Abstract
Law enforcement (LE) use of force (UOF) is a complex social, medical, and legal issue. In recent years, highly visible and publicized UOF incidents have sparked public outrage about racial inequity and motivated broad institutional reflection on sanctioning violence in the name of protecting communities. A public health approach to violence and to LE-UOF is required to develop 21st-century policing recommendations. Tactical emergency medical services physicians are uniquely positioned to convene and to serve as advisors, educators, and advocates to LE departments, community leaders, and public policy developers in order to improve UOF policies.
In Plato’s vision of a perfect society … the greatest amount of power is given to those called the Guardians. Only those with the most impeccable character are chosen to bear the responsibility of protecting the democracy.
Michael Nila and Stephen Covey1The … calculus [of reasonableness in use of force] must embody an allowance for the fact that police officers are often forced to make split-second decisions about the amount of force that is necessary in a particular situation.
Graham v Connor2
Guardianship
Law enforcement use of force (LE-UOF) is socially, legally, and medically complex. Public outrage about racial inequity in UOF has prompted many to question how violence, rooted deeply in foundational systems of modern US society, has been sanctioned over many years in the name of community policing, service, and protection. Ultimately, outbreaks of violence express failures in education, housing, employment, governance, and health care and underscore the importance of LE officers’ roles as guardians of human rights, peace, and order and of emergency physicians’ roles as guardians of life. Although these guardianship roles might be viewed by some as overly idealistic or even naïve in ignoring the complex historical roots and realities of policing in US communities, they are nonetheless crucial to maintaining social order: when guardians fail to live up to their oaths or are perceived to violate their core values, societies convulse.
Long-term media coverage of numerous UOF incidents exposes a lack of national professional standards, agency policies, and rigorous data collection on LE-UOF.3,4,5 Although absence of uniformity undermines LE accountability to the public, coverage of high-profile UOF incidents reveals legitimate, deep-rooted fear and suspicion of LE’s treatment of people of color and of individuals with mental health illness and drug use disorders.6,7,8,9,10
Emerging research suggests that police contact is a determinant of health inequity and a cause of early mortality among people of color.11 The LE and public health communities have distinct approaches to violence prevention and have developed unique cultures, vocabularies, and entrenched biases that impede their collaboration. To move forward, violence and LE-UOF must be approached from a unified public health standpoint with the aim of improving health outcomes,12 and tactical emergency medical services (TEMS) clinicians should help effect this change.
Violence Prevention Roles for TEMS Clinicians
TEMS developed largely within emergency medicine (EM) to respond to niche trauma care demands of high-risk, field-based situations that required experience at the intersection of LE, public health, trauma care, mental health care, and emergency medical care.13 TEMS clinicians undergo training in hot and warm zone operations, tactical movement, and crisis de-escalation tactics to manage threats to public safety in disciplined, protocol-driven ways. TEMS clinicians also play key roles in EM, as emergency departments (EDs) are the sites of care for most individuals involved in LE-UOF incidents, although many ED personnel lack specific training in the treatment or reporting of UOF injuries.14,15,16 Outside EDs, TEMS clinicians can motivate holistic, data-driven, scientifically informed approaches to LE interactions during crises and can advise agencies on how to improve UOF policies and protocols to mitigate excessive UOF and adverse outcomes.3 Here, we discuss 4 foundational roles of TEMS clinicians: advisors, conveners, educators, and advocates.
Clinicians can motivate holistic, data-driven, scientifically informed approaches to law enforcement interactions.
Advisors. TEMS physicians have earned the trust of LE officers through years of training, shared experience, community service, and aligned professional ethics (see Figure). On the basis of this trust, they can serve as critical advisors across the tactical and strategic spectrum. At the tactical level, clinicians can advise and influence real-time LE behavior concerning UOF. At the strategic level, clinicians’ diverse knowledge, skills, and backgrounds enables them to provide LE leaders with guidance on training, education, quality assurance, and accountability that can improve the outcomes of LE-UOF.
Figure. Virtues in Emergency Medicine and Policinga
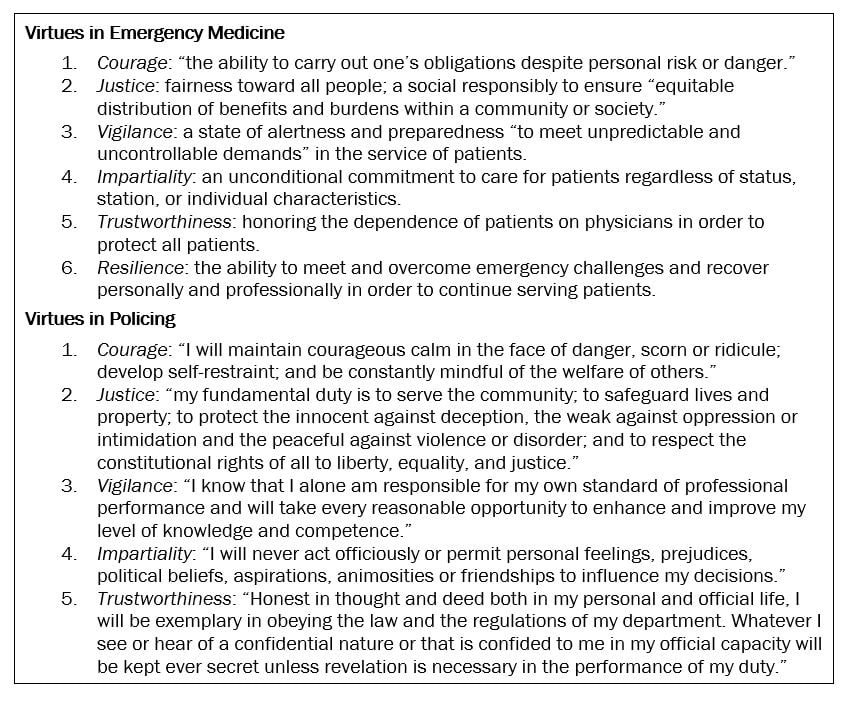
aAdapted from the American College of Emergency Physicians17 and the International Association of Chiefs of Police.18
Conveners. TEMS clinicians possess unique social capital that allows them to convene a broad network of stakeholders from LE, health systems, academia, and public health.19 Since the Napoleonic Wars, prehospital and crisis clinicians have straddled the divide between what is best for an individual patient in a clinical care situation and what is best for society from a public health perspective.20,21 The modern TEMS physician is comfortable with this tension and experienced in solving complex problems by mobilizing experts across a broad professional network. With a view to innovating public policy on UOF, TEMS physicians can bring together national medical societies (eg, the American College of Emergency Physicians, the National Association of EMS Physicians, the American College of Surgeons, the American Public Health Association, and the American Medical Association) and LE organizations (eg, the International Association of Chiefs of Police, the Major Cities Chiefs Association, and the National Tactical Officers Association), as they did with the implementation of tactical emergency casualty care as a national standard for trauma care in high-threat environments.22,23
Educators. TEMS physicians have years of education in anatomy, physiology, biology, and chemistry in addition to clinical experience managing patients with mental health problems and drug toxicity.24,25 They can leverage decades of diverse experience in adult learning to create, implement, and sustain best practices for UOF. As clinicians, many TEMS physicians have experience caring for patients with delirium and agitation, exceptional pain tolerance, and incoherent delusions, and they understand the risk of positional asphyxiation to the prone patient.26,27 Consequently, TEMS clinicians are uniquely suited to educate LE officers on the physiologic consequences of various UOF modalities (eg, chemical agents, nonlethal electric shock weapons, physical restraints). TEMS clinicians are also experts at crew resource management (CRM). In the ED, integrated team care for trauma and for cardiopulmonary resuscitation during cardiac arrest demonstrate the value of CRM.28 Applying these clinically validated CRM tactics during UOF incidents can optimize de-escalation techniques, medication delivery, patient monitoring, and the use and position of restraints. Combined with clear identification of roles and responsibilities during team responses, education on these tactics could mitigate adverse outcomes, UOF incidents, and in-custody deaths.
Advocates. Although advocacy is a core tenet of the physician’s professional ethos, it is not a simple task in the context of UOF. In seeking to shape UOF policies, TEMS clinicians should advocate for a data-driven, public health approaches to UOF policies and management of complex, high-threat interactions.29,30,31 The President’s Task Force on 21st Century Policing details 3 relevant advocacy priorities.32
- Create standards of care for UOF. At the departmental level, TEMS clinicians can demonstrate to LE agencies the importance of crafting, validating, and implementing quality assurance processes to codify such standards. And, at a national level, TEMS clinicians can try to unite professional societies in health professions, law, public health, and public policy to help generate resources to match this requirement.
- Require and fund crisis response training. Just as clinicians would not introduce a new airway device in EM practice without robust training and budget allocation, so TEMS physicians must advocate at all levels for funding for expanding and developing LEO training in UOF and crisis mitigation.
- Study outcomes. Advocacy efforts should demand accurate data collection to inform public policy, develop departmental processes, craft realistic training, and support a public health approach to violence reduction.32,33
Models of Success
There is evidence that TEMS clinicians are increasingly influencing UOF policies across the United States, as leaders search for solutions to the complex issues of violence, LE use of force, and community security. In Champaign, Illinois, LE now successfully utilize a multidisciplinary behavioral health response team to reduce UOF incidents when engaging with individuals with mental illnesses and substance use disorders.34,35 In Dallas, LE worked with TEMS clinicians to develop the Rapid Integrated Group Healthcare Team (RIGHT)—comprising paramedics, licensed clinical social workers, and police officers—to more effectively manage mental illnesses and substance use disorders when responding to calls about people in crisis.36 Dallas is also addressing UOF incidents through the novel ABLE (Active Bystandership for Law Enforcement) Project,37 a national resource for training, technical assistance, and research to nourish LE cultures in which officers intervene to prevent misconduct, avoid mistakes by police, and promote officer health and wellness.37,38
LE-UOF will continue to be required in certain situations. However, we can and must do better. Reducing violence, criminal or sanctioned, is a whole-community challenge that requires a whole-community set of solutions. Within the house of medicine, TEMS physicians stand at the ready to serve as trusted advisors, conveners, educators, and advocates. In these roles, they can truly help guide a diverse public health coalition to ensure that data, training, focused funding, and accountability drive efforts aimed at the most judicious and just UOF.
References
-
Nila M, Covey SR. The Nobility of Policing. Franklin Quest; 2008.
-
Graham v Connor, 490 US 386 (1989).
-
Alpert G, Dunham RG. Understanding Police Use of Force: Officers, Suspects, and Reciprocity. Cambridge University Press; 2004.
-
The use-of-force continuum. National Institute of Justice. August 3, 2009. Accessed March 19, 2021. https://nij.ojp.gov/topics/articles/use-force-continuum
-
National use-of-force data collection. Federal Bureau of Investigation. Accessed March 18, 2021. https://www.fbi.gov/services/cjis/ucr/use-of-force
- Gilbert K, Ray R. Why police kill Black males with impunity: applying public health critical race praxis (PHCRP) to address the determinants of policing behaviors and “justifiable” homicides in the USA. J Urban Health. 2015;93(suppl 1):122-140.
- Strote J, Hickman M. The relationship of injury and complaints of police use of excessive force. Am J Forensic Med Pathol. 2020;41(1):5-10.
- Strauss G, Glenn M, Reddi P, et al. Psychiatric disposition of patients brought in by crisis intervention team police officers. Community Ment Health J. 2005;41(2):223-228.
- Compton M, Demir Neubert B, Broussard B, McGriff J, Morgan R, Oliva J. Use of force preferences and perceived effectiveness of actions among Crisis Intervention Team (CIT) police officers and non-CIT officers in an escalating psychiatric crisis involving a subject with schizophrenia. Schizophr Bull. 2009;37(4):737-745.
- Watson A, Swartz J, Bohrman C, Kriegel L, Draine J. . Understanding how police officers think about mental/emotional disturbance calls. Int J Law Psychiatry. 2014;37(4):351-358.
- Bui A, Coates M, Matthay E. Years of life lost due to encounters with law enforcement in the USA, 2015-2016. J Epidemiol Community Health. 2017;72(8):715-718.
- Shepherd J, Sumner S. Policing and public health—strategies for collaboration. JAMA. 2017;317(15):1525-1526.
-
What is tactical medicine? American College of Emergency Physicians. Accessed March 19, 2021. https://www.acep.org/tacticalem/about-us/what-is-tactical-medicine/
- Hutson H, Anglin D, Rice P, Kyriacou D, Guirguis M, Strote J. Excessive use of force by police: a survey of academic emergency physicians. Emerg Med J. 2009;26(1):20-22.
-
Pearce JD. Not just for SWAT teams: the importance of training officers in tactical emergency medicine. Police Chief Mag. April 2015. Accessed March 19, 2021. https://www.policechiefmagazine.org/not-just-for-swat-teams-the-importance-of-training-officers-in-tactical-emergency-medicine/
-
Hardy J, Mehkri F. Protecting the protectors: physician roles in tactical emergency medicine support. EM Resident. June 6, 2017. Accessed March 19, 2021. https://www.emra.org/emresident/article/protecting-the-protectors-physician-roles-in-tactical-emergency-medicine-support/
-
American College of Emergency Physicians. Code of ethics for emergency physicians. Revised January 2017. Accessed October 4, 2021. https://www.acep.org/globalassets/new-pdfs/policy-statements/code-of-ethics-for-emergency-physicians.pdf
-
Law enforcement code of ethics. International Association of Chiefs of Police. Adopted October 1957. Accessed October 4, 2021. https://www.theiacp.org/resources/law-enforcement-code-of-ethics
-
Obasogie OK, Newman Z. Police violence, use of force policies, and public health. Am J Law Med. 2017;43:279-295.
-
George A. Baron Larrey—Napoleonic inventor of ambulances, triage and MASH. Conversation. July 8, 2016. Accessed March 19, 2021. https://theconversation.com/baron-larrey-napoleonic-inventor-of-ambulances-triage-and-mash-57893
-
Hughes K. Army helicopters in Korea, 1950 to ‘53. US Army. October 28, 2016. Accessed March 19, 2021. https://www.army.mil/article/177302/army_helicopters_in_korea_1950_to_53
- Schwartz R, Lerner B, Llwewllyn C, et al. Development of a national consensus for tactical emergency medical support (TEMS) training programs—operators and medical providers. J Spec Oper Med. 2014;14(2):122-138.
- Pennardt A, Callaway DW, Kamin R, et al. Integration of tactical emergency casualty care into the national tactical emergency medical support competency domains. J Spec Oper Med. 2016;16(2):62-66.
-
Policy on emergency medicine residency training requirements. American Board of Emergency Medicine. April 2021. Accessed December 17, 2021. https://www.abem.org/public/docs/default-source/policies-faqs/em-residency-training-requirements.pdf?sfvrsn=b7b1c3f4_4#:~:text=Residents%20must%20successfully%20complete%20at,accrued%20from%20year%20to%20year
-
Board eligibility. American Board of Emergency Medicine. Accessed July 14, 2021. https://www.abem.org/public/become-certified/board-eligibility
-
Heiskell LE. How to prevent positional asphyxia. Police Mag. September 9, 2019. Accessed November 9, 2021. https://www.policemag.com/524139/how-to-prevent-positional-asphyxia
-
Grayson K. Stand up, and speak out. EMS 1. May 25, 2021. Accessed November 9, 2021. https://www.ems1.com/airway-management/articles/stand-up-and-speak-out-QD0lQusspK4sDPkN/
-
Hopkins C, Burk C, Moser S, Meersman J, Baldwin C, Youngquist S. Implementation of pit crew approach and cardiopulmonary resuscitation metrics for out-of-hospital cardiac arrest improves patient survival and neurological outcome. J Am Heart Assoc. 2016;5(1):e002892.
-
Anti-Poverty Network of New Jersey. The Uncomfortable Truth: Racism, Injustice, and Poverty in New Jersey. September 2017. Accessed March 19, 2021. https://2750d32d-03da-445f-8576-8ae3f5da7b2f.filesusr.com/ugd/14a332_1fb8d8650c844748ad81d7531652caac.pdf
-
APA urges closer partnerships between police, behavioral experts to stem racial incidents. News release. American Psychological Association; June 10, 2020. Accessed March 19, 2021. https://www.apa.org/news/press/releases/2020/06/police-partnerships
- Fellner J. Race, drugs, and law enforcement in the United States. Stanford Law Pol Rev. 2009;20(2):257-291.
-
Office of Community Oriented Policing Services. The President’s Task Force on 21st century policing: implementation guide. US Department of Justice; 2015. Accessed March 25, 2021. https://policingequity.org/images/pdfs-doc/reports/TaskForce_FinalReport_ImplementationGuide.pdf
-
Vitale AS. The End of Policing. Verso; 2017.
-
Sanders JR. Overview of the Champaign County Crisis Intervention Team. Urbana Police Department. Accessed November 9, 2021. https://urbanaillinois.us/sites/default/files/attachments/cit-presentation.pdf
-
Behavioral health response. Urbana Police Department Crisis Intervention Team. Accessed November 9, 2021. https://www.urbanaillinois.us/government/police/cit-team
-
Miller T. For mental health 911 calls, Dallas found success in social workers. D Mag. July 17, 2020. Accessed March 17, 2021. https://www.dmagazine.com/frontburner/2020/07/for-mental-health-911-calls-dallas-found-success-in-social-workers
-
Active Bystandership for Law Enforcement (ABLE) Project. Georgetown Law. Accessed November 9, 2021. https://www.law.georgetown.edu/innovative-policing-program/active-bystandership-for-law-enforcement/
-
Caruth Police Institute approved to provide ABLE training for Dallas Police Department. UNT Dallas. January 13, 2021. Accessed November 9, 2021. https://www.untdallas.edu/news/caruth-police-institute-approved-provide-able-training-dallas-police-department



