Abstract
This commentary on a case considers a transgender patient’s mental health and risk for deep vein thrombosis (DVT) in ethical decision making about feminizing gender-affirming hormone therapy (GAHT). Key considerations when beginning GAHT include recognizing that venous thromboembolism risk may only be modest and can be easily mitigated and that a transgender patient’s mental health status should not weigh in a treatment decision about hormone therapy any more than it would for someone who is not transgender. Because the DVT risk of the case patient, who has a history of smoking and DVT, will only be increased modestly if at all by estrogen therapy and can be decreased through smoking cessation along with other DVT prevention methods, the patient should receive gender-affirming hormone therapy.
Case
K is 34 years old and is transgender. They present to an endocrinology clinic to meet Dr J and, hopefully, begin desired hormone therapy. Dr J is most concerned about K’s suffering deep vein thrombosis (DVT) 3 years ago and 10-pack-per-year smoking history, especially since K is not currently on anticoagulation therapy and continues smoking. K has also seen a therapist regularly for 15 years to augment medical management of depression and anxiety.
Dr J asks K to talk more about what they hope to achieve with hormone therapy, and K responds with a list of long hoped-for changes. Dr J notes that some physical changes that K hopes for could be better achieved surgically. Dr J outlines how to mitigate K’s DVT risk, although some thromboembolism risk would remain, even with anticoagulants and smoking cessation. Dr J explains that, in order to better understand and quantify estrogen therapy risks, results of laboratory tests on K’s blood draws from today’s visit will be needed, too. K emphasizes that they would like to start hormones as soon as possible. K is eager to start anticoagulation therapy if that would make it easier for them to start hormone therapy with Dr J. Dr J also advises K to consider whether they can commit to a smoking cessation program. K schedules a follow-up appointment next week but feels daunted about quitting smoking and discouraged about not having an estrogen regimen prescribed yet.
Commentary
Dr J is tasked with managing K’s gender-affirming estrogen regimen in an ethical way. The goal is to treat K’s health risks equitably, commensurate with the care of any other patient. Dr J is concerned about minimizing K’s risk of DVT, prescribing gender-affirming hormone therapy (GAHT) safely, and providing appropriate mental health intervention when needed.
K’s medical history, including smoking and DVT history, should be the focus of treatment. K’s treatment as a transgender person should not differ from that of any other patient with a similar medical history seeking hormone therapy. Put differently, although K’s patient experience must be highlighted and valued, K’s being transgender is not likely to change their treatment regimen. If K chooses to explore other methods of gender-affirming care, such as surgery, Dr J can adjust the treatment plan to K’s long-term goals.
Assessing DVT Risk
With regard to treatment options, K’s DVT risk is an important factor to weigh, given K’s smoking history and that their prior DVT increases the likelihood of recurrent thromboembolism.1 Other factors, such as age above 35 (K is 34), weight, hypertension, and co-occurring illnesses such as HIV, must be included when assessing DVT risk.2 Since degree of the DVT risk with GAHT cannot be definitively determined, forms of estrogen that increase venous thromboembolism risk should not be prescribed.3 Regardless of K’s GAHT, Dr J must encourage K to quit smoking and to minimize DVT risk by taking therapeutic anticoagulants and wearing compression stockings.4,5,6 K’s willingness to both start anticoagulation therapy and commit to a smoking cessation program shows promise for their safe use of estrogen.
Before prescribing estrogen, clinicians must review the literature on the dosage and method of estrogen administration. Low-dose exogenous estrogens have been shown to increase risk of blood clots.7 If patients, such as K, are already at risk of DVT, they may need to take anticoagulant medications independently of their plans to take exogenous estrogen. Estrogen treatment is thus a secondary factor in assessment of K’s DVT risk, and it is critical to address the primary factor—a prior DVT—in isolation.
Although patient experience must be highlighted and valued, being transgender is not likely to change their treatment regimen.
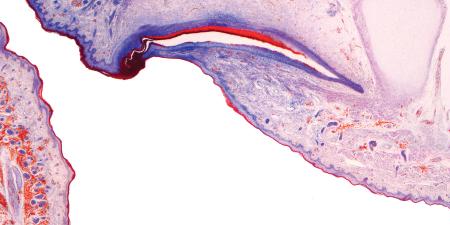
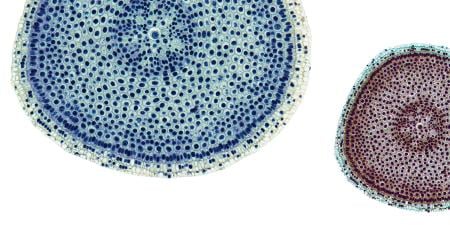
In K’s case, there are various available options for estrogen therapy that minimize the associated health risks. For example, transdermal estrogen may pose less risk for DVT than oral estrogen.8 More specifically, transdermal estrogen, unlike oral estrogen, does not increase proinflammatory cytokines and procoagulant factors in transgender women.2,9 Nevertheless, it is unclear if the lower DVT risk of transdermal estrogen is due to dosage or route of administration.3
Although research on DVT risk of estrogen therapy for transgender patients (other than individual case studies10) is sparse, oral ethinyl estradiol has been shown to be associated with venous thromboembolism in transgender women11 and should not be prescribed, as there are safer and equally effective alternatives available. Additionally, hormone therapy with a combination of lower doses of estrogen and adjunct androgen-lowering or androgen-inhibiting agents might decrease DVT risk. In Europe, cyproterone acetate and gonadotropin-releasing hormone (GnRH) agonists have been the preferred agents in conjunction with estrogen.12 In Israel, spironolactone or GnRH agonists as well as cyproterone acetate are used as estrogen adjuncts.13 An Israeli research team reported that spironolactone and GnRH do not elevate prolactin as cyproterone acetate does, suggesting that the observed elevation of prolactin in transgender women may be due to factors besides estrogen.13 Ultimately, the use of forms of estrogen other than estradiol as GAHT poses a small risk for DVT.11 By addressing K’s other health problems, their DVT risk can be further lowered. Most importantly, Dr J should inform K that knowledge of the risk of DVT with GAHT is limited in scope due to a lack of data.
Estrogen is a commonly prescribed medication; K should receive estrogen since the benefits of estrogen therapy to K’s quality of life outweigh the minimal risks. Note that, in parallel cases, a patient with ovaries and a history of DVT and tobacco use is not automatically denied hormonal birth control or menopausal hormone therapy. In fact, taking exogenous estrogens, a history of immobilization postsurgery, and other common factors have lower DVT risk than pregnancy,9 which can increase a person’s postpartum risk of venous thromboebolism 22- to 84-fold relative to women who are not pregnant or postpartum.14 It has also been shown that the DVT risk for combined oral contraceptives—the most commonly used estrogen product and one that often includes the thrombogenic estrogen, ethinyl estradiol—is lower than the DVT risk for pregnant and postpartum patients.9 While exogenous estrogen may have a non-zero risk of harm, its small risk is outweighed by its potential benefit in supporting K’s needs.
Assessing Mental Health Risk
Dr J and K’s health care team must also support K’s mental health by encouraging K’s continued therapy and consistent follow-up care in addition to GAHT. Transgender patients seeking GAHT are often labeled as suffering from gender dysphoria. Gender dysphoria is defined in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders as significant distress related to a desire to be another gender, but clinical dysphoria is not exclusive to transgender or gender diverse people.15 The eleventh version of the International Classification of Diseases signaled that gender identity-related health conditions are not mental disorders by moving the relevant categories to the chapter titled “Conditions Related to Sexual Health.”16 While K presents with a “list of long hoped-for changes” in relation to their gender identity, this detail alone does not constitute evidence of a mental health concern. Thus, it would be inappropriate to interpret K’s desire for GAHT as a desire to relieve dysphoria. Rather, the prescription of GAHT represents a patient-centered treatment that respects K’s autonomy in choosing medical care that will most benefit their health and well-being. Additionally, unless mental health complications arise that might interfere with treatment or put K at risk for mental health instability, K’s 15-years of therapy to manage depression and anxiety is not relevant to the decision to prescribe K estrogen therapy. There is no evidence to suggest that K’s use of estrogen would increase their depression and anxiety. In fact, multiple studies show that transgender people’s depression and anxiety significantly improve following GAHT,17 which could be anticipated to have a positive outcome in K’s treatment as well. In addition to regularly scheduled appointments to assess the effectiveness of GAHT, Dr J may also revisit the conversation annually to ensure that the treatment is not negatively interfering with K’s mental health.
Conclusion
K should receive GAHT with appropriate follow-up care and discussion about potential risks and outcomes. While K has important lifestyle modifications to consider, their well-being as a transgender person remains the priority. Dr J should provide updated information as it becomes available to allow for well-informed decision making with K. In addition, Dr J must approach such conversations with trauma-informed knowledge, inclusive language, and thoughtful advice on how to proceed with K’s care safely.
K’s being transgender does not mean that the risks and benefits of estrogen therapy should be assessed differently for K than for cisgender women. By educating K about minimizing their DVT risk and quitting smoking and by encouraging follow-up with a mental health professional, Dr J shows support for K, whose willingness to take anticoagulants and make lifestyle changes justifies prescribing appropriate GAHT.
References
- Hansson P, Sorbo J, Eriksson H. Recurrent venous thromboembolism after deep vein thrombosis: incidence and risk factors. Arch Intern Med. 2000;160(6):769-774.
- Heit JA. Epidemiology of venous thromboembolism. Nat Rev Cardiol. 2015;12(8):464-474.
-
Goldstein Z, Khan M, Reisman T, Safer JD. Managing the risk of venous thromboembolism in transgender adults undergoing hormone therapy. J Blood Med. 2019;10:209-216.
-
Sachdeva A, Dalton M, Amarigi SV, Lees T. Elastic compression stockings for prevention of deep vein thrombosis. Cochrane Database Syst Rev. 2010;(7):CD001484.
- Gialeraki A, Valsami S, Pittaras T, Panayiotakapoulous G, Politou M. Oral contraceptives and HRT risk of thrombosis. Clin Appl Thromb Hemost. 2018;24(2):217-225.
- Laidlaw E, Irwig MS. Risks and benefits of estrogen therapy for a male-to-female transsexual with a prothrombin gene mutation. Endocr Pract. 2013;19(6):150-153.
-
Oedingan C, Scholz S, Razum O. Systematic review and meta-analysis of the association of combined oral contraceptives on the risk of venous thromboembolism: the role of the progestogen type and estrogen dose. Thromb Res. 2018;165:68-78.
- Mohammed K, Abu Dabrh AM, Benkhadra K, et al. Oral vs transdermal estrogen therapy and vascular events: a systematic review and meta-analysis. J Clin Endocr Metab. 2015;100(11):4012-4020.
- Zucker R, Reisman T, Safer JD. Minimizing venous thromboembolism in feminizing hormone therapy: applying lessons from cisgender women and previous data. Endocr Pract. 2021;27(6):621-625.
-
Oguz SH, Buyakasik Y, Yildiz BO. Management of recurrent deep vein thrombosis in a transgender woman. J Endocr Soc. 2021;5(suppl 1):A792.
- Slack DJ, Safer JD. Cardiovascular health maintenance in aging individuals: the implications for transgender men and women on hormone therapy. Endocr Pract. 2020;27(1):63-70.
- Safer JD. Using evidence to fill gaps in the care of transgender people. Endocr Pract. 2020;26(11):1387-1388.
- Sofer Y, Yaish I, Yaron M, Yokobi M, Stern N, Greenman Y. Differential endocrine and metabolic effects of testosterone suppressive agents in transgender women. Endocr Pract. 2020;26(8):883-890.
- Jackson E, Curtis KM, Gaffield ME. Risk of venous thromboembolism during the postpartum period: a systematic review. Obstet Gynecol. 2011;117(3):691-703.
- Schulz SL. The informed consent model of transgender care: an alternative to the diagnosis of gender dysphoria. J Humanist Psychol. 2018;58(1):72-92.
-
Gender incongruence. International Classification of Diseases. Version 11. World Health Organization. Updated February 2022. Accessed January 13, 2023. https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f411470068
- T’Sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine. Endocr Rev. 2019;40(1):97-117.