients: impact of pharmaceutical care. J Am Pharm Assoc. 2005;45(1):48-54.
-
Buttorff C, Ruder T, Bauman M. Multiple chronic conditions in the United States. RAND Corporation; 2017. Accessed September 20, 2020. https://www.rand.org/content/dam/rand/pubs/tools/TL200/TL221/RAND_TL221.pdf
-
Ashman JJ, Rui P, Okeyode T. Characteristics of office-based physician visits 2016. Centers for Disease Control and Prevention; January 2019. NCHS data brief 331. Accessed September 20, 2020. https://www.cdc.gov/nchs/products/databriefs/db331.htm
-
US Department of Health and Human Services. National Healthcare Quality and Disparities Report, 2018. Agency for Healthcare Research and Quality; September 2019. AHRQ publication 19-0070-EF. Accessed June 30, 2020. https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/2018qdr.pdf
- Powell LM, Chaloupka FJ, Bao Y. The availability of fast-food and full-service restaurants in the United States: associations with neighborhood characteristics. Am J Prev Med. 2007;33(4)(suppl):S240-S245.
- Phatak A, Prusi R, Ward B, et al. Impact of pharmacist involvement in the transitional care of high-risk patients through medication reconciliation, medication education, and postdischarge call-backs (IPITCH Study). J Hosp Med. 2016;11(1):39-44.
-
American Pharmacists Association. Successful integration of pharmacists in accountable care organizations and medical home models: case studies. March 2020. Accessed June 30, 2020. https://www.pharmacist.com/sites/default/files/APhA_Medical_Home_ACO_Report_Final.pdf
- Victor RG, Blyler CA, Li N, et al. Sustainability of blood pressure reduction in black barbershops. Circulation. 2019;139(1):10-19.